Opabinia regalis / Wikimedia Commons
A new treatment for heart failure with the “potential to change clinical practice” could save the lives of 20% more patients than the current gold-standard therapy, according to the results of a large clinical trial.
The results were so compelling that the trial – known as PARADIGM-HF and published in The New England Journal of Medicine[1] (online, 30 August 2014) – was called to a halt seven months before it was due to finish. Researchers reported an “overwhelming benefit” from the investigational treatment compared with enalapril, the widely used angiotensin-converting enzyme (ACE) inhibitor.
The trial set out to examine the effect of a new therapy, named “LCZ696”, which comprised the novel neprilysin inhibitor sacubitril plus valsartan, an angiotensin-receptor blocker (ARB).
Helen Williams, consultant pharmacist cardiovascular disease for South London, attended the European Society of Cardiology conference where the results were presented. “PARADIGM-HF results were received very positively at the conference with evidence that LCZ696 has superior efficacy and better tolerability compared to the current gold standard, ACE-inhibitor therapy,” she said.
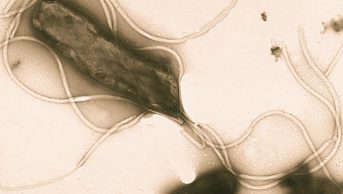
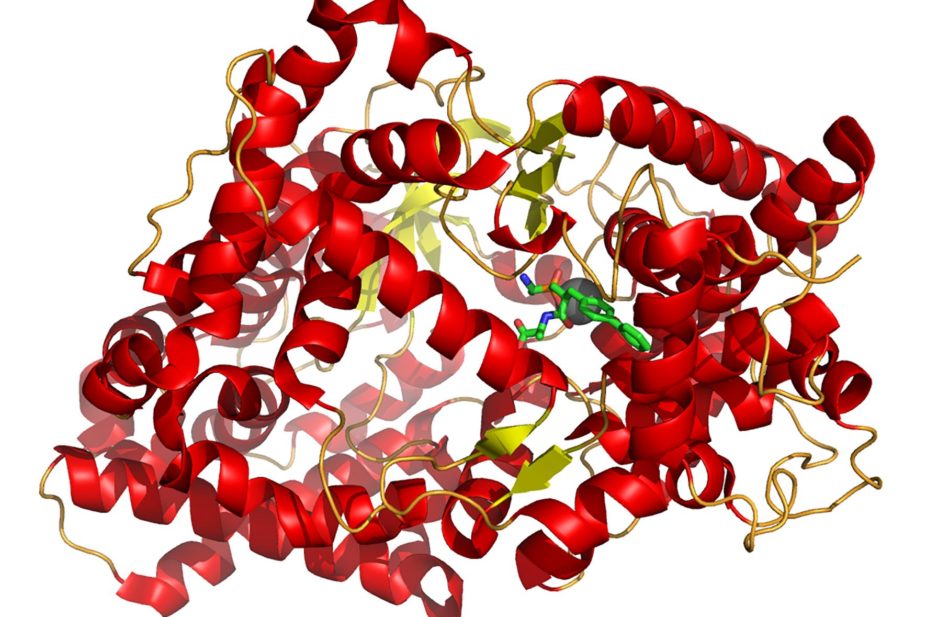
Sacubitril represents a new class of medicine; inhibiting the enzyme neprilysin, which is responsible for breaking down certain peptides that have an effect on blood vessel constriction. Inhibition of neprilysin increases the levels of these peptides, limiting vasoconstriction.
“In addition to the vasodilatory effect of valsartan, sacubitril enhances levels of endogenous natriuretic-peptide vasodilators,” explains Sotiris Antoniou, consultant pharmacist cardiovascular medicine at Barts Health NHS Trust. “The combination of the two demonstrated a reduction in the risk of death from cardiovascular causes by 20% – a number needed to treat (NNT) of just 32 – and the primary endpoint of death or hospitalisations from cardiovascular disease (CVD) by 20% (NNT 22) compared with the ACE inhibitor, enalapril.”
Previous studies have found that giving a neprilysin inhibitor with an ACE-inhibitor had a superior effect on heart failure compared with either drug alone, but the combination was associated with unacceptable levels of angioedema.
To minimise the risk of angioedema, in this study, the neprilysin inhibitor was combined with an ARB.
“In this study there was a higher rate of angioedema with the investigational product LCZ696, which is a potential concern,” says Williams. “However, the incidence of angioedema, even with this product was < 0.5% with an NNT of around 222 (compared to < 0.25% with enalparil; NNT around 422) so the absolute risk is low and the risk to benefit ratio still favours the new product.”
Williams described the new drug as an important and promising development, with the potential to change clinical practice. However, she says that the timeline for introduction into the clinic is unclear. “As a new class of drug, further research would be valuable to demonstrate that this result can be reproduced,” she says.
Antoniou believes that, based on the strength of the results, LCZ696 could eventually replace ACE inhibitors.
In an editorial supporting The New England Journal of Medicine paper[2]
, Mariell Jessup, of the Hospital of the University of Pennsylvania and the Presbyterian Medical Center of Philadelphia, points out that apart from the launch of ivabradine in 2012, treatment for heart failure has remained essentially unchanged for a decade. “PARADIGM-HF may well represent a new threshold of hope for patients with heart failure,” she says, adding that the beneficial results may apply to a wide spectrum of patients, even those currently receiving the best possible therapy.
Study results
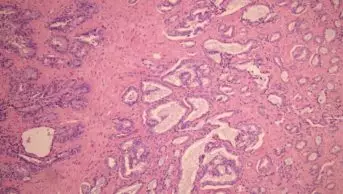
Patients with stage II, III or IV heart failure and an ejection fraction of <40% (later changed to a threshold of <35%) were randomised to receive either 200mg LCZ696 twice daily (n=4,187) or 10mg enalapril twice daily (n=4,212). Patients continued to receive their other medicines for heart failure, such as beta-blockers.
Initially, the trial was intended to last 34 months, but was stopped after 27 months due to the clear superiority of LCZ696 treatment over enalapril.
The number of patients who died or were admitted to hospital due to cardiovascular causes was 914 in the LCZ696 group and 1,117 in the enalapril group (hazard ratio 0.80, 95% confidence interval 0.73–0.87; P<0.001). A total of 711 patients in the LCZ696 group died, compared with 835 in the enalapril group (HR 0.84, 95% CI 0.76–0.93; P<0.001) and of these, cardiovascular causes accounted for 558 deaths and 693 deaths, respectively (HR 0.80, 95% CI 0.71–0.89: P<0.001).
Quality of life improved significantly in the LCZ696 group of patients compared with the patients receiving enalapril, as measured by the Kansas City Cardiomyopathy Questionnaire. However, patients in the LCZ696 group had higher rates of non-serious angioedema and symptomatic hypotension, but lower rates of renal impairment, hyperkalaemia and cough compared to the enalapril patients. Overall, the authors conclude that there were no important safety concerns associated with LCZ696 and fewer patients in this group discontinued their medication.
References
[1] McMurray JJV, Packer M, Desai AS, et al. Angiotensin–Neprilysin Inhibition versus Enalapril in Heart Failure. The New England Journal of Medicine. Available from: doi:10.1056/NEJMoa1409077
[2] Jessup M. Neprilysin Inhibition — A Novel Therapy for Heart Failure. The New England Journal of Medicine. Available from: doi: 10.1056/NEJMe1409898