Abstract
Objective
To identify the proportion of patients receiving paracetamol inappropriately via the IV route, determine trends for inappropriate administration, and identify effective changes that maximise its safe and effective use.
Methods
Data were collected by pharmacists during their usual ward rounds. All patients receiving IV paracetamol for their morning (8am) dose were included. Data collection was for two distinct periods, 10 working days each, occurring in October 2007 and October 2008.
Results
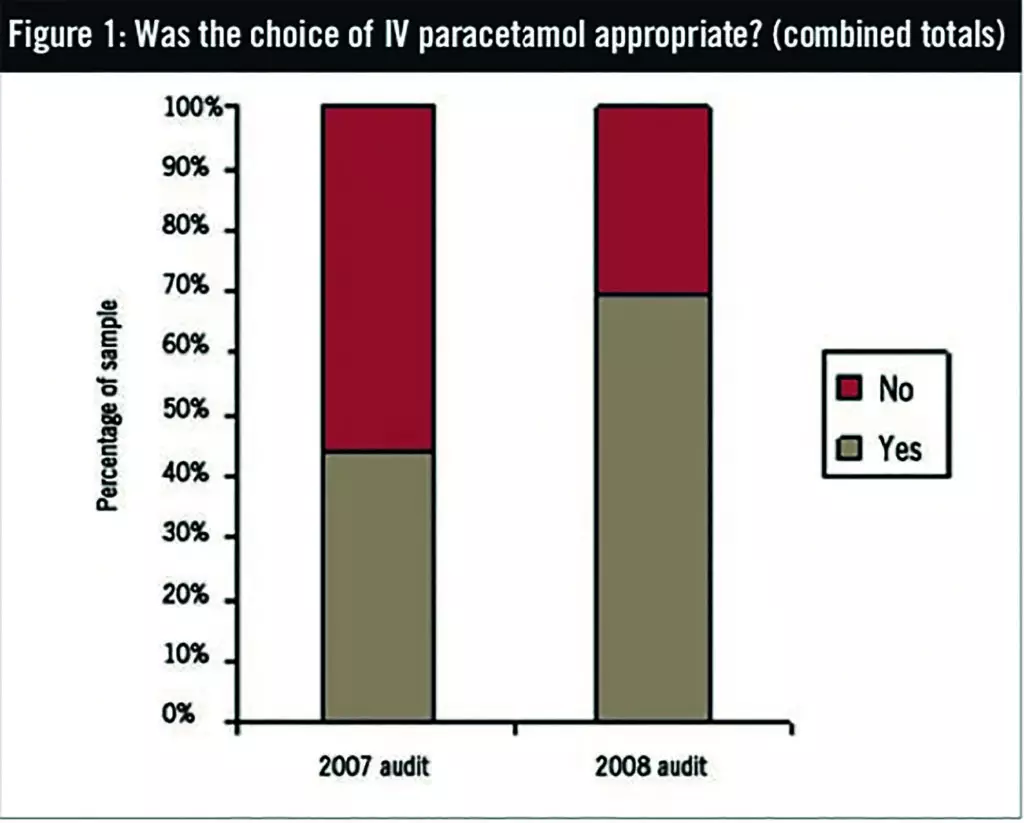
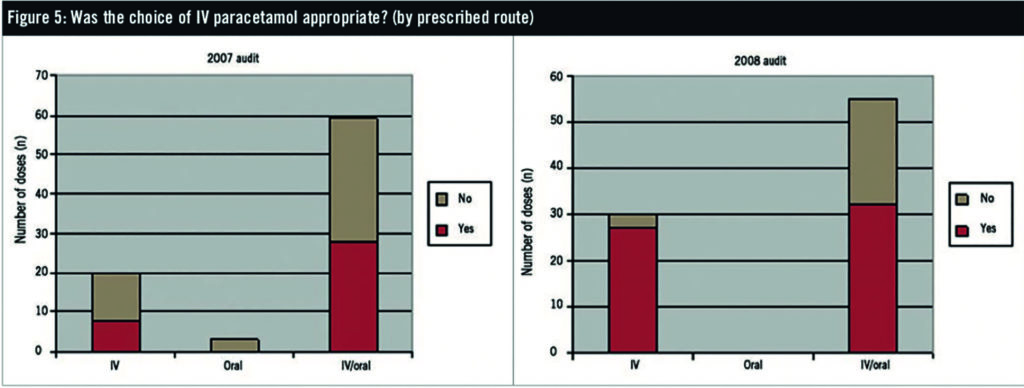
During the October 2007 data collection period, 82 IV paracetamol doses were identified, of which 44% were appropriate. The subsequent audit in October 2008 had an 85-dose sample size and 69% appropriateness.
Conclusion
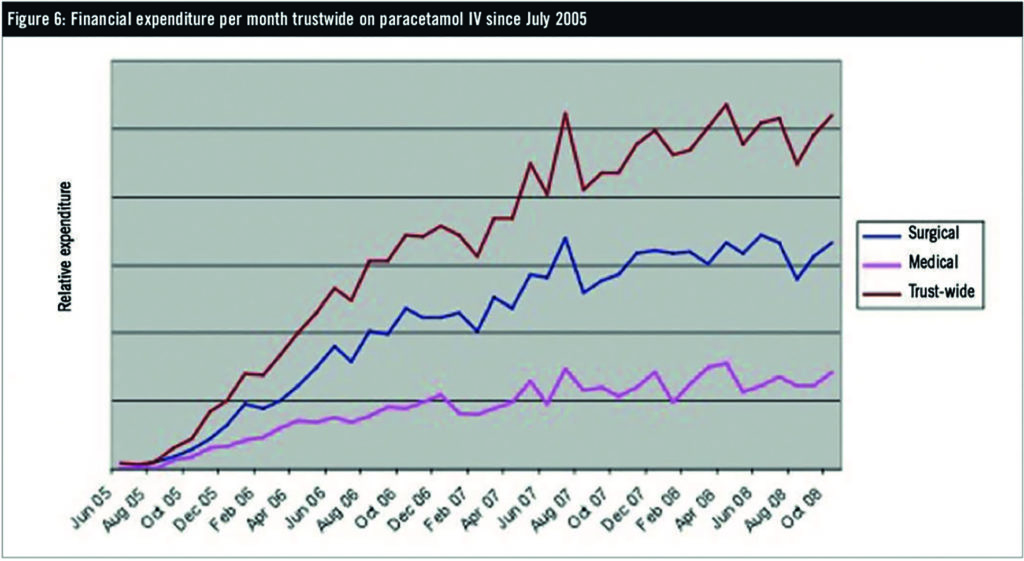
With regular reviews, education and heightened professional awareness, inappropriate use of paracetamol IV can be reduced. Nevertheless, overall expenditure on IV paracetamol continues to rise.
In October 2007 an audit was designed and carried out to determine whether intravenous (IV) paracetamol was being used appropriately in the surgical division and intensive care unit at Portsmouth Hospital NHS Trust (PHT). The primary objective of this audit was to determine whether rising expenditure on IV paracetamol could be justified. Standards were drawn up based on PHT’s existing business case for IV paracetamol,1 which was written following extensive consultation between pharmacy and leading trust clinicians, and in consideration of the best available clinical evidence. These standards defined IV paracetamol as being appropriate only if the oral route was unavailable (where there is a post-operative ileus, upper gastrointestinal tract obstruction), absorption was erratic, the patient could not swallow, or the patient was actively vomiting. Rectal administration of paracetamol was discouraged in adults due to high costs, patient preference, and poor bioavailability.2–5 Administration of IV paracetamol perioperatively or 48 hours after surgery was considered acceptable.
After two weeks of data collection, 82 doses of IV paracetamol were recorded and it was identified that 56% of these were given inappropriately, which when factored into the annual spend for the drug indicated a potential £52,000 saving per annum for 100% standards compliance. Recorded usage varied significantly between different clinical areas. Intensive care and the head and neck unit saw the highest proportion of use, closely followed by the other general surgical areas. Use on orthopaedics was limited. Intensive care demonstrated the highest compliance with standards (61% of 23 sampled doses), and the head and neck unit the lowest (8%). The presence of an IV/oral dosage route choice on the chart, allowing a nurse to choose between oral or IV paracetamol at the time of administration, did not affect the appropriateness of IV usage.
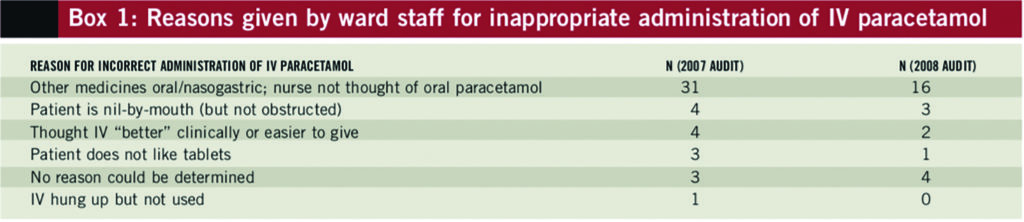
When questioned, nurses were concerned about swallowing difficulties but were not aware of alternative preparations that could be given down nasogastric (NG) tubes, such as soluble tablets or suspensions. It was found that 63% of all inappropriate doses were given to individuals who were taking other medicines orally or via an NG tube.
The findings of this audit were presented to anaesthetists, consultants and nurses. All ward stock lists were amended to ensure that alternative oral dosage forms (as liquids or soluble tablets) were available. Another audit was commissioned one year later to determine whether standards had improved, the findings from which are presented in this paper.
Clinical usage
Paracetamol is available within PHT for administration by oral, rectal and IV routes. The bioavailability of IV paracetamol is greater than the estimated 63–89% bioavailability in adults of oral preparations and the unreliable 24–98% availability of rectal preparations.2–6 Peak plasma concentrations are achieved approximately 45 minutes after a 1g oral dose and approximately 25 minutes after a 1g IV infusion.5 The addition of paracetamol to morphine patient-controlled analgesia (PCA) following major surgery has been shown to reduce postoperative morphine use by 20%, with good tolerance and few side effects.7
The use of IV paracetamol, however, brings with it significant risks of line infection associated with all IV preparations.8 This risk increases with each manipulation of the line, so reducing unnecessary infusions will reduce infections. Cost issues are also important, since a 1g dose of IV paracetamol is currently 250–300 times more expensive than the oral equivalent.
Objectives
The objectives of this work were:
- To identify and record details of patients being administered IV paracetamol and determine whether patients were receiving it appropriately
- To identify reasons for incorrect IV administration, thus identifying changes that rationalise the use of IV paracetamol
- To compare the results of successive audits to determine whether educational interventions have reduced inappropriate use
Standards
National guidelines do not exist for the use of paracetamol IV. Its use, however, needs to fall within the PHT business case1 for paracetamol IV and evidence-based best practice. This is as follows:
- Patients should receive oral paracetamol, except: when the oral route is unavailable; where the patient is not receiving any medicines/fluids/feed orally or via an NG/percutaneous endoscopic gastrotomy/jejunoscopy tube, has poor intestinal absorption, swallowing difficulties, or is vomiting
- IV paracetamol can be given in the surgical setting, but it should only be used perioperatively and/or 48 hours after surgery
- Being nil-by-mouth alone is not a valid reason for initiating IV paracetamol
Any other rationale given for administering IV paracetamol was considered inappropriate.
Methods
Auditing was carried out at the Queen Alexandra Hospital in Portsmouth, on the orthopaedic trauma wards, general surgical wards, head and neck unit, surgical high care unit, children’s surgical ward, surgical admissions unit, and intensive care unit. All patients on these wards administered IV paracetamol were included in the audit. There were no exclusion criteria.
Data collection was carried out for approximately two working weeks using a purpose-designed data collection form. This form was completed by the ward pharmacist.
To reduce investigative load on individual pharmacists, the only data collected pertained to the 8am dose on days of data collection. No data were collected on weekends due to service level restrictions. All data were collated and entered into a Microsoft Excel spreadsheet.
Results and discussion
During the October 2007 data collection period, 82 paracetamol doses were identified, of which 44% were appropriate. The subsequent audit in October 2008 had an 85-dose sample size and 69% appropriateness. Results from the two auditing periods are summarised graphically in Figures 1–5.
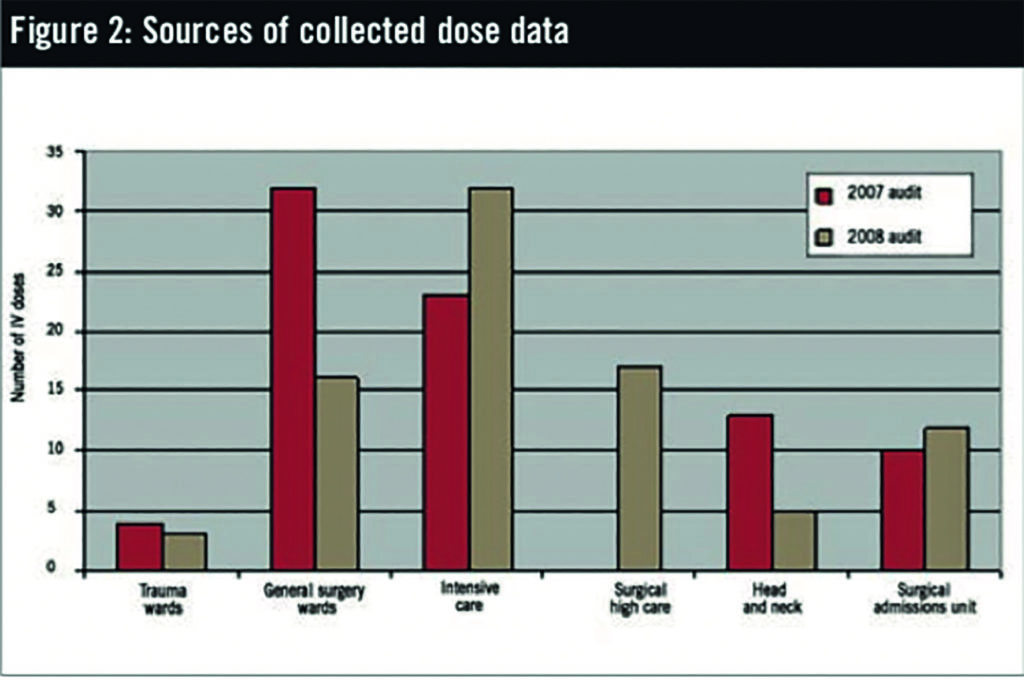
Recorded use has changed between the clinical areas over time. Intensive care remains the highest user with 38% of the 2008 sample data, but use by the general surgical wards has dropped (37% of sample in the initial 2007 audit, dropping to 19% in the 2008 audit). It is, however, hard to assess whether this is significant as a new unit (surgical high care) has opened in the time between the two audits. Head and neck unit usage has decreased (16% of sample in 2007, to 6% in 2008), which may be the result of intensive education of ward staff and high-profile stocking of soluble and liquid paracetamol dosage forms. Use for orthopaedic patients was limited.
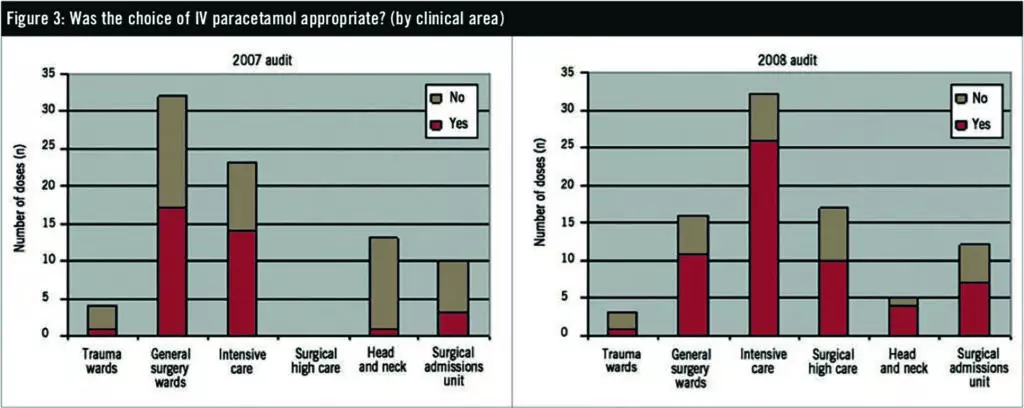
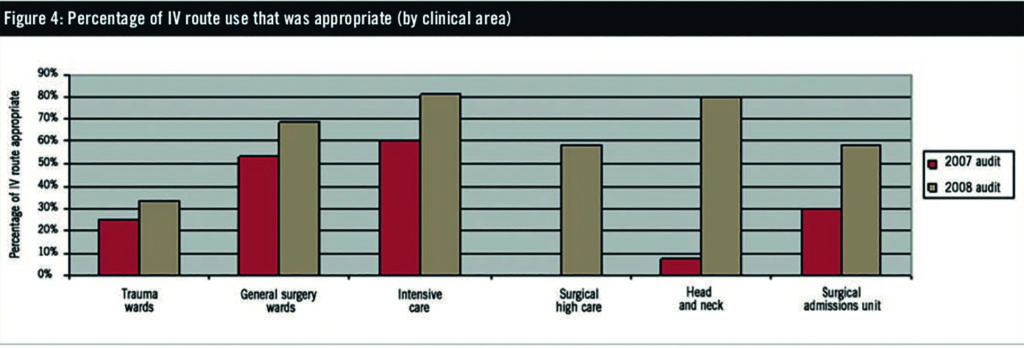
Intensive care consistently demonstrated the highest compliance with standards (81% of 32 sampled doses in the 2008 audit). The head and neck unit showed the biggest improvement over time, with 80% appropriateness in the 2008 audit (five sample doses), compared with 8% in 2007 (13 sample doses). The surgical admissions unit demonstrated the lowest consistent compliance with standards of appropriateness. The 59% compliance rate with surgical high care is also of concern, especially considering that a large proportion of these patients usually fall into categories where IV paracetamol is appropriate, such as postoperative ileus or no oral route. Because this is a new unit for the 2008 year we cannot draw comparisons. Other wards had sample sizes too small for comparison of their compliance rates.
When questioned, nurses are concerned about swallowing difficulties, but rarely consider alternative preparations that can be given down NG tubes, such as soluble tablets or suspensions. This finding is no different between audits, although its prevalence decreased.
In the initial 2007 audit it was determined that stating an IV/oral route option had little impact on the appropriateness of IV paracetamol. In the latest 2008 audit, however, this situation has changed (58% of all doses given IV/orally were appropriate versus 90% written solely as IV). This brings into doubt the role of the IV/oral option, despite its convenience for nurses.
With regard to the reasons stated by nursing staff for incorrect administration of IV paracetamol (Box 1), 62% of inappropriate doses in the 2008 audit were given to individuals who were taking other medicines orally or via NG tube.
Financial analysis
Use of IV paracetamol continues to rise despite improved compliance with prescribing standards and local initiatives (Figure 6). Further education and interventions are needed to reduce inappropriate prescribing. A 100% compliance rate would have reduced local trust expenditure substantially in the 2008 calendar year and placed trust-wide expenditure back below budgeted levels.
Key recommendations
The following recommendations have been identified:
- IV paracetamol should only be used for patients unable to tolerate oral routes. Although evidence demonstrates improved efficacy over oral dosage forms, IV should not be considered in place of stronger oral analgesics such as co-codamol when the oral route is available. Different staff groups should continue to receive pharmaceutical education targeted to their individual situations and clinical expertise.
- Where an IV/oral prescription exists and the patient no longer has any reasonable need for an IV preparation (their condition has improved), the route should be corrected to oral only. This can be done by the ward pharmacist via the trust enabling protocol, and is subject to their professional discretion.
- Use of IV paracetamol for more than 24 hours should be automatically reviewed.
- All nurses administering IV paracetamol against an IV/oral prescription should annotate the drug chart with the administered route in addition to their initial for every dose. Ward pharmacists also need to write “State route of administration” or similar on IV/oral paracetamol prescriptions so that ward staff are reminded to do this at the time of administration.
About the author
Michael Marsden is directorate pharmacist, general surgery, at Portsmouth Hospitals NHS Trust.
Email: michael.marsden@porthosp.nhs.uk
References
- Portsmouth Hospital Trust. Request for change of agent/preparation on the district prescribing formulary (short form application). Paracetamol IV. 2005.
- Holmer Pettersson P, Owall A, Jakobsson J. Early bioavailability of paracetamol after oral or intravenous administration. Acta Anaesthesiologoca Scandinavica 2004;48:867–70.
- Pickering G, Loriot MA, Libert F, et al. Analgesic effect of acetaminophen in humans: First evidence of a central serotonergic mechanism. Clinical pharmacology and therapeutics 2006;79:371–8.
- Sinatra RS, Jahr JS, Reynolds LW, et al. Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology 2005;102:822–31.
- Jarde O, Boccard E. Parenteral versus oral route increases paracetamol efficacy. Clinical Drug Investigation 2007;14:474–81.
- Oscier CD, Milner QJ. Peri-operative use of paracetamol. Anesthesia 2009;64:65–72.
- Peduto VA, Ballabio M, Stefanini S. Efficacy of propacetamol in the treatment ofpostoperative pain. Morphine Sparing effect in orthopedic surgery. ActaAnaesthesiologoca Scandinavica 1998;42:138–45.
- Millen S, Sheikh C. Anaesthesia and surgical pain relief: managing post-operative pain. Hospital Pharmacist 2003;10:442–50.


