Imagedoc / Alamy Stock Photo
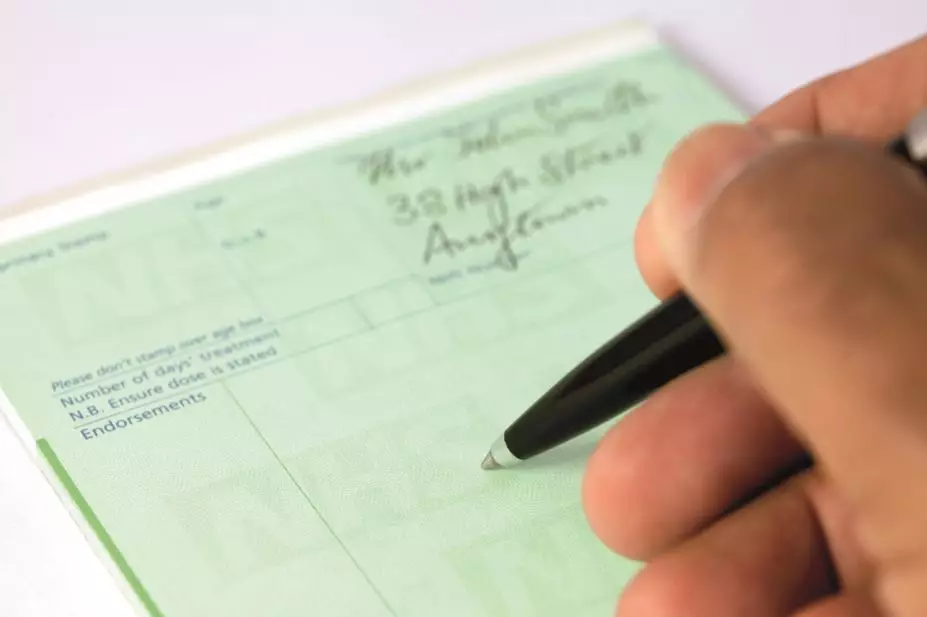
Prescribing safety indicators are now widely used with electronic medical records in the UK to identify patients at risk of prescribing errors.
However, there is no agreement on what is an acceptable level of high-risk prescribing and it is unclear if the indicators could be used to compare prescribing safety between general practices.
An audit of 526 general practices, published in The BMJ
[1]
(online, 3 November 2015), found that 49,927 (5.3%) of 949,552 patients had received a potentially inappropriate prescription, while 21,501 (11.8%) patients had not received adequate monitoring during treatment.
The researchers, from the University of Manchester, found a wide variation between practices, suggesting scope for improving safety. However, they say further research is needed to determine how often prescribing indicators are triggered by clinical decisions as opposed to oversight or error.
References
[1] Stocks SJ, Kontopantelis E, Akbarov A et al. Examining variations in prescribing safety in UK general practice: cross sectional study using the Clinical Practice Research Datalink. BMJ 2015;351:h5501. doi:10.1136/bmj.h5501


