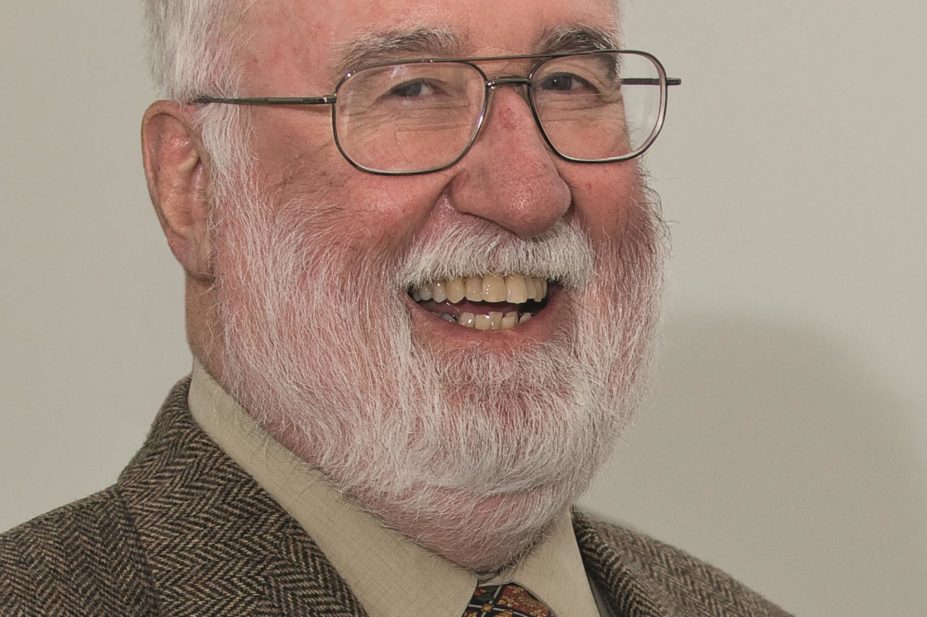
Eric Bosch
“Be loyal to people, not institutions, and serve the young” is how David Sackett characterised his life’s philosophy. He also identified a “predilection for marching to a different drummer”.
The pioneer and proponent of evidence-based medicine, who died in Canada of metastatic cholangiocarcinoma in May 2015, aged 80, was testing the validity of expert opinion early in his career.
As a medical student at the University of Illinois, he was frustrated by the justifications his seniors made for their therapeutic decisions, ranging from “that’s how we’ve always done it” and “that’s how the experts say we should do it” to “don’t talk back, just do it”.
As a final-year student caring for a teenager with infectious hepatitis, he queried the conventional wisdom that such patients should be kept in bed until their enlarged liver receded. Researching the question, he found a paper in the Journal of Clinical Investigation, which showed that time to recovery was indistinguishable between patients allocated to bed rest and those allowed to be up as much as they wanted.
Sackett convinced his supervisors to allow the teenager up and the patient made an uneventful recovery. “I became a troublemaker, constantly questioning conventional therapeutic wisdom,” he said.
After two years at the US Public Health Service in Buffalo, New York, Sackett, who was born in Chicago to a “bibliophile mother and artist/designer father”, studied epidemiology and biostatistics methods at Harvard School of Public Health.
In 1967, he was appointed the first chairman of clinical epidemiology and biostatistics at McMaster, the new medical school in Hamilton, Ontario, Canada. During his 27 years at McMaster he established many randomised controlled trials, including, in 1985, one demonstrating the beneficial effects of aspirin for patients with unstable angina[1]
.
“It essentially established the rationale for the use of aspirin for the prevention of cardiovascular outcomes — heart attack, stroke and cardiovascular death — in patients with unstable angina,” says John Cairns, professor of medicine and past dean at the University of British Columbia, one of the study’s authors. “Aspirin remains a foundational component of the treatment of unstable angina to this day.
“When I arrived at McMaster University in 1975 I was a fully trained cardiologist from McGill, but I had not worked with aspirin, nor been exposed to the concepts of large clinical trials,” Cairns recalls. “Dave’s generous guidance, optimism and sense of humour did wonders in drawing young investigators into the world of clinical research.”
Sackett was also physician-in-chief at Chedoke Hospital, Hamilton. Aged 49, he undertook a two-year “retreading” residency to ensure he did not lose touch with clinical medicine.
In 1994, he was invited to Oxford to become director of the Centre for Evidence-Based Medicine (CEBM), which he found “a breathtaking opportunity to a contented 59-year-old academic physician”. He was also a consultant at the John Radcliffe hospital. Defining evidence-based medicine in a paper in The
BMJ in 1996, as “the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients”, Sackett added: “Evidence-based medicine is neither old hat nor impossible to practice.” And he refuted arguments that it could only be conducted “from ivory towers and armchairs”.
“When asking questions about therapy we should avoid non-experimental approaches since these routinely lead to false positive questions about efficacy,” he said. “The randomised trial and especially the systematic review of several randomised trials is so much more likely to inform us and so much less likely to mislead us.”
But this was not widely welcomed in Oxford. “The initial response of the British medical ‘establishment’ was so negative, condescending and dismissive that I was often miserable for the first year and a half of my time there,” Sackett said.
“Not everything was plain sailing,” recalls Carl Heneghan, now director of the CEBM, who was a medical student in Oxford when he first met Sackett. “I’d say there was about a 50-50 split among the clinical staff, but among the juniors there was more than the fair share of support to make up for the dissent.”
To encourage effective decision making, Sackett came up with the idea of an “evidence cart”, whose contents included a laptop to search PubMed, a rapid printer for doctors, medical students and patients to take information away, textbooks on making physical diagnosis and a “red book” of critically appraised evidence. He would do a ward round of emergency admissions with young doctors showing evidence-based medicine in action.
An audit carried out a month before the cart arrived of 72 clinical cases that needed a search for evidence found only 19 searches were carried out. After the cart arrived, it was used for searches 98 times in a month.
“Strange how simple ideas capture the imagination, but folk would travel from abroad to see what was happening on the ward round,” says Heneghan. For his part, Sackett travelled around the UK, giving talks at some 200 hospitals, founded the journal Evidence Based Medicine in 1995 and co-authored ‘Evidence based medicine: how to practice and teach EBM’, published in 1997. The first print run of 2,500 sold out within a week and it is now in its fourth edition.
By 1999, Sackett thought evidence-based medicine had gained enough momentum for him to return to Canada to a cottage in Ontario where he ran workshops for researchers and argued for the compulsory retirement of “experts” who can “retard the advance of science and harm the young”.
“There are still far more experts around than is healthy for the advancement of science,” he wrote in the BMJ in 2000. “Surely a lot more people could retire from their fields and turn their intelligence, imagination and methodological acumen to new problem areas.”
Richard Smith, former editor of The BMJ and a friend of Sackett, described him on Twitter as “one of the medical greats and fun all the way”.
Sackett is survived by his wife Barbara (nee Bennett) and their four sons.
References
[1] Cairns JA, Gent M, Singer J et al. Aspirin, sulfinpyrazone or both in unstable angina — results of a Canadian multicenter trial. New England Journal of Medicine 1985;313:1359–1375.
You may also be interested in
Philip Leon Marshall Davies (1938–2026)

Bill Scott OBE (1949–2025)
