Gabriel Caponetti / Wikimedia Commons
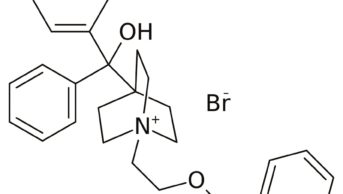
Ibrutinib, a Bruton’s tyrosine kinase inhibitor (BKI), has been launched in the UK for the treatment of adults with mantle cell lymphoma (MCL) or chronic lymphocytic leukaemia (CLL).
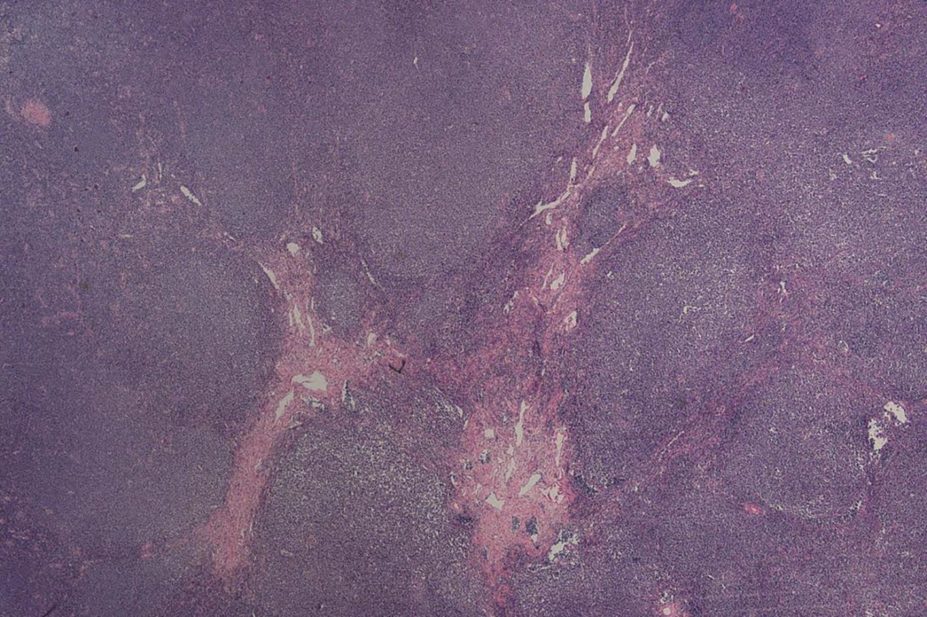
It is the first in a new class of BKI drugs, which interfere with the B-cell receptor signalling pathway. This is implicated in the pathogenesis of B-cell malignancies, including MCL, diffuse large B-cell lymphoma, follicular lymphoma, Waldenstrom’s macroglobulinaemia and CLL.
According to its summary of product characteristics, ibrutinib should be given at a dose of 560mg (four 140mg capsules) once daily when used to treat adult patients with relapsed or refractory MCL. For adults with CLL, a lower dose of 420mg (three capsules) once daily is recommended; treatment is indicated in CLL patients who have received at least one prior therapy, or first line in patients with the 17p gene deletion or TP53 mutation who are unsuitable for chemo-immunotherapy.
In clinical trials, ibrutinib significantly improved progression-free survival against its comparator ofatumumab (Arzerra) in patients with relapsed or refractory CLL — a difficult-to-treat group. Of note, patients with 17p gene deletion, who are more frequently refractory to chemotherapy and tend to be younger than the average CLL patient, did as well on ibrutinib as patients without this poor-risk genetic profile.
“Administered orally once daily compared to weekly complex infusions for up to 16 weeks for ofatumumab and with a favourable toxicity profile, ibrutinib is an attractive alternative for patients and chemotherapy units alike,” says Libby Hardy, principal pharmacist, cancer services at Royal Devon and Exeter Hospital, Exeter.
The FLAIR study is currently recruiting in the UK for treatment-naïve patients with CLL. The study is evaluating ibrutinib with rituximab against the current standard of care — fludarabine, cyclophosphamide and riruximab (FCR). “This offers particular hope for 17p-deleted patients who do disproportionately badly on FCR due to lack of wild type p53 function, an important pathway for mediating purine analogue (fludarabine) cytotoxicity,” says Hardy.
For the MCL indication, the licensing study was a single arm study with no comparator. Ibrutinib was shown to be highly active in this disease with a favourable toxicity profile compared with other, more intensive treatment options.
The most common side effects seen with ibrutinib are pneumonia, upper respiratory tract infection, thrombocytopenia and fatigue.
“Pharmacists should be alerted to the numerous potential drug interactions relating to CYP3A4 metabolism, and particularly to the danger of ibrutinib being given to patients on anticoagulants as there is already a high risk of haemorrhage with this drug,” Hardy notes.
Ibrutinib received marketing authorisation in October 2014 and will be sold under the trade name of Imbruvica by Janssen-Cilag Ltd.