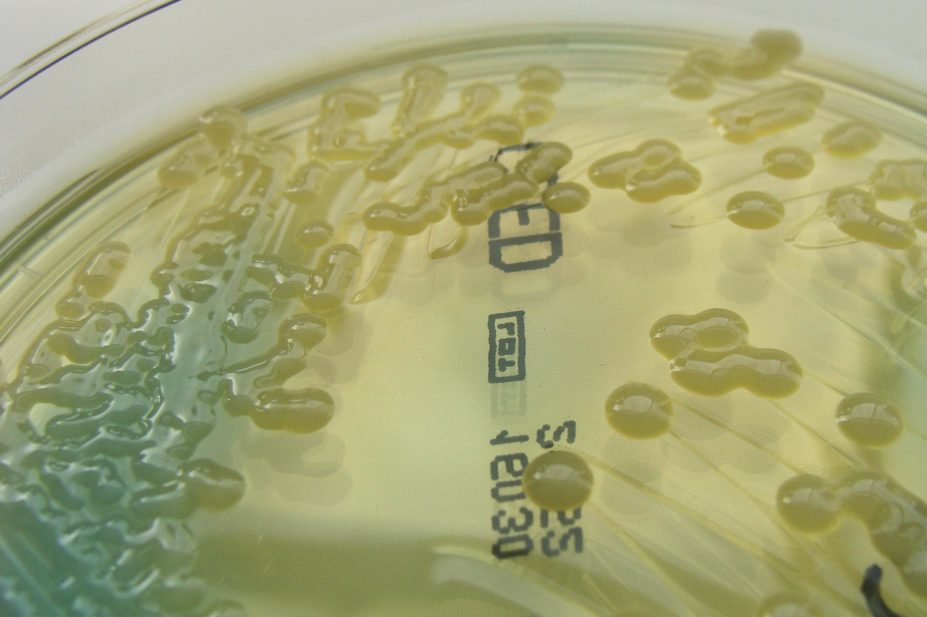
Nathan Reading / Wkimedia Commons
A comprehensive antibiotic stewardship programme at a New York city hospital saved money, reduced drug-resistant infections and led to an increase in the reporting of adverse events, according to a study presented at the American Society for Microbiology’s annual ICAAC meeting in Washington, DC[1]
.
Stewardship programmes, under which the use of antibiotics is closely monitored, reported on and managed, aim to improve their appropriate use and reduce antibiotic resistance.
In 2013, the initiative saved more than US$600,000 and involved more than 5,000 interventions. At least half of the interventions saved money, the study found. The pharmacist heading the programme reported 63 adverse drug reactions in 2013, while the physician’s assistants reported 41.
Nishant Prasad, infectious disease attending physician at the 535-bed New York Hospital in Queens, New York City said the programme had worked “quite well” and in some unexpected areas.
However, the programme did not reveal improved patient outcomes. “Outcomes are really difficult to do,” said Prasad. “There is an association between these interventions and patient outcomes, but none has been shown to be statistically significant, because there were too many confounding factors.”
Researchers analysing the frequency of multi-drug resistant microorganisms found resistant strains of Klebsiella pneumoniae decreased in prevalence from 17.7% in 2011 to 10.5% in 2013. Resistant Acinetobacter baumannii also decreased from 43.3% to 39.5% during that time, and meticillin-resistant Staphylococcus aureus decreased from 56.8% to 41.6%. The researchers paid special attention to Clostridium difficile-associated diarrhea, which also decreased from 18.4% to 11.4%.
Of the various interventions, 31% were antibiotic renal adjustments, 21% discontinuations and 18% were changes from intravenous (IV) to oral therapies.
From 2012 to 2013, expenditure on daptomycin decreased by 50%. At the same time, there was a 169% increase in IV rifampin costs, and an 88% decrease for cefepime.
“Some of the most significant cost savings came from the change in daptomycin use,” explained Prasad, who noted that an increase in the price of rifampin in 2013 was associated with a 20% decrease in its use.
References
[1] Prasad N, Warren N, Kula A, et al. Impact of antibiotic stewardship program interventions on multi-drug resistant organism resistance rates and hospital costs. [Poster K-343] American Society for Microbiology. Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington DC. 6 September 2014.


