JL / The Pharmaceutical Journal
The home secretary Sajid Javid has announced that medical cannabis can be prescribed for patients from 1 November 2018; however, pharmacists should not expect to be deluged with prescriptions immediately. Unlike the scenes in Canada, where cannabis was decriminalised completely on 17 October 2018, there will be far stricter controls in the UK.
The drug has not been legalised. The regulations are clear that only cannabis-based medical products will be moved into Schedule 2 of the Misuse of Drugs Act 2001 regulations, meaning that possession, supply and procurement is authorised for pharmacists. Before this happens, the Department for Health and Social Care and the Medicines and Health products Regulatory Agency need to agree on a clear definition of what constitutes a cannabis-derived medical product, so they can be given marketing authorisations and prescribed.
Consultants will be able to prescribe cannabis-derived medical products as ‘specials’ and patients will be able to get access to them through clinical trials of a new medical product but, apart from that, any other form of cannabis will be illegal.
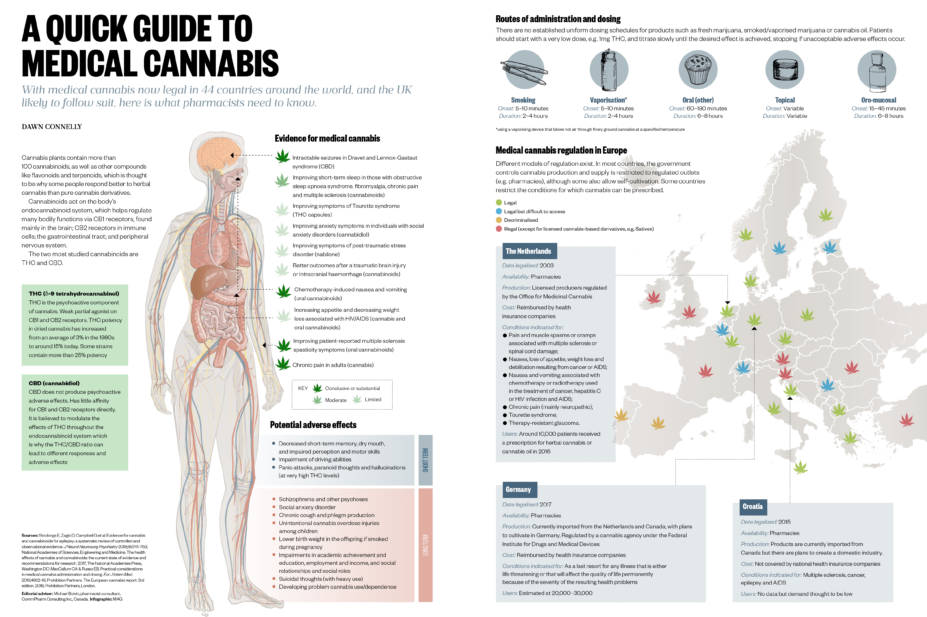
There is only one cannabis-related medical product approved in the UK — Sativex, manufactured by UK-based firm GW Pharmaceuticals. This was licensed almost ten years ago for treating spasticity in multiple sclerosis, but has not really made a mark after the National Institute for Health and Care Excellence (NICE) refused to recommend its use on the NHS on cost grounds. Epidiolex, also manufactured by GW Pharmaceuticals, has been approved by the US Food and Drug Administration for use in the United States and is passing through the European Medicines Agency authorisation process. But because it contains virtually no tetrahydrocannabinol (THC) — the main psychoactive compound in cannabis — it is exempt from scheduling regulations.
This dearth of licensed medical cannabis products is not likely to last long. At this year’s Pharmacy Show, held on 6–7 October 2018 at the NEC Birmingham, the number of stalls touting cannabis-related products was rivalled only by Falsified Medicines Directive ‘solutions’. Returning delegates at the show were heard to compare the situation with the ubiquitous vaping sales force present a few years ago.
There are various forms of cannabis oils legally available in the UK that do not include THCs, and the Cannabis Trades Association estimates that as many as 250,000 people currently use them. Even Hollywood actor Gwyneth Paltrow, also known for her staunch advocacy of ‘wellness’, has said she sometimes uses cannabidiol (CBD) oil to help her sleep.
The publicity around the Billy Caldwell case is likely to drive sales of CBD oils, but the public is entirely confused about what they can and cannot buy, or get prescribed, and what does or does not work for their condition.
The widest-reaching source of information on the subject is probably the internet and its main providers are entirely unregulated online sellers. NICE guidance on medical cannabis is not expected until at least October 2019, meaning that healthcare professionals will be none the wiser about indications, dosing or precautions when prescribing medical cannabis. This presents a real opportunity for pharmacy to take the lead on how these medicines are introduced in the UK.
In Canada, medical cannabis has been available since 2001. Initially only patients with a terminal illness, or another serious medical condition could receive it, but the law was relaxed over time and 269,000 Canadians were using medical cannabis by the end of 2017. The drug has now been legalised for recreational use in the country, but both the medical and pharmacy professions were opposed to its use at first. Professional bodies, including the Canadian Medical Association (CMA), even lobbied against its prescribing and dispensing and, consequently, the government allowed patients to buy medical cannabis directly from the producer, cutting out pharmacists completely.
This is not true for healthcare bodies in the UK. The Royal Pharmaceutical Society has been very supportive of the rescheduling of medical cannabis and is working on guidance for pharmacists. The regulations have been written in such a way that pharmacists will be the sole supplier. There is an opportunity here for pharmacists to develop the expertise to educate others on the effective use of the various forms of medical cannabis and fill the knowledge vacuum that currently exists as new cannabis-based medical products come on to the market. This change has offered a real chance to put pharmacy at the forefront of a new and exciting development in patient care once again.


