Shutterstock.com
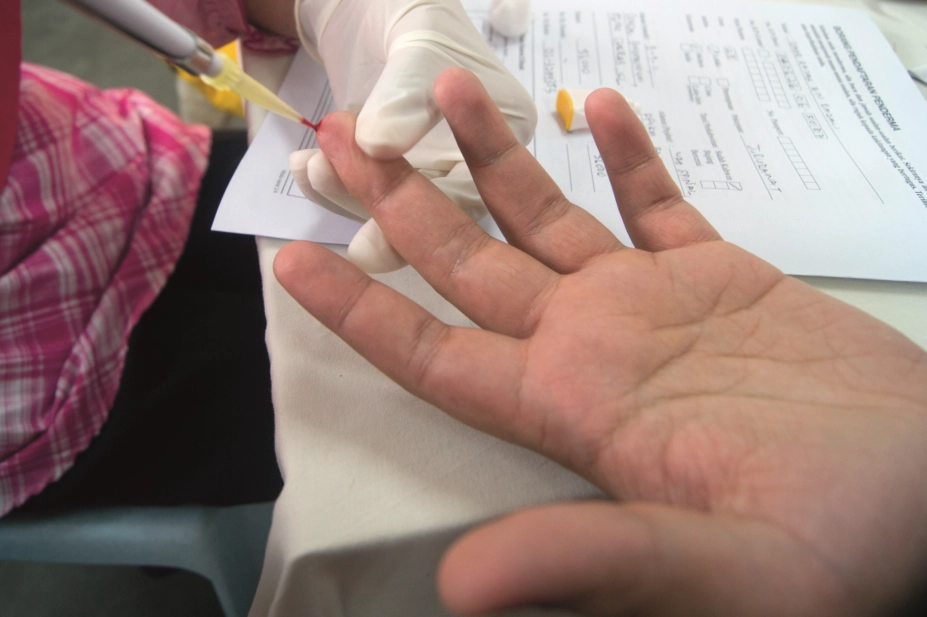
HIV testing should be available in pharmacies in areas of England where the condition is highly prevalent, says a new guideline from the National Institute for Health and Care Excellence (NICE) and Public Health England.
An estimated 101,200 people were living with HIV in the UK in 2015. Of these, more than 13,500 — or one in eight — are living with an undiagnosed infection.
To improve diagnosis in areas of high and extremely high prevalence, the guideline recommends offering HIV testing to everyone who has not previously been diagnosed with HIV who registers with a GP practice or who has a blood test.
The guideline says HIV testing should be available in community settings, such as pharmacies; the voluntary sector, such as faith groups; and venues where there may be high-risk sexual behaviour, including nightclubs, saunas and music festivals.
In areas where HIV prevalence is extremely high, people who have not been diagnosed with the condition should be tested on admission to hospital, including A&E department visits, even if they are having no other blood tests, the guideline says.
Areas of ‘extremely high prevalence’ are considered to have five or more diagnosed infections per 1,000 people aged 15–59 years — criteria met by 20 of the 152 local authorities in England. ‘High prevalence’ is considered to be or 2–5 diagnosed infections per 1,000 people aged 15–59 years — 54 local authorities in England fall into this category.
The guideline adds that the use of home self-sampling kits shows “great promise, especially as a way to engage people who are less likely to present at services”, and it recommends that people who decline testing are signposted to self-sampling services.
The guideline also points out that data from a self-sampling service that Public Health England runs with local authorities show that 32% of those tested had never had an HIV test before.
Commenting on the new guideline, Sandra Gidley, chair of the Royal Pharmaceutical Society English Pharmacy Board, says: “People infected with HIV but unaware of their status will have poorer health outcomes and are more likely to pass on the infection to others. Early detection of illness is a key part of pharmacists’ practice and opportunistic testing in pharmacies for HIV in high risk populations can make a huge contribution to improving patient outcomes.”
She added: “Providing tests in community pharmacies also gives the chance to detect HIV in people who may not want to visit a sexual health clinic, but it must be remembered that testing and diagnosis should always be accompanied with appropriate counselling and signposting.”
Gillian Leng, deputy chief executive of NICE, says: “We want to normalise HIV testing so it isn’t viewed any differently from any other blood test. There are now highly effective treatments for HIV and it should no longer be seen with fear or stigma.”
Philippa Matthews, clinical lead for HIV, sexual and reproductive health for the Royal College of GPs, welcomed the guideline, but says there are barriers for GP surgeries to offer wide-scale HIV testing. “Funding for such initiatives is currently decided by local councils, and there is no uniformity across the country. There is also the issue of effective implementation — including training and support for practices to adopt these schemes.”
“Furthermore, there are sensitivities that GPs need to take into account when offering HIV tests to patients who are usually visiting the GP for reasons not connected with HIV; a conversation that is difficult within the frustrating constraints of the standard ten-minute consultation,” she adds.
The strain placed on councils by central government cuts to public health budgets is expected to make the recommendations in the guideline difficult to implement. Recognising this, the Elton John Aids Foundation has offered to fund HIV testing for two years in Lambeth — the UK local authority with the highest rate of HIV.

