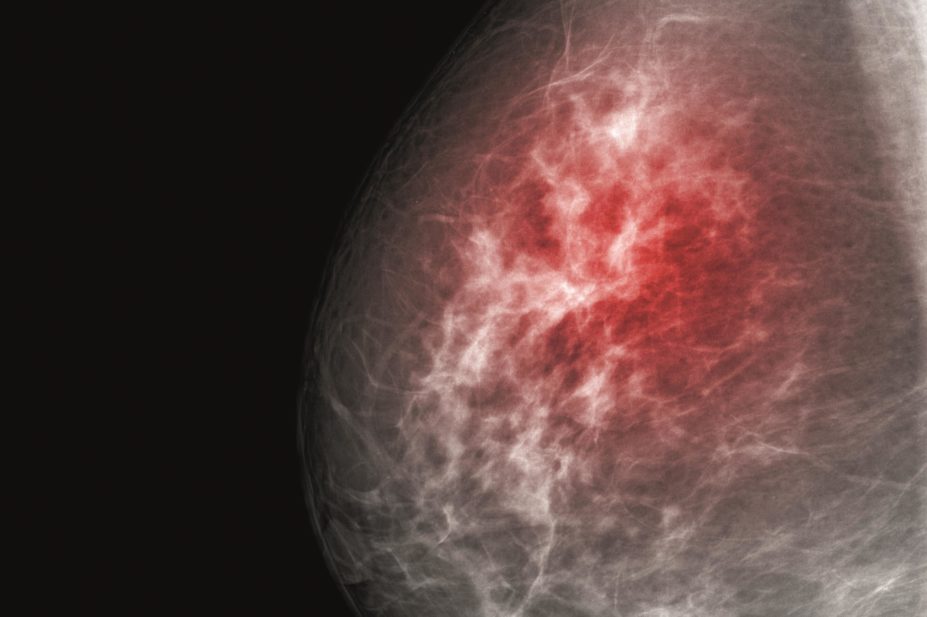
Shutterstock.com
Researchers have discovered why breast cancer patients whose tumours display both oestrogen and progesterone receptors have the best chance of survival, which has long been observed but not understood.
The finding[1]
could benefit up to half of all breast cancer patients, leading to the development of a hormone treatment that is cheap, safe and widely available.
It has long been known that tumours with oestrogen receptors (ER) and progesterone receptors (PR) (ER/PR double positive) have the best clinical outcome, but the interplay between the two proteins has remained unknown. Both are transcription factors, which means they are both involved in switching genes on and off in cells.
Breast cancer cells have increased sensitivity to oestrogen. Once oestrogen has bound to ER on the surface of these cells, the ER enters the cell and ends up in the nucleus, where it attaches to specific regions of DNA, switching on transcription of a group of genes that promote cell division and hence tumour growth.
Exactly what the PR does – if anything – while this is happening has remained unclear. All that was known was that the presence of these receptors would slow tumour growth. Now, Jason Carroll of Cancer Research UK’s Cambridge Research Institute and colleagues, have taken a closer look.
“We’ve used cutting-edge technology to tease out the crucial role that progesterone receptors play in breast cancer — a mystery that has baffled scientists for many years,” says Carroll. “This important laboratory research helps explain why some breast cancer patients have a better outlook.”
The team grew breast cancer cells that displayed both ER and PR in the laboratory, and made sure the cells had enough oestrogen and progesterone to bind to the receptors. The researchers then removed the PR (which had bound to progesterone) from the cells, and were surprised to find that the PR was now bound to the ER.
Since both receptors are transcription factors, Carroll’s team investigated whether this unexpected binding would affect gene transcription. They examined where the ER would attach to DNA in the absence of progesterone, and looked at where the ER would attach to DNA in the presence of progesterone and its receptor.
The researchers found that the receptor bound to different regions of DNA depending on whether progesterone was present. In other words, the PR (that had bound to progesterone) was changing the genes that the ER was switching on or off. Alongside this, the researchers saw that progesterone was associated with a slowing of cancer cell growth. The pattern was seen again in studies with different cancer cells and in mice.
The findings are particularly exciting because progesterone, which slowed tumour growth in both cells and in an animal model, is a cheap, safe, and widely available drug.
“These findings are an exciting development in our understanding of how hormones may make certain breast cancers grow,” says Samia al Qadhi, chief executive of the breast cancer support charity, Breast Cancer Care.
“There are 55,000 women every year in the UK dealing with the overwhelming news they have breast cancer, so any research to help improve treatments can only be welcomed,” says al Qadhi, “This interesting study is in its early stages. We look forward to hearing whether it will lead to trials on people, establishing if progesterone could be an effective treatment for patients in the future.”
Carroll is hopeful. “We’re already discussing a clinical trial to test whether giving women with ER/PR double-positive breast cancer progesterone, alongside oestrogen-blocking drugs, helps more women survive this disease,” he says.
Cancer Research UK issued a warning following media coverage of the study. “We want to clear up an important point: the effects observed in this study were from using progesterone itself. Many contraceptives, and certain forms of HRT, contain derivatives of progesterone (e.g. medroxyprogesterone acetate, MPA) — these seem to act differently. So headlines claiming that ‘a hormone found in the Pill slows growth of tumours’ are slightly inaccurate.”
References
[1] Mohammed H, Russell A, Stark R et al. Progesterone receptor modulates ERa action in breast cancer. Nature 2015. doi:10.1038/nature14583.


