
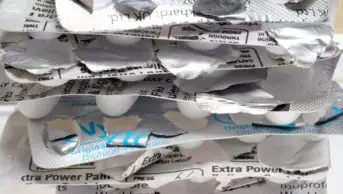
Shutterstock.com
Pharmacists could be given new powers to prescribe medicines in low-risk situations as part of new legislation being put forward by the government.
The Medicines and Medical Devices Bill 2019/2020, which was first announced in the Queen’s Speech in December 2019 and will be introduced by the Department of Health and Social Care (DHSC) on 13 February 2020, would also enable hospitals to use patient DNA to manufacture tailor-made drugs in an effort to improve access to treatments for patients with rare cancers and brain tumours.
This comes after the government set out plans in the October 2019 Queen’s Speech to introduce legislation to allow a wider range of healthcare professionals in the NHS to prescribe ‘low-risk’ medicines.
A DHSC statement, published on 13 February 2020, said the legislation will “allow the sector to increase the range of professions able to prescribe medicines in low-risk circumstances, as midwives and paramedics do now with pain relief, and physiotherapists with anti-inflammatories”.
“This will be with appropriate safeguards and clear limits on what medications are eligible,” it added.
The DHSC confirmed to The Pharmaceutical Journal
on 13 February 2020 that the list of healthcare professionals given the powers to prescribe these types of medicines could “potentially” include pharmacists, subject to a consultation.
It added that the definition of ‘low-risk’ circumstances would also be consulted on.
“This allows the NHS to make the very best use of its highly skilled workforce, to save patients’ time and reduce unnecessary GP appointments,” the statement added.
Sandra Gidley, president of the Royal Pharmaceutical Society, commented: “Given that pharmacists have greater expertise in drug use than any other profession, this would appear to be a good move.
“We have yet to see the detail, but thought should also be given as to how to make better use of pharmacy independent prescribers in community settings.”
The new legislation will also enable hospitals to use patient tissue and DNA samples “to tailor innovative treatments for individual patients when other medicines have failed,” the DHSC said.
It also said the bill will allow hospitals, in their existing facilities, “to develop drugs that have a shelf-life of minutes and wouÆ’ld otherwise be unavailable to them”.
“This has the potential to streamline access to treatments for patients with rare cancers and brain tumours.”
Aamer Safdar, pharmacy education, training and workforce development team lead at Barts Health NHS Trust, told The Pharmaceutical Journal that the new legislation “is good news for patients and for researchers as it will allow innovation in the growing area of personalised medicines”.
“This will inevitably mean that hospital pharmacies will need to review how they manage these treatments in terms of handling, manipulating and providing to patients,” he said.
“The wider care that pharmacists may need to provide on an individual basis to patients will be important. Hospitals will need to be resourced appropriately so that they have the facilities to provide these new treatments by highly skilled members of the pharmacy team.”
Baroness Nicola Blackwood, parliamentary under secretary of state at the DHSC, said the legislation will give the NHS “further freedom to innovate to improve the lives of countless people and protect patient safety to the highest standards”.
“It will slash red tape, support uptake of treatments for people with rare diseases and empower those in the NHS who know what’s best for their patients to deliver the best quality care,” she said.
You may also be interested in
Government misses consultation deadline for post-Brexit scheme to detect fake medicines

Proposed legislation could see government ‘broaden’ use of data collected through the Falsified Medicines Directive
