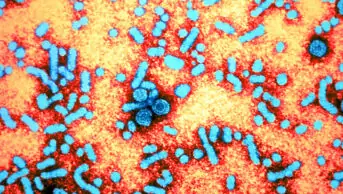
Wikimedia Commons
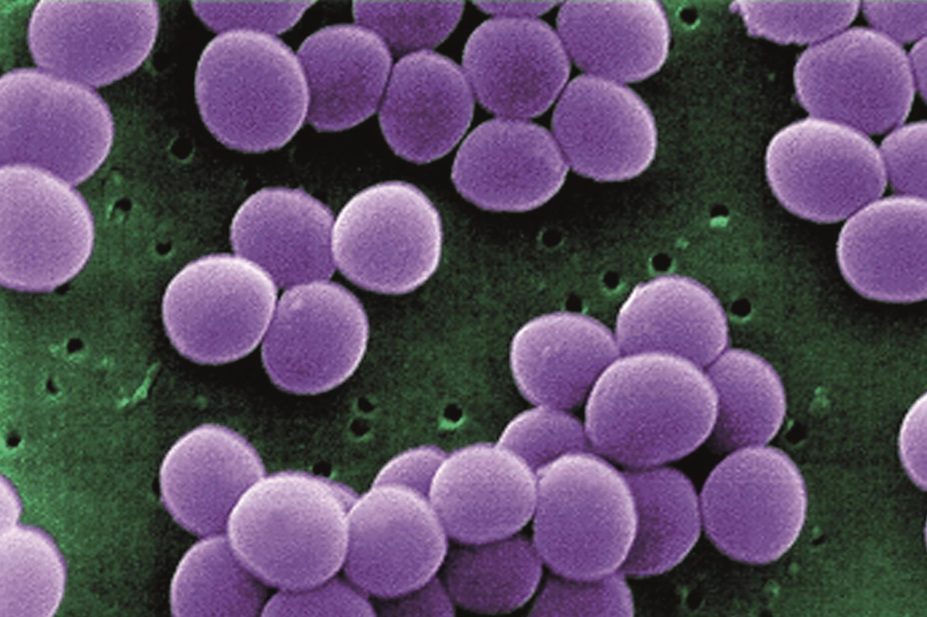
The antibiotic telavancin (Vibativ) has been made available in Europe for the treatment of adults who have contracted pneumonia in hospital, including ventilator associated pneumonia (VAP), caused by meticillin-resistant Staphylococcus aureus (MRSA).
Telavancin was approved by the European Medicines Agency in 2011. However, its marketing authorisation was suspended in 2012 before launch because the contract manufacturer did not meet the Good Manufacturing Practice requirements. There were no safety concerns with the product itself. Following transfer of production to a new contract manufacturer, the marketing suspension was lifted in early 2014 and telavancin is now available in Europe.
Telavancin, marketed by the Clinigen Group, is a lipoglycopeptide antibacterial agent, which offers a dual mechanism of action. It is the first of an innovative new class of antibiotics. In a similar way to vancomycin, telavancin binds to and prevents polymerisation of bacterial cell wall constituents, weakening and then killing the cell. Telavancin also has a second mode of action where it interacts with the cell membrane, causing depolarisation – again leading to cell death.
The dual mechanism suggests that it may be harder for bacteria to become resistant to telavancin because a strain resistant to one of the actions may still be susceptible to the other.
Telavancin is authorised for the treatment of hospital-acquired (nosocomial) pneumonia (HAP) in adults, including VAP, known or suspected to be caused by MRSA, when other treatments are not suitable. It is administered once daily by IV infusion and, unlike vancomycin, does not require therapeutic drug level monitoring.
Up to 60% of S. aureus strains are meticillin resistant, and mortality rates for HAP range from 30% to 70%. Vancomycin, linezolid and teicoplanin are currently the only other antibiotics available in Europe to treat HAP/VAP caused by MRSA and other serious Gram-positive bacterial infections.
Pooled data from two randomised controlled trials, involving more than 1,500 patients show that 7–21 days of intravenous telavancin (10mg per kg every 24 hours) produces similar cure rates to IV vancomycin (1g every 12 hours) in patients with hospital-acquired pneumonia suspected to be caused by Gram-positive pathogens. Cure rates with telavancin were 58.9% at 7–14 days after the end of treatment and 59.5% with vancomycin.
The most commonly reported side-effects of telavancin in trials include fungal infection, insomnia, disturbances of taste, headache, constipation, diarrhoea, vomiting, pruritus, rash, acute renal failure, foamy urine, fatigue and chills. Raised blood levels of creatinine and the liver enzymes alanine aminotransferase and aspartate aminotransferase were also recorded.