Shutterstock.com
Restricting access to over-the-counter (OTC) medicines could lead to significant health inequalities, the Royal Pharmaceutical Society (RPS), Pharmaceutical Services Negotiating Committee (PSNC), the Association of the British Pharmaceutical Industry (ABPI) and the National Pharmacy Association (NPA) have all agreed.
Responding to a three-month consultation by NHS England and NHS Clinical Commissioners on items that should not routinely be prescribed in primary care, The RPS, PSNC, ABPI, and NPA each called for further evidence to clarify the impact on people on low incomes if OTC products were no longer supplied on the NHS.
The consultation, which closed on 21 October 2017, sought the views of the public, patients and professionals on proposed national guidance for clinical commissioning groups (CCGs) on 18 medicines and treatments identified to be of low value, including homeopathy and some travel vaccinations.
The proposals would see prescribing of all the products limited in some way, but the final recommendations will only constitute advice to CCGs and will not be binding.
Additionally, section five of the consultation asked for views on more than 3,200 medicines, currently available OTC, which could be added to the not routinely prescribed list. These medicines are described by NHS England as being for conditions that are minor or self-limiting, and include treatments for diarrhoea, constipation and head lice.
Section five
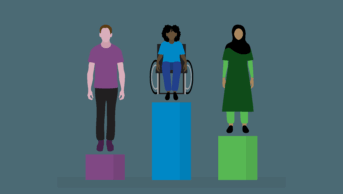
“These proposals would not only adversely affect a patient’s health and care, but also consequently target and potentially discriminate against people with long-term conditions, patients with multimorbidities, the young, cancer sufferers, the elderly and the poorest in society,” said the RPS in its consultation response.
“While we recognise the NHS needs to operate within its budget allocated by government, as proposals currently stand, we could not support health professionals being asked to restrict access to cost-effective treatment.”
The NPA said that “significant health inequalities” may arise, and it highlighted the likely adverse impact on older women in particular, which was identified in the consultation and said that “more females are prescribed the defined list of medicines than males…more frequently to over 65 year olds.”
It went on to suggest that a nationally advanced minor ailment service would “negate the need for implementation of what could potentially be a divisive policy affecting the most disadvantaged individuals in our society.”
In its response to the consultation, the PSNC said that if restrictions were implemented there must be a comprehensive implementation plan with the full involvement of community pharmacy.
In their consultation responses, both the ABPI and the Proprietary Association of Great Britain (PAGB), a trade association representing the consumer healthcare industry, said it was vital to encourage more people to self-care, possibly with advice from a pharmacist.
Section four
The RPS, PSNC and ABPI largely welcomed the proposals in section four of the consultation, which dealt with the 18 low-value medicines, and particularly those that would severely limit the ability to prescribe homeopathy and herbal remedies.
The PSNC, ABPI and NPA all suggested that some of the products should be added to the NHS prescribing “blacklist”, which would remove the ability to prescribe them on the NHS at all. This would provide greater clarity for community pharmacy teams and others involved in the prescribing process.
The ABPI expressed strong concerns over limiting the prescribing of travel vaccines, which it said could have “serious public health implications” and a disproportionate impact on black and minority ethnic (BME) and low-income travellers from high risk destinations.
The NPA also warned that limiting travel vaccines could result in an inadvertent cost to the NHS if patients travelled to at-risk areas without vaccinations.
In its response to the consultation, the PSNC recommended that local pharmaceutical committees should be engaged in discussions organised by CCGs to plan local implementation of the proposals. It added that all patients affected by the changes should have a face-to-face consultation to discuss them.
The RPS said the consultation highlighted an opportunity to develop services in primary care using the skills of community pharmacists to support patients who do not have the means to purchase the products under discussion.
The NPA claimed that far greater cost-efficiencies could be made across the health system by helping people to make best use of medicines prescribed for long term conditions, with support from their local pharmacist.
A spokesperson for NHS England said the NHS England Board would consider the responses to the consultation before publishing final guidance “in due course”.