Umeh Ali
Finally! On 2 December 2020, the moment we’d been waiting for had come at last: the UK approved the first ever vaccine against COVID-19, developed by Pfizer and BioNTech.
When we heard the news at the Sowe Valley Primary Care Network (PCN), we sprung into action. There was a palpable buzz in the air as we mobilised our multidisciplinary team into a machine with a singular focus: to get this vaccine out to our 80,000 patients as soon as it was available.
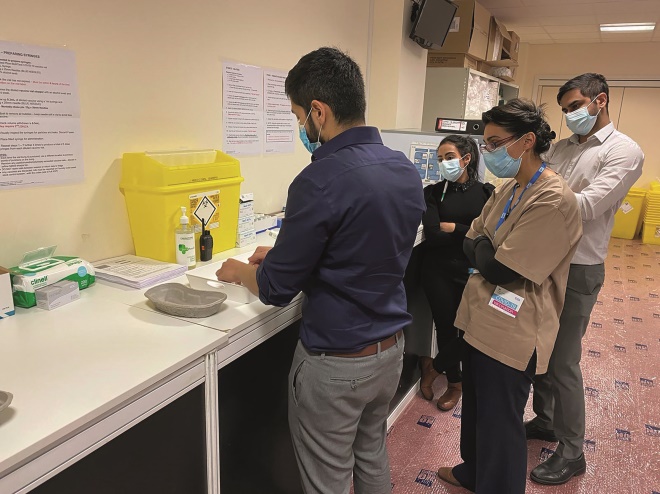
This is where our multidisciplinary team came into its own. From the very start, the work of building a vaccination centre was divided among the different members of the team.
Since starting as a PCN pharmacist in August 2020, I had mainly worked remotely on medicine-related queries from clinicians and structured medication reviews. But my role was transformed overnight: suddenly, I was tasked with coming up with a set of local standard operating procedures (SOPs) and policies for the new vaccine.
This was not easy. I had never had to write SOPs for such a new medicine, with often patchy information from the manufacturer — understandable, given that the vaccine was being rolled out so rapidly.
We came up with a protocol for the storage, handling, drawing up and administration of the vaccine. Luckily, my years of working in community pharmacy and a clinical commissioning group gave me a strong understanding of how flu vaccination services were already being run.
Alongside our team, others planned an appropriate site for the vaccination hub, built the necessary cubicles and drawing-up rooms, as well as waiting areas, and provided refreshments and amenities.
The administration team were tasked with identifying patients who were in categories one and two (those aged 80 years and over, care home residents, and health and social care workers) — who are first in line to receive the vaccine.
Our clinical team, led by the PCN clinical director, created a pathway for these patients to attend the hub and receive the vaccine.
Our PCN paramedic helped implement the anaphylaxis protocols and the practice managers coordinated the various teams, and acted as go-betweens for the project managers.
We delivered our first dose of the Pfizer/BioNTech vaccine at around 15:00 on 7 January 2020: a moment that few of us will forget any time soon. We were all elated, with a sense that the end was finally in sight.
And during our first 10 days, we delivered around 2,500 vaccines to our patients. There have been many highs and lows, but mostly highs, in no small part thanks to an excellent team, who have thought of every potential problem and solved it before it ever came to pass.
But one low point occurred just a few days ago, when an elderly patient collapsed owing to an unclear cause. This emergency situation necessitated the immediate involvement of the whole team. Our on-site paramedic sprang into action and began the basic life support algorithm. This has been formally investigated through an significant event process, but the experience allowed us to test out our anaphylaxis and emergency response process.
I hastily called for an ambulance and relayed all the information they requested. At the same time, our social prescriber swooped in to provide comfort and support to the patient’s family member, who was watching from nearby.
The paramedic and I supported one another with drug delivery and clinical assessment. We managed to stabilise the patient until the ambulance crew arrived and took over, speeding off to the hospital for further treatment. This was my first real-life experience of possible anaphylactic shock and it will stay with me for as long as my memory will serve.
But this was an isolated case. Some people have been worried about adverse effects and potential long-term problems, but not enough to dissuade them from taking up the vaccine. We strive to provide each patient with as much information as possible and address their individual concerns to the best of our ability.
So far, our patients have been extremely grateful to us for bringing them, as one lady put it, a lifeline. It has been so rewarding.
But it has also been hard. We faced many challenges; changing delivery dates, in particular, led to problems in allocating our workforce.
The unpredictable schedule has been one of the hardest factors for me, but I have had so much support and flexibility from our whole team.
We’ve now gone live with the Oxford/AstraZeneca vaccine, and the Moderna vaccine is also on the horizon. And I can’t wait to add more medicines to our arsenal.
Umeh Ali, clinical pharmacist, Sowe Valley Primary Care Network, Coventry


