shutterstock.com
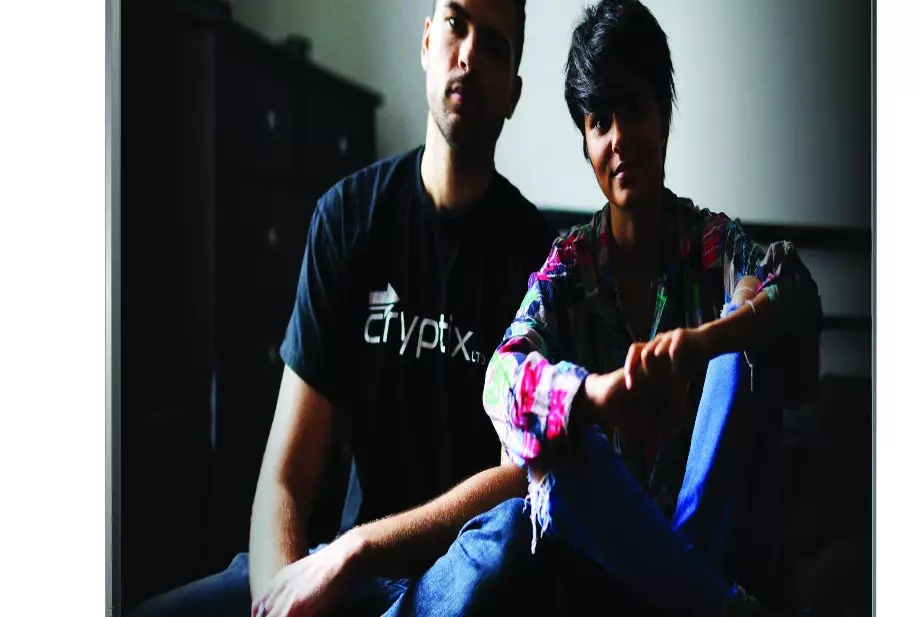
Sanah Ahsan was given a diagnosis of depression in her teens. She took antidepressants at the age of 17 years, and again in her 20s. They didn’t work. She considered taking her own life several times, but now she uses talking therapy to manage her condition.
In 2018, there were 700,000 referrals of people under the age of 19 years to mental health services — a 45% increase in two years. And in ‘Young, British and Depressed’, Ahsan — now training to become a psychologist for child and adolescent mental health services (CAMHS) — investigates this “youth depression crisis”.
Staggering statistics are accompanied by sobering video diaries from teenagers who talk candidly about their darkest thoughts, and we hear from leading voices in psychiatry who are critical of the meteoric rise of mental health awareness. It’s a shocking watch, and one that challenges everything most people accept about mental health in 2019.
We’re getting better at talking about our mental health, and campaigns to destigmatise these issues are becoming more common, but some experts believe that these campaigns could be having unintended negative consequences.
Sami Timimi, a consultant psychiatrist, says the campaigns promote the idea that mental health problems are just around the corner, and that experiencing intense emotions is a sign that something is wrong: “I think that is a very unhelpful cultural message.” As a specialist who works with children and teenagers, he knows there are young people in crisis who do need professional support but, he says, perhaps controversially, that we must help young people understand that growing up is hard, that we are resilient, and that we can get through difficult periods in our lives.
Clinical psychologist Lucy Johnstone, holding a young people’s mental health awareness cartoon from charity Mind, is also concerned that branding emotional problems as illness is preventing us from tackling the real causes. She finds it upsetting that these campaigns are persuading young people to take on a ‘mental illness narrative’. “Instead of asking ‘what’s wrong with me?’, ask ‘what’s happened to me?’” she says.
Labels and diagnoses aside, we need a healthcare system that recognises and acts on young people’s distress. Campaigns are encouraging young people to reach out about their mental health, but once they’ve plucked up the courage, the support is not always there — something that is known all too well by 18-year-old Parveen, whose five- to six-month wait for talking therapy left her no option but to accept antidepressants from her GP.
Antidepressants should be prescribed for young people only after assessment by a psychiatric specialist, and alongside psychological support. Dispatches surveyed 1,000 GPs to find that 39% of GPs would prescribe antidepressants to people under the age of 18 years, but only 1% thought they were the best option. With practice pressures and long waits for therapy, what else are GPs to do?
A great deal, suggests mental health researcher James Davies, who says that young people are not been given enough information about the withdrawal symptoms of antidepressants. National guidelines suggest these symptoms are mild for most and resolve within a week, but Davies’s research concluded that they are far more common, severe and long-lasting than we thought.
‘Young, British and Depressed’ sends a strong message that we must move away from a system that is too quick to medicate young people’s problems, to one that promotes their wellbeing and helps them work through the causes. But it slightly shies away from saying what CAMHS are crying out for: funding.
Teenager Parveen made the dire need for access to psychological support clear: “For me, it was just someone to talk to. But there was no one to talk to.”
‘Young, British and Depressed’ is available for streaming on All4 at: https://www.channel4.com/programmes/dispatches/on-demand/69735-001
References
Dispatches. Young, British and Depressed. London: Channel 4; 2019


