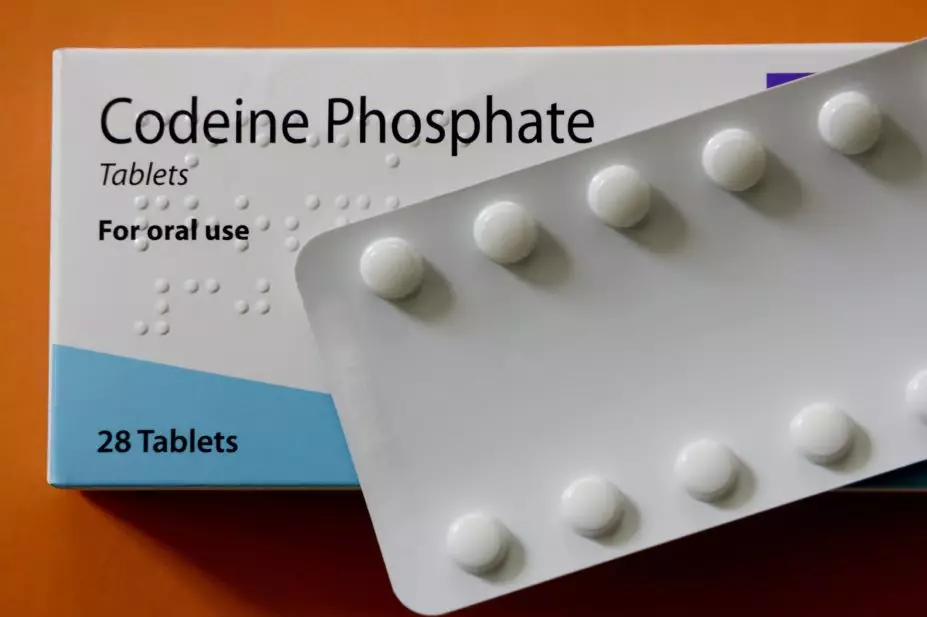
SHEILA TERRY/SCIENCE PHOTO LIBRARY
Opioid prescribing in Wales has increased by 30% in the past decade, according to figures published by the Welsh government.
The opioid prescribing figures, published on 10 February 2020, revealed that 1,594,473 opioid items were prescribed in Wales in 2018/2019, compared with 1,108,098 items in 2008/2009.
The figures also revealed that opioid prescribing had increased significantly across all seven local health boards (see Table).
| Local health board | Items prescribed in 2008/2009 | Items prescribed in 2018/2019 | Percentage increase |
|---|---|---|---|
| Abertawe Bro Morgannwg University Health Board | 177,759 | 279,576 | 57.3% |
| Aneurin Bevan University Health Board | 222,530 | 275,331 | 23.7% |
| Betsi Cadwaladr University Health Board | 257,044 | 358,123 | 39.3% |
| Cardiff and Vale University Health Board | 142,478 | 182,400 | 28.0% |
| Cwm Taf Morgannwg University Health Board | 99,561 | 149,028 | 49.7% |
| Hywel Dda University Health Board | 166,326 | 267,638 | 60.9% |
| Powys Teaching Health Board | 42,400 | 82,377 | 94.3% |
However, the figures also show that across Wales opioid prescribing did decrease marginally by 0.3% between 2016/2017 and 2018/2019.
Emma Davies, formerly advanced pharmacy practitioner in pain management at Abertawe Bro Morgannwg University Health Board (now at Cwm Taf Morgannwg University Health Board) — where prescribing has increased by around 57% since 2008/2009 — said the high level of analgesic prescribing across the country was a “cause for concern”, but added that it would not be a surprise to anyone working in community and primary care in Wales.
“There are high levels of short-term prescriptions but, over the years, the numbers of people receiving long-term prescriptions of analgesics has also risen,” she said.
“There needs to be an acknowledgement about the complexity of pain, as a condition and the multi-factorial nature of it.
“For example, persistent pain, which much of this prescribing is for, is more prevalent in areas of greater deprivation — as is depression and anxiety — all these things add to the pain burden and while [they] are not fixed by analgesics, [they] are also not fixed by removing them.”
Davies added that without having access to supportive services from the moment patients present, it was very difficult for prescribers to avoid prescribing such medication.
“Similarly, if the people presenting with pain are not aware of the numerous problems with analgesics – mostly that they really aren’t very effective – they will continue to ask for and expect them.”
A Public Health England review, published in September 2019, found that more than 500,000 patients in England were continuously prescribed an opioid for three years or more, despite a lack of evidence showing their efficacy in the long term.
In response to high opioid prescribing rates, Sunderland Clinical Commisioning Group launched an awareness campaign in October 2019 aimed at tackling addition to the drugs.
Responding to the opioid prescribing figures, a spokesperson for the Welsh government said: “An increase in opioid prescriptions between 2008/2009 to 2018/2019 was seen across the whole of the UK however in Wales opioid prescribing fell by 0.3% between 2016/2017 and 2018/2019.
“The latest data published by the All Wales Medicines Strategy Group indicates further decreases in opioid prescribing in the current year.
They added: “Tackling dependence on prescription-only medicines and over-the-counter medicines is a priority areas identified within our ‘Substance misuse delivery plan 2019/2022’ and, [in 2019], we published guidance on living with persistent pain, with a focus on the need to ensure those living with pain are helped to reduce or stop taking non-beneficial medications.”
Also, when prescribing strong opioids, the spokesperson said clinicians must discuss with their patients any concerns they may have regarding addiction, tolerance and side effects.
An investigation by The Pharmaceutical Journal
in February 2020 found that four out of five providers in Wales reported an average waiting time of more than 20 weeks for patients accessing treatment after referral to a chronic pain management service.
- This article was amended on 27 March 2023 to correct Emma Davies’ affiliation