
Samrina Bhatti
Closed loop medicines administration (CLMA) is the functionality that supports the cross checking of the correct patient, medicine and prescription using digital technologies. Specifically, checking should be used to confirm the patient identity against the medicine/dose due and the actual medicine that is selected for administration — appropriate decision support should be generated if there is a mismatch, whilst the administration should be recorded as given should the checks all match correctly (see figure 1).
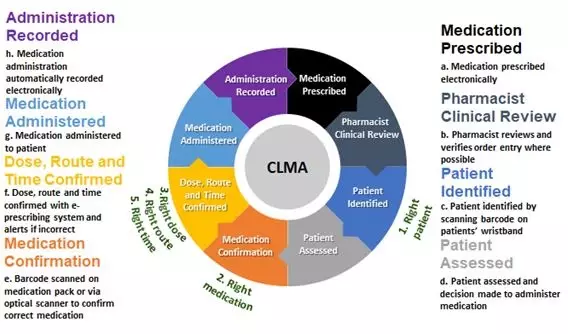
Figure 1: Closed loop medicines administration
Source: Samrina Bhatti
CLMA offers a means of reducing medication related administration error whilst identifying the type of error potentially avoided. Using ‘traditional’ methods, staff are not always aware that an error or near miss has occurred, particularly where no patient harm has resulted1. Evidence demonstrates that medication errors can be minimised using CLMA by addressing the ‘five rights’ of medicines administration (see Table 1).
| Evidence shows that CLMA can reduce the overall rate of adverse drug events and decrease transcription errors by supporting staff administering medications in confirming the ‘five rights’ of medication administration in real time2. | |
|---|---|
| Right Patient | Identifiable by scanning the barcode on a patient’s wristband. |
| Right Medication | Identifiable by scanning a barcode on the medication package / label or by using an optical medication scanner. If the medicaiton sanned does not match that which is prescribed, a warning appears. |
| Right Route | The electronic prescription can be cross referenced to ensure the right route is used for administration based on the profile of the scanned medication. The system provides a warning alert if the ‘normal’ route for the medication scanned does not match the prescription via the formulation. |
| Right Time | The user can ensure the medication is being administered at the right time by searching for a scheduled due time that falls within the permitted time window for documenting administrations. A warning alert is generated if the medicaiton scanned falls outside the scheduled administration window. |
| Right Dose | The integrated medication scanning system compares the dose to be administered with the prescription; a warning appears if the doses do not match. |
The driver behind the introduction of CLMA is to reduce medication administration related risks and errors improving the quality of care. An estimated 237 million medication errors occur in the NHS in England every year3. Of these, 54.4% are administration errors across all settings1. Furthermore, adverse drug events can lead to increased length of hospital stay, healthcare costs, patient morbidity and mortality. Studies have found medicines administration error rates in hospital to be between 10.5-19.7%4. The Medicines Safety Programme5 has been established in response to the WHO Global Patient Safety Challenge which aims to reduce the level of severe, avoidable harm related to medications by 50% over 5 years, globally6. CLMA is a good example of a digital transformation which can improve care and efficiency.
The benefits of providing a CLMA process are now becoming evident as sites are beginning to implement the system. Published evidence has largely focussed on the reduction of adverse drug events and the impact on patient care1.
Interim work from sites is largely focussing on patient safety benefits. Cambridge University Hospitals NHS Foundation Trust has demonstrated that scanning is highlighting potential errors that are being acted upon by staff using the process. The interim results can be seen in table 2 below. The data refers to approximately 11,500 administrations per day. The table shows that in February 2019, 2.2% of potential medication errors were averted due to the use of barcode scanning system alerting.
| Interim results for closed loop medicines administration at Cambridge University Hospitals NHS Foundation Trust. | ||||
|---|---|---|---|---|
*No order: when a barcode is scanned and the medication cannot be matched to an active order. **No active order: when an attempt is being made to administer a medication to a patient where that patient previously had an active order for that medication, but that order has since been discontinued by the clinical team. | ||||
| November 2018 | December 2018 | January 2019 | February 2019 | |
| Medication scan rate | 65.7% | 66.3% | 68.1% | 70.0% |
| No order* | 4229 (1.2%) | 4401 (1.3%) | 4722 (1.3%) | 4586 (1.4%) |
| No active order** | 2631 (0.7%) | 2369 (0.7%) | 2645 (0.7%) | 2774 (0.8%) |
| Total | 6860 (1.9%) | 6770 (2%) | 7367 (2%) | 7360 (2.2%) |
Similarly, St George’s University Hospitals NHS Foundation Trust data demonstrates that between February 2018 and February 2019 scanning the barcode on the patient’s wristband during medication administration, prevented practitioners from administering to an incorrect patient 14,678 times. Scanning the medication pack prevented practitioners from administering an incorrect medication or dose 113,674 times.
As adoption of CLMA is in its infancy across the NHS, it is hoped that sharing knowledge will help to prevent duplication of lessons learnt and further promote collaborative working. I was tasked with developing a toolkit to aid implementation of CLMA, on behalf of the Medicine’s Optimisation Digital Global Digital Exemplar Learning Network, through a series of engagements with NHS organisations and national workshops.
The toolkit highlights the practical challenges around implementing CLMA. It aims to support trust teams including chief clinical information officers, nursing and pharmacy teams. The development of this toolkit would not have been possible without those who shared their learning.
In conclusion, common with other transformation programmes, the introduction to CLMA requires careful planning and wide engagement with clinical leadership to ensure success. There is growing experience of implementing technology to support medicines administration with positive benefits being identified. Sites embarking on their journey should learn from and collaborate with others as well as use the national resources available. The Medicines Optimisation Digital Learning Network will continue to provide a central platform to support and share this work.
The toolkit can be accessed here.

Source: Samrina Bhatti
About the author:
Samrina is the chief pharmaceutical officer’s clinical fellow for NHS England, Specialist Pharmacy Service and is an associate of the Faculty of Clinical Informatics. She has a background in patient safety, clinical governance and healthcare technology.
References:
1. Truitt, E. Effect of the Implementation of Barcode Technology and an Electronic Medication Administration Record on Adverse Drug Events. Hosp Pharm. 2016;51(6): 474-483.
2. Cambridge University Hospitals. (2018). Global Digital Exemplar Blueprint.
3. EEPRUorguk. EEPRU. [Online]. Available from: http://www.eepru.org.uk/prevalence-and-economic-burden-of-medication-errors-in-the-nhs-in-england-2/ [Accessed 9 June 2019].4. Berdot , S. Drug administration errors in hospital inpatients: a systematic review. Journalpone. 2013;8(10): 1371.
5. Medicines Safety Programme [Online]. Available from: https://www.sps.nhs.uk/wp-content/uploads/2018/02/1-RICHARD-CATTELL-Medicines-Safety-Programme-Slides-MUSN.pdf [Accessed 9 June 2019]
6. World Health Organisation. [Online]. Available from: https://www.who.int/news-room/detail/29-03-2017-who-launches-global-effort-to-halve-medication-related-errors-in-5-years [Accessed 9 June 2019].


