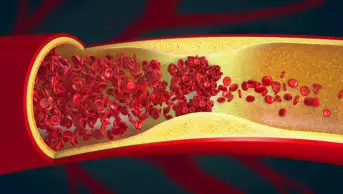
Shutterstock
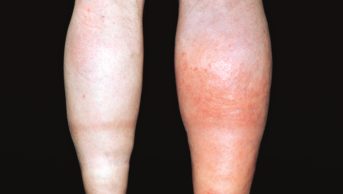
Giving anti-clotting drugs routinely to all patients as prophylaxis against developing venous thromboembolism (VTE) after surgery may be unnecessary in as many as 75% of cases, according to research published in the Annals of Surgery
[1]
(online, 19 January 2017).
The study throws into question the common practice that all patients who are to undergo general surgery should be given anticoagulants regardless of their individual risk of developing a VTE, the researchers say.
“These data argue strongly for a precision medicine approach to VTE chemoprophylaxis, where the intervention is guided by the risk/benefit relationship at the patient level. These data also provide strong evidence about who should not receive chemoprophylaxis,” the team says.
The researchers base their conclusions on an analysis of 14,776 patient records from 13 studies when they set out to discover which surgical patients were more likely and least likely to benefit from being given anticoagulants. All the studies included data on patients with postoperative VTE and/or bleeding events with and without chemoprophylaxis (the studies also included mechanical prophylaxis).
The team took into account the patients’ Caprini score – the commonly used assessment tool that calculates an individual’s risk of developing a VTE. A patient with a 0–2 Caprini score has a small risk of developing a VTE, but this rises as the number of risk factors a patient has increases.
The researchers discovered that patients with Caprini scores of 7 to 8 and greater than 8 had a significant reduction in peri-operative VTE when chemoprophylaxis was received. This had previously been shown in plastic and reconstructive surgery, but never in the general surgical population, they say.
But patients with Caprini scores of 6 or under — who accounted for 75% of the patient population — did not have a “significant” VTE risk reduction with chemoprophylaxis.
This study also looked at bleeding risk in response to chemoprophylaxis when stratified by VTE risk score, and shows that there is no clear association between Caprini score and risk for bleeding.
The research was welcomed by Sotiris Antoniou, consultant pharmacist in cardiovascular medicine, Barts Health NHS Trust in London.
Antoniou, who is also honorary senior research associate at UCL School of Pharmacy, says: “As we move into a more personalised medicine approach, this [study] provides a reminder that all medicines pose a risk.
“VTE prophylaxis in surgical patients currently falls under the ‘one-size-fits-all’ approach and using a risk stratification score (for example, Caprini) may allow us to fine tune the need and identify some individuals who may not receive any tangible benefit from receiving pharmacological VTE prophylaxis, yet be exposed to bleeding risk.
“For the past decade the drive in the UK has been to promote VTE prophylaxis, recognising that as many as 70% of patients assessed to be at medium or high risk of developing deep vein thrombosis did not receive any form of mechanical or pharmacological VTE prophylaxis, contributing to 25,000 deaths from preventable hospital-acquired VTE every year.”
He says that VTE guidance from the UK’s health technology assessment body, the National Institute for Health and Care Excellence, does provide reference to bleeding considerations by highlighting risk factors. “This paper further complements this to continue the journey for an individualised approach.”
References
[1] Pannucci CJ, Swistun L, MacDonald JK et al. Individualized venous thromboembolism risk stratification using the 2005 Caprini score to identify the benefits and harms of chemoprophylaxis in surgical patients. doi: 10.1097/SLA.0000000000002126