Zephyr / Science Photo Library
On 11 December 2017, Ionis Pharmaceuticals announced successful results from a Phase I/IIa trial of their drug IONIS-HTTRx, which is injected through the spinal canal and targets the underlying cause of Huntington’s disease (HD). IONIS-HTTRx, an antisense oligonucleotide (ASO), interferes with the translation of genetic information (mRNA) to the disease-causing protein: huntingtin (htt).
According to Ionis, the treatments were safe and tolerable, and caused a measurable dose-dependent reduction in the concentrations of htt within cerebrospinal fluid (CSF). The results made the headlines, and Roche has exercised an option to license the treatment for further development. This is very promising news. But I must caution that this is just one step in a chain of clinical-trial testing; the drug has not yet shown (nor has it had a fair chance to show) that it is an effective clinical treatment for HD.
Pathology of Huntington’s
Huntington’s disease is a devastating familial neurological disease that is caused by a single autosomal dominant genetic mutation. The mutation comprises an elongation of a trinucleotide repeat chain in the coding DNA for the (htt) protein. This abnormally long trinucleotide chain is variable in length, which influences the age of the disease’s onset and severity.
Onset of clinical illness typically occurs in midlife and is characterised by movement disorder, cognitive loss, and behavioural and psychiatric symptoms, such as extremes of apathy and agitation. It is a slowly developing but unrelenting disease, and patients typically experience one to two decades of persistent decline before death. There are currently no disease-modifying treatments for HD.
Identifying the responsible gene
The gene that causes HD was identified in 1993, and there was much optimism that gene identification would shortly lead to effective treatments for this presumably simple one-gene disease.
Htt protein is involved in hundreds of biological pathways within the nervous system and elsewhere
Instead, HD has taught us a sobering lesson regarding the potential complexities of a ‘simple’ disease. Htt is involved in hundreds, if not thousands, of biological pathways within the nervous system and elsewhere. There is a steady stream of new discoveries regarding its biological functions, along with a corresponding stream of hypotheses regarding which of these functions are pathological and vital in the etiology of HD. It has therefore been very difficult to identify the key pathogenic mechanism(s) of action and target them through traditional small–molecule drug development.
Taking a different path
Ionis’s alternative approach is to stop or reduce the levels of the protein itself — doing so has decreased HD-like symptoms in multiple animal models of the disease. Ionis’s ASO is injected into the circulating cerebrospinal fluid, from which it enters the brain and partially blocks translation of the htt mRNA into protein. There are substantial technological challenges involved in designing such an ASO, and in developing an effective method of delivery into the human brain; Ionis has successfully tackled many of these challenges. The safety and potential efficacy of a treatment strategy that directly interferes with htt protein production has also been uncertain. In its success, the Ionis trial answers some (though not all) of these questions.
Learning lessons from animal models
HD is a relatively rare dominant genetic illness, and nearly all people with the disease are heterozygous for the mutation, meaning they have two different copies (or alleles) of a gene. They retain one copy of a normal htt gene, which produces non-mutant htt, alongside the mutant protein that is produced by the other disease-causing gene.
Through animal models, we have known for some time that the presence of normal htt is vital for embryogenesis, the process in which the embryo develops, and non-mutant htt is important, if not vital, for ongoing healthy function in the mature brain, and possibly in other tissues. But Ionis-HTTRX’s action is not specific to mRNA from the mutant allele; normal htt protein is also reduced.
There has been concern that reducing normal htt levels might have unpredictable and potentially serious adverse effects
The level of non-mutant htt required for healthy biological function is unknown, and there has been concern that the concomitant reduction of normal htt levels might have unpredictable and potentially serious adverse effects. Although extensive animal models had suggested that this would not be the case, the issue had not yet been settled in humans. The lack of side effects, to date, in the Ionis trial is a significant outcome and a cause for relief. The level of concern for human safety in a Phase I safety and tolerability drug trial is variable, but, in this case, that concern was non-negligible. (I should note that Ionis designed their safety trial by starting with minimal doses of the ASO and increased the dose only gradually, contingent on a lack of adverse effects at lower doses.)
The trial’s most exciting news
Ionis announced that levels of circulating htt in the CSF were indeed lowered, which strongly suggests that the intended mechanism of action has been accomplished. Beforehand, there was uncertainty over whether a successful reduction of htt within brain cells would even be detectable in the CSF. The concentration of the protein within neurons is much higher than in the extraordinarily small concentrations in the CSF, and the mechanisms establishing equilibrium between the two are not well understood. A failure to lower CSF levels would therefore have been inconclusive and led to a more difficult decision on whether to proceed with further treatment development.
Holding fire on the new therapy
The results have, thus far, been announced only in short press releases and no formal scientific presentations are yet available, so my conclusions must be tentative, but this trial could hardly have had better results. There is good evidence to suggest that the drug’s supposed action has been accomplished and that it does not cause short-term adverse effects.
While this is exceedingly positive news, we have not yet established that the treatment will be of clinical benefit in the treatment of HD. I have seen no claim from anyone connected to the trial that this is the case, although I’ve also not seen many caveats against jumping to this conclusion. Unfortunately, this issue has been obscured in the secondhand reporting that has crossed my inbox. While there is good cause for optimism, Ionis’s ASO therapy has not yet been shown to be an effective clinical treatment for HD.
Concern has been expressed that antisense therapy delivered through the cerebrospinal fluid may not reach deeper brain structures
There was a lag between htt reduction and detectable benefits to motor, cognitive, or psychiatric aspects of the illness, and this lag was reasonably expected. But how long this lag should be is unclear.
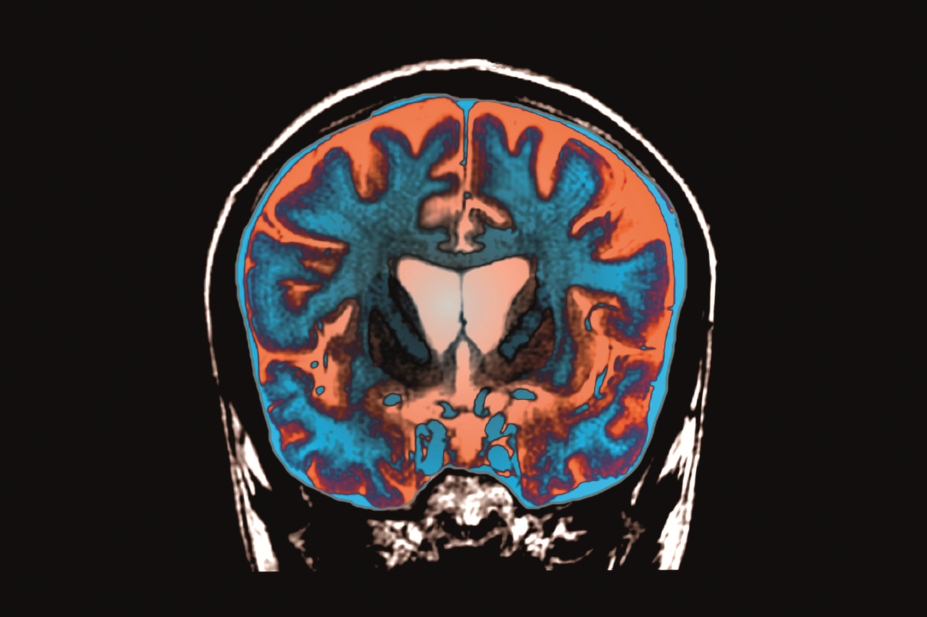
We also cannot be certain that htt is being suppressed sufficiently in important parts of the brain. HD involves dysfunction of multiple brain circuits that connect the cerebral cortex to deeper brain structures, such as the basal ganglia and thalamus. The basal ganglia are especially sensitive to the effects of mutant htt, and some have expressed concern that ASO delivery through the CSF may not reach these deeper brain structures in sufficient concentration. We must therefore be clear that the IONIS-HTTRx trial has apparently been an unqualified success, as evaluated by its reasonable, pre-established goals.
Those goals, however, did not include an expectation that clinical efficacy would be shown during these early phases of human testing. Such a conclusion, positive or negative, must await larger and longer definitive Phase IIb and III trials. Ionis has won a very big battle, but the war is not yet over.
Professor Douglas Langbehn is a professor of psychiatry and biostatistics at the University of Iowa Carver College of Medicine. He has been a frequent research collaborator with Professor Sarah Tabrizi, who led the IONIS-HTTRx trial, but he was not involved in its design, conduct, or analysis. He will receive institutional support from a Wellcome Trust grant awarded to UCL to perform secondary scientific analyses of data collected during this trial. Professor Langbehn is or recently has been a paid consultant regarding HD trial research design for Roche, Voyager, and Teva.


