Abstract
Aim
To report on the evaluation of a new vocational learning format “learning@lunch”. The learning@lunch programme is designed for hospital pharmacists and pharmacy technicians to work together during their lunch break to explore clinical topics.
Outcome measures
Participation rates, reasons for participation or non-participation, and satisfaction with different aspects of the learning programme.
Results
Of the original sample of 7,112, 472 had moved address or left the hospital sector, giving a final sample of 6,640. The final response rate was 25.9% (n=1,722). In total, 927 of those who completed the questionnaire (53.8%) had used the programme whereas 795 respondents had not. The most frequently quoted reason (38.8%) for pharmacists not having taken part in learning@lunch was that the trust had not scheduled a session. Lack of time was the reason given by almost a fifth (18.3%) of non-participants, while 10% believed that the topics were not relevant to their skills and experience. Overall, participants in the programme (n=927) were satisfied with the resources available, with 89.7% agreeing that the materials were easy to understand and 76.3% agreeing that the case studies in the modules were relevant to their practice. Most learning@lunch participants (85.8%) agreed that the most recent module they had studied had helped to update their knowledge and skills. A similar proportion (79.4%) of participants thought the programme was of value to clinical practice.
Conclusions
The findings from this evaluation provide valuable insight into participants’ views on learning@lunch and suggest they found the programme relevant and useful to practice. On the whole, those who had participated in learning@lunch were positive about the resources and content available to them.
Healthcare professionals worldwide face continuing pressure to maintain and develop their skills and competences in the face of evolving healthcare technologies. In 2002, the International Pharmaceutical Federation (FIP) approved the use of the continuing professional development (CPD) concept, arguing that it was the responsibility of individual pharmacists to ensure their competence as a health professional remained adequate throughout their career.1 To ensure that patients and service users receive maximum benefit from the treatments and services pharmacists provide, FIP argued that pharmacists must keep up to date with developments in practice, pharmaceutical science, professional standards and pharmaceutical law. CPD has been defined by the Department of Health as “a process of lifelong learning for all individuals and teams which meets the needs of patients, delivers the health outcomes and healthcare priorities of the population, and which enables professionals to expand and fulfil their potential.”2
In Great Britain, CPD has been a requirement of the Royal Pharmaceutical Society’s code of ethics since 2001.3 However, until 2009, mandatory standards for CPD had not been set. Since summer 2009, practising pharmacists and registered pharmacy technicians have been required to make a minimum of nine CPD entries per year.4 At the moment, only a relatively small proportion of pharmacy technicians are registered, but by 2011 all technicians must be registered.5 CPD is also likely to play a major part in arrangements for revalidation, which is due to be in place by 2012. Under these new arrangements registered pharmacists and pharmacy technicians will be required periodically to demonstrate their fitness to practise.6
In England, CPD activities and programmes are provided by several organisations, including the Centre for Pharmacy Postgraduate Education. In 2006, the CPPE launched the “learning@lunch” programme. This initiative was designed for hospital pharmacists and registered pharmacy technicians, working together in small groups, to explore clinical topics. The programme takes the form of self-directed reading from booklets provided by CPPE, plus an hour-long workshop session, facilitated by a member of the hospital team. Participants are encouraged to work through the case studies contained in the programme. The sessions are intended to take place during a lunch break.
The first series of learning@lunch covered cardiovascular disease and consisted of three modules: acute coronary syndromes; secondary prevention; and stable angina. Subsequent series have been produced on smoking cessation, palliative care and diabetes. Initial feedback from the pilot suggested that hospital pharmacists found the programme useful and interesting.7
Aim and objectives
The aim of this study was to explore the uptake of learning@lunch among hospital pharmacists and pharmacy technicians in England. The objectives of the evaluation were to explore how participants chose to study the programme, to explore satisfaction with the modules chosen and to determine the usefulness of the scheme for day-to-day practice. This paper will report on the data regarding participation, take-up and satisfaction with the programme.
Method
The evaluation involved self-completion of a questionnaire that was sent to all pharmacists who had registered with the Royal Pharmaceutical Society as working in the hospital sector in its 2005 workforce census (n=6,219).8 Approval for using the census data to identify pharmacists was obtained from the Society. These data were cross-referenced with the CPPE database to ensure that all pharmacists working in hospitals were identified — most notably, those who had first registered after the 2005 census was carried out.
The questionnaire was also sent to hospital pharmacy technicians, who were identified through the CPPE database (n=893). Ethical approval was granted by the University of Manchester Senate Committee on the Ethics of Research on Human Beings. Since the study was an evaluation of an existing service, NHS ethical approval was not required.
The questionnaire included questions relating to awareness of the learning@lunch programme, participation in the programme, satisfaction with programme content and its usefulness. Participants were asked to score their agreement with a series of statements on a five-point Likert scale. The statements were divided into three main sections: content and resources; the facilitated learning@lunch session; and the usefulness of the programme. The data are reported here in terms of agreement, ie, the percentage of respondents “agreeing” or “strongly agreeing” with a statement. Several open questions were also included, but the results of these responses are not reported here.
The questionnaire was piloted with 12 practising hospital pharmacists and several pharmacists who were working in academia and hospital, all of whom were invited to comment on its content. Minor changes were made to the questionnaire as a result. All studied pharmacists and technicians were given a paper copy of the questionnaire, but were also invited to complete it online. Each member of the sample was given a unique token number to prevent duplicate responses.
The data from the questionnaires were entered into and analysed by computer programme SPSS (version 14). The analysis explored the influence of personal and hospital characteristics on awareness and uptake of learning@lunch. Statistical tests used included chi-squared for categorical variables and t-tests and one-way ANOVA for scale variables. The significance level was set at 5% (0.05).
Results
A total of 1,722 usable responses were received, of which 1,470 were from hospital pharmacists (23.6% of potential respondents) and 250 were from hospital pharmacy technicians (28.0% of potential respondents). Two individuals removed their identifying numbers from the questionnaire, which meant it was not possible to determine whether they were hospital pharmacists or pharmacy technicians. Most respondents (94.3%) completed the paper version of the questionnaire. The overall response rate was 24.2% (1,722 of 7,112).
Excluding those who had left their registered address or were no longer working in hospital pharmacy (n=472) gave an adjusted response rate of 25.9% overall and 25.4% and 29.6%, respectively, for pharmacists and pharmacy technicians.
Characteristics of respondents
The characteristics of respondents are shown in Box 1. Over half of the overall sample was female. The mean age of respondents was 40 years (range 24–70 years). In total, 927 respondents (53.8%) had used the learning@lunch programme in some way — of whom 838 were pharmacists and 88 were pharmacy technicians. One learning@lunch participant had removed his or her ID number so could not be identified as a pharmacist or pharmacy technician. Pharmacists were significantly more likely to have used the programme than technicians (57.0% vs 35.2%; P<0.01).
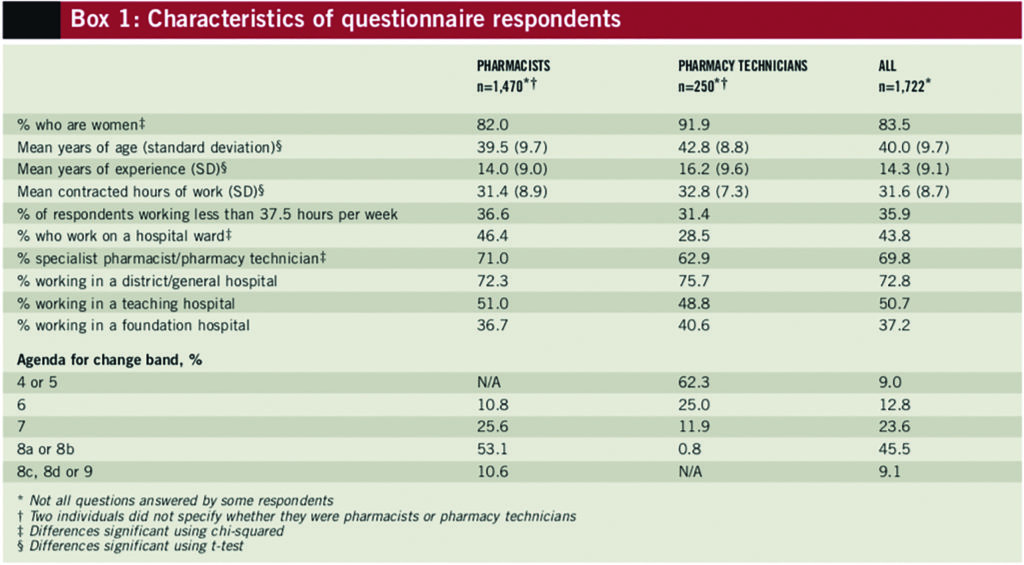
There were no statistically significant differences between participation and non-participation in learning@lunch according to gender. Participants were younger than non-participants (39 years vs 41 years; P<0.01). Full-time employees (>37 hours per week) were more likely to have participated in learning@lunch than those working part-time (66.8% vs 61.0%; P<0.05) and those working in district general hospitals were more likely to have participated than those working in specialist hospitals (58.4% vs 46.0%; P<0.01). Participation rates for learning@lunch were higher for pharmacy staff who described themselves as ward-based than their non-ward-based counterparts (64.2% vs 45.6%; P<0.01).
Reasons for participation
Questionnaire respondents who had taken part in learning@lunch were asked a closed question with pre-defined answers regarding their reasons for participating. The most commonly cited reasons for using the programme were for professional development (55.7%) and to gain additional skills in the workplace (18.0%). Some participants (17.0%) reported that they had attended a learning@lunch session simply because their department was running it.
Respondents who had not taken part in learning@lunch were asked a closed question with predefined answers regarding reasons for non-participation. The most frequently quoted reason (38.8%) for non-participation was that the trust had not run any sessions. Lack of time was quoted by almost a fifth (18.3%) of respondents. About a sixth (16.5%) of technicians stated that they had not taken part because the topics were not relevant to their areas of skill — a higher percentage than for pharmacists (9.7%). However, the difference between these results was not statistically significant.
Attitudes
On the whole, respondents were satisfied with the content and resources available through learning@lunch (see Box 2). More than three-quarters of the sample agreed that the case studies were relevant to their practice.
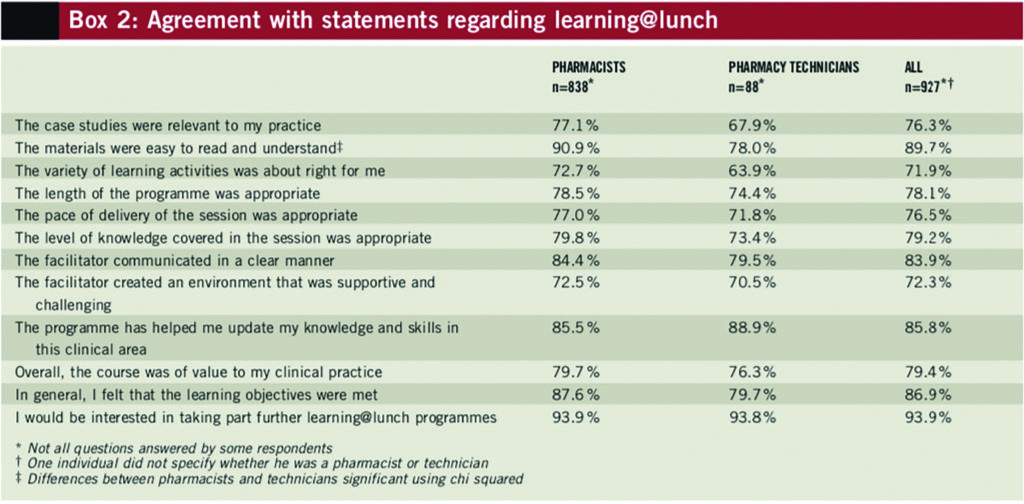
Although overall most respondents found the material easy to read and understand, pharmacists were significantly more likely to agree with this statement than pharmacy technicians. More than two-thirds of participants agreed that the variety of learning activities in the programme was appropriate for them and 78.1% agreed that the length of the programme was appropriate.
The learning@lunch session
The majority of learning@lunch participants agreed with the four statements regarding the learning@lunch session itself (see Box 2). In terms of pace of delivery, over three-quarters of participants agreed that it was appropriate. They also showed high levels of agreement (79.2%) regarding the level of knowledge covered in the facilitated session. The statement that recorded the highest level of agreement (83.9%) was “the facilitator communicated in a clear manner”. Most respondents also agreed that the facilitator created a supportive and challenging environment for the session.
Usefulness of learning@lunch
Participants recorded high levels of agreement for the four statements regarding the usefulness of learning@lunch. The majority (85.8%) agreed that learning@lunch had helped them to update their knowledge and skills in particular clinical areas and four out of five believed that learning@lunch was relevant to their practice. Most participants agreed that the learning objectives of the programme had been met. The statement that recorded the highest level of agreement (93.9%) was “I would be interested in taking part in further learning@lunch programmes”.
Discussion
The paper presents the results of an evaluation of a new vocational learning format, introduced by the CPPE in 2006. More than half of those who had participated in learning@lunch did so for their professional development, suggesting that the programme is relevant to the professional development of pharmacists and technicians. Earlier research, which explored attitudes towards CPD, found that the role of the department head was key in introducing CPD in the workplace and went as far to suggest that “the infrastructure within which people work can be both a catalyst and a barrier to CPD activity”.9
This seems to be the case in the learning@lunch study; the main barrier to participation noted by the non-participants was that their employer had not scheduled any learning@lunch sessions. In contrast, almost one in five pharmacists was prompted to participate in the programme simply by the fact that their employer was running a session, rather than any strong internal desire to improve their skills or develop their career. The findings from this study suggest that the main barrier, as in many previous studies exploring CPD in pharmacies, was lack of time.10–12
Participation rates were higher among those working in general or district hospitals than those working in specialist trusts (eg, mental health hospitals). This tallies with a previous analysis of the orders received by the CPPE for learning@lunch modules, which found much lower uptake among specialist hospitals.13 This is despite the fact that the learning@lunch modules have been targeted at pharmacy staff working in any patient-centred hospital.
The results of the series of statements regarding learning@lunch suggest that overall participants were satisfied with the:
- Relevance of the content
- Ease of understanding the materials
- Variety of the learning activities
- Length of the programme
- Pace and delivery of the session
- Learning environment created by the facilitator
The relevance of content is important since it has been identified previously as a key facilitator for involvement in CPD activities.16 In the learning@lunch evaluation, 90% of those who took part thought that the activities were relevant to their practice.
There was some evidence to suggest that pharmacist participants found the material contained in learning@lunch easier to understand than did pharmacy technicians. Some participants suggested that it was difficult to pitch the programme to meet the learning needs of both groups. However, on balance, both pharmacists and pharmacy technicians reported high levels of satisfaction with many aspects of the programme.
Most participants said that the programme had helped to update their skills and knowledge and they had found the courses of value to their clinical practice. More than 90% of those who participated were keen to undertake further learning@lunch activities.
For the CPPE, the evaluation results have impacted on the development of the learning@lunch programme, resulting in changes to the design of the module booklets, reformatting of questions and the provision of additional training sessions for facilitators. Recommendations for future topics were provided by participants and have been used to inform discussions about the programme’s future content. Data from the evaluation were also used to inform the conception of a new CPPE learning programme called “Focal point”.
Limitations
The response rate to the questionnaire, for both pharmacists and pharmacy technicians, was disappointing. There are a number of possible reasons for this low response. One explanation could be that pharmacists and technicians who had not participated in learning@lunch may have believed that the questionnaire had little relevance to them and therefore chose not to respond. Familiarity with the survey topic has been shown to be an important predictor of response.14 It is also possible that the length of the questionnaire (eight pages) might have discouraged some potential respondents from taking part.
There is some evidence to suggest that male pharmacists and those aged between 21 and 29 years are under-represented in the sample.8 This should be taken into account when considering how generalisable the findings of the evaluation are.
Conclusion
The findings from this evaluation provide valuable insight into participants’ views on learning@lunch and suggest that those who took part found the programme relevant and useful to their practice. The uptake rate for the programme among those who responded to the questionnaire was around 53%, and was lower among those working in specialist hospitals. This is a significant finding because learning@lunch is designed to provide core information relevant to all hospital pharmacists and technicians, regardless of setting.
Since the programme has now been running for over three years, further research could be conducted to determine whether uptake has improved and whether changes made to the programme, as a result of this evaluation, have enhanced it.
Declaration of interest
Dr Cutts is director of the Centre for Pharmacy Postgraduate Education. No other financial, commercial, personal or occupational interests declared.
Acknowledgements
The authors thank the following people for their assistance with the evaluation: Janice Mason-Duff, Julie Kennedy, Claire Hallam, Dave Dunning, Sadian Chadburn, Maurice Burns, Vin Felton, Paul Gray, Andrew Wagner, Sarah Willis, Mike Pigram, Nicola Turner, Lindsey Harper, Debbie Armstrong, Steve Williams, Janet Whittam, Helen Potter and those who took part in the pilot. The authors also thank all the pharmacists and pharmacy technicians who took the time to complete the questionnaire.
About the authors
Elizabeth Seston is a research fellow and Karen Hassell is director, both at the Centre for Pharmacy Workforce Studies, University of Manchester.
Christopher Cutts is director of the Centre for Pharmacy Postgraduate Education.
Email: liz.seston@manchester.ac.uk
References
- International Pharmaceutical Federation. Statement of professional standards: continuing professional development. September 2002. www.fip.org/www/ uploads/database_file.php?id=221&table_id= (accessed 23 April 2009).
- Department of Health. A first class service: Quality in the new NHS. July 1998. www.dh.gov.uk (accessed 23 April 2009).
- Royal Pharmaceutical Society of Great Britain. Code of ethics for pharmacists and pharmacy technicians. London: Royal Pharmaceutical Society of Great Britain; 2007.
- Pharmacists must make nine CPD records per year. Pharmaceutical Journal 2009;282:149.
- Royal Pharmaceutical Society of Great Britain. Pharmacy technicians. www.rpsgb.org/ acareerinpharmacy/pharmacysupportstaff/ pharmacytechnicians.html (accessed 23 April 2009).
- Royal Pharmaceutical Society of Great Britain. FAQs: CPD requirements. www.uptodate.org.uk/faqs/Requirements.shtml (accessed 3 May 2009).
- Gross Z. Learning at lunch — new CPPE programme for pharmacists. Hospital Pharmacist 2006;13:93–4.
- Hassell K, Seston EM, Eden M. Pharmacy workforce census 2005: Main findings. London: Royal Pharmaceutical Society of Great Britain; 2006.
- Swallow V, Clarke C, Iles S, et al. Work based, lifelong learning through professional portfolios: Challenge or reward? Pharmacy Education 2006;6:77–89.
- Mottram DR, Rowe P, Gangani N, Al-Khamis Y. Pharmacists’ engagement in continuing education and attitudes towards continuing professional development. Pharmaceutical Journal 2002;269:618–22.
- Swainson D, Silcock J. Continuing professional development for employee pharmacists: A survey to compare practice in the hospital and community sectors. Pharmaceutical Journal 2004;272:290–3.
- Wilson V, Schlapp U, Davidson J. Prescription for learning? Meeting the development needs of the pharmacy profession. International Journal of Lifelong Education 2003;22:380–95.
- Schafheutle EI, Noyce PR, Cutts C. Hospital trust engagement with a new vocational learning format for pharmacists and technicians. International Journal of Pharmacy Practice 2009;17:243–7.
- Groves RM, Presser S, Dipko S. The role of topic interest in survey participation decisions. Public Opinion Quarterly 2004;68:2–31.


