Shutterstock.com
The Medicines and Healthcare products Regulatory Agency (MHRA) has backed the continued use of the thrombolytic drug alteplase for up to 4.5 hours after the onset of symptoms of acute ischaemic stroke, but say the chances of a more favourable outcome for patients are enhanced the earlier the treatment is given.
The review was set up after Roger Shinton, a former consultant physician at Birmingham Heartlands Hospital, questioned the evidence base supporting the drug in a letter to The Lancet
[1]
in 2014. He raised concerns about the initial trial[2]
used to obtain marketing approval for alteplase and a subsequent trial[3]
that was key to extending its window of use in Europe from 3.0 hours to 4.5 hours.
The MHRA appointed an expert group to review all the available evidence on alteplase, which included data from the marketing authorisation holders. The group also commissioned the Stroke Thrombolysis Trialists’ Collaborative Group (STTCG), which published a meta-analysis on alteplase in 2014[4]
, to conduct additional analyses.
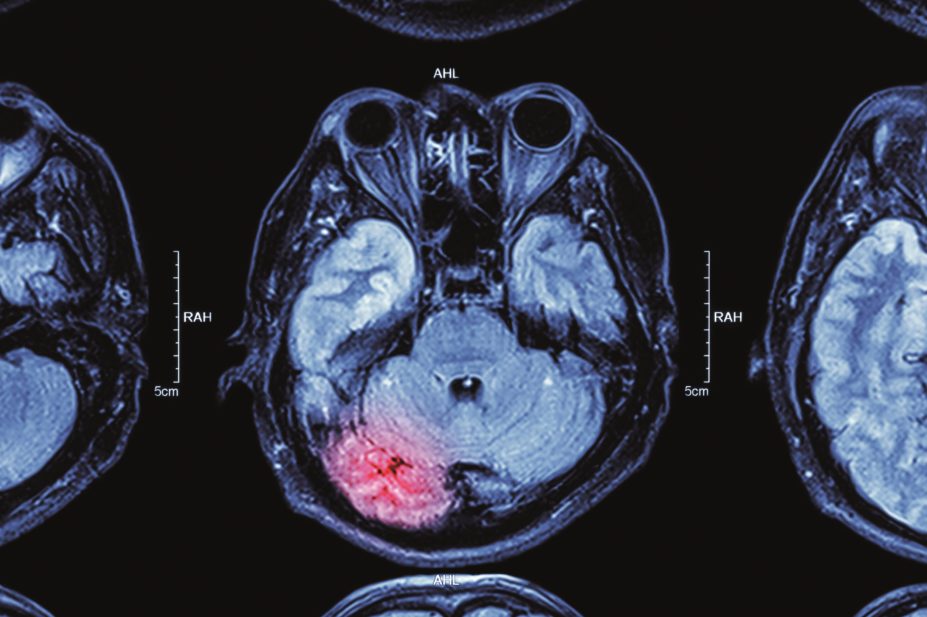
The group concluded that the benefit/risk ratio of alteplase for treatment of acute ischaemic stroke is positive when used within the terms of its licence up to 4.0 hours after onset of symptoms. There was around a 2% risk of a fatal intracranial haemorrhage in the first two days post-treatment with alteplase, but this risk was outweighed by the reduced risk of disability in surviving patients.
Sir Ian Weller, who chaired the group, explains: “The evidence shows that for every 100 patients treated with alteplase, while there is an early risk of a fatal bleed in two patients, after three to six months, around ten more patients in every 100 are disability free when treated within 3.0 hours. In addition, five more patients in every 100 are disability free when treated between 3.0 hours and 4.5 hours after a stroke.
“The conclusion of the group is very clear in that the current time frame for treatment is supported by strong evidence.”
The review also found that 11% of all stroke patients receive alteplase. The drug is used off label in 30% of cases; mostly in patients aged over 80 years (equivalent to 29% of all alteplase use). Around 2% of patients get alteplase more than 4.5 hours after symptom onset.
Speaking at a press conference in London on 23 July 2015 to announce the expert group’s conclusions, Tony Rudd, NHS England’s National Clinical Director for Stroke, said that while alteplase was not licensed for over-80s, there was evidence that this group benefitted as much as younger patients. However, he added that in this age group “it should only be used in settings where there are clinicians with experience and expertise in stroke”.
The MHRA’s director of vigilance and risk management of medicines June Raine said she expects manufacturers to apply to extend the use of alteplase to anyone aged over 80 years using data from recent STTCG analyses[4]
.
Rudd confirmed that the recommendation on use after 4.5 hours remains unchanged. “Each individual patient should be assessed on their own merits within 4.5 hours and 6.0 hours,” he said.
Shinton and other senior doctors have called for all the data on alteplase to be published. Raine said everything except pre-publication data was due to be published online on 24 July 2015, which she said was “unprecedented”. “Pre-publication data will be added as soon as that is possible,” she said.
References
[1] Shinton R. Questions about authorisation of alteplase for ischaemic stroke. Lancet 2014:384:659–660.
[2] National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. New England Journal of Medicine 1995:333:1581–1588.
[3] Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. New England Journal of Medicine 2008;359:1317–1329.
[4] Emberson J, Lees KR, Lyden P et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–1935.
You may also be interested in
Medicines commission calls for greater clarity on risk of suicidal behaviour from antidepressants

Patient safety commissioner pushes government on valproate redress almost two years after report
