Abstract
Aim
To identify (i) the enhanced services primary care trusts had commissioned, (ii) whether the service had been commissioned before the start of the new community pharmacy contract, (iii) the contractual option used, (iv) the number of community pharmacies providing the service and (v) their plans for commissioning in the future.
Design
A self-completion questionnaire.
Subjects and setting
All PCTs in England.
Results
The response rate was 74%. The enhanced services commissioned by most PCTs were supervised administration (88%), needle and syringe exchange (85%) and stop-smoking (77%).
The services commissioned least by PCTs were gluten free foods (2%), home delivery (2%) and schools service (1%).
In terms of the number of community pharmacies providing enhanced services, stop-smoking was the most widespread, provided by 2,118 community pharmacies (36%). 81% of all enhanced services commissioned across all PCTs had been commissioned before implementation of the new contract.
In terms of numbers, stop-smoking was the service commissioned by most PCTs after the implementation of the new contract (43 PCTs). The service with the highest level of commitment to commission in the next 12 months was minor ailments.
Service level agreements were by far the most frequently used contractual arrangement by PCTs (69% of all enhanced services).
Conclusion
The impact of the new contract on enhanced service commissioning levels has been modest. Commissioning of services for substance misuse and smoking cessation are high, mapping onto national priorities for public health.
Since April 2005, primary care trusts have had the option to commission services locally from community pharmacies through the enhanced service tier of the new contractual framework. The enhanced service directions issued by the Department of Health give authority to PCTs to arrange the delivery of 19 enhanced pharmaceutical services if required.1
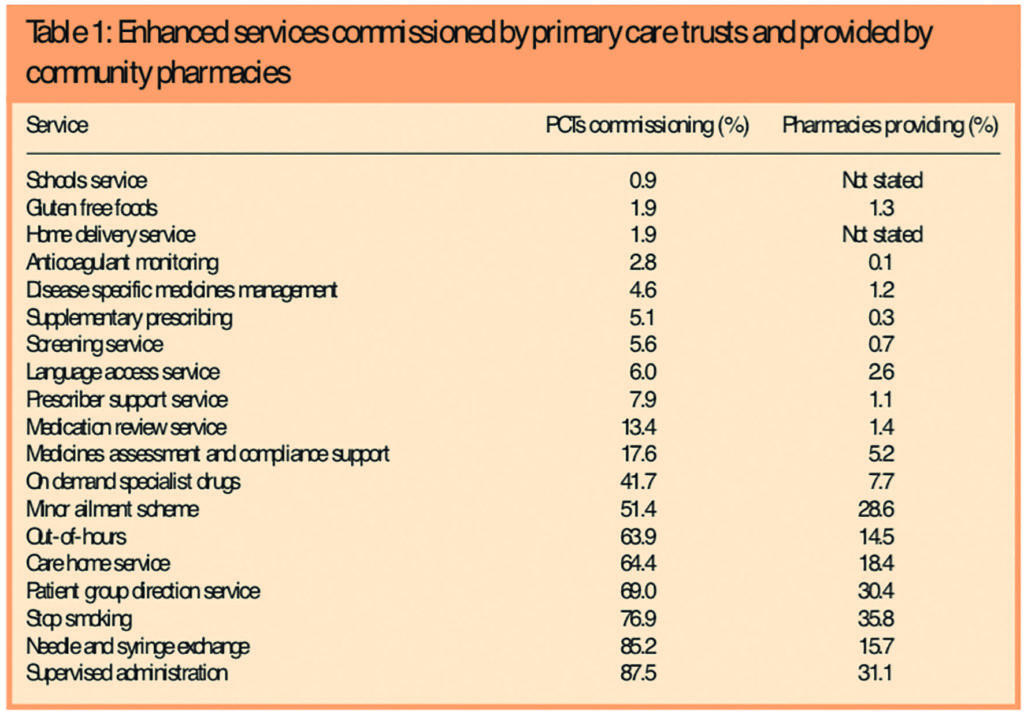
The 19 enhanced pharmaceutical services are listed in Table 1. They focus on areas such as medicines management, public health and improving access.
Enhanced service template specifications are now available for 10 of these 19 enhanced services.2 With PCTs facing major reconfiguration later this year, and with the introduction of practice-based commissioning, the primary care commissioning climate is likely to undergo considerable change.
The first two papers in this series on commissioning pharmaceutical services examined the planning stage of the commissioning process. This paper focuses on the next stage of the process — contracting or purchasing.3 This paper presents a representative picture of enhanced pharmaceutical service commissioning and provision in the first 12 months of the new pharmacy contract.
Method
A pre-piloted questionnaire was distributed to all PCTs in England in March 2006 (n=290). A detailed description of the research method, sample and the topics covered by this questionnaire are provided in the first paper in this series.4
This third paper draws on data from the commissioning of enhanced services section of the questionnaire. Respondents were asked:
- Which of the 19 enhanced services (outlined in the Department of Health directions) their PCT had commissioned
- Whether the service had been commissioned before the start of the new contract
- What contractual option had been used to commission the service — an alternative provider of medical services contract, the new pharmacy contract, a local pharmaceutical services contract, a service level agreement, or “other”
- How many community pharmacies were providing the service
- Whether there were any plans to commission the service in the next 12 months (for those PCTs that had not commissioned the service)
- To provide details of any other services they had commissioned
Data were entered into SPSS v13.0 for analysis and frequency counts and crosstabulation of variables were performed.
Results
Responses were received from 216 PCTs, giving a response rate of 74 per cent. These PCTs covered a total of 7,574 community pharmacies, 77 per cent of all community pharmacies in England in 2006.5
Commissioning of community pharmacy services by PCT
All the PCTs that responded to the questionnaire had commissioned at least one of the 19 enhanced services. The median number of enhanced services commissioned per PCT was six, with a range of between one and 15.
The enhanced services commissioned by most PCTs were supervised administration and needle and syringe exchange, as shown in Table 1. One hundred and eighty-nine PCTs (88 per cent) had commissioned supervised administration and 184 (85 per cent) had commissioned needle exchange services. Stop smoking was the third most popular service, being commissioned by 166 PCTs (77 per cent). One hundred and forty-nine PCTs (69 per cent) had commissioned a service involving a patient group direction, 139 (64 per cent) a care home service, 138 (64 per cent) an out-of-hours service and 111 (51 per cent) a minor ailments service.
The commissioning of medicines management services such as medicines assessment and compliance support, and medication review was found to be low, with only 38 PCTs (18 per cent) and 29 PCTs (14 per cent), respectively, commissioning these. Disease specific medicines management services were found to be even less widespread, being commissioned by only 10 PCTs (5 per cent). The services commissioned least by PCTs were gluten free foods and home delivery, only four PCTs (2 per cent) had commissioned these, and schools service, commissioned by only two PCTs (1 per cent).
Services provided by community pharmacies
Table 1 shows the percentage of PCTs commissioning a service compared with the percentage of community pharmacies providing the service. In terms of the number of community pharmacies providing enhanced services, stop smoking was the most widespread, being provided by 2,118 community pharmacies (36 per cent). The service most frequently commissioned by PCTs, supervised administration, was provided by 1,764 community pharmacies (31 per cent). Despite being the second most popular service commissioned by PCTs, needle and syringe exchange was only provided in 968 community pharmacies (16 per cent).
For 71 per cent of PCTs that had commissioned minor ailments, provision of this service was limited to between 1 and 25 per cent of community pharmacies in their PCT area. Provision was limited to 1 to 25 per cent of community pharmacies for 66 per cent of PCTs commissioning needle exchange and 60 per cent of PCTs commissioning supervised administration. For all PCTs commissioning a care homes service, this was provided by less than 25 per cent of the community pharmacies in their area. Stop smoking was more widespread, being provided in 76 to 100 per cent of community pharmacies in the PCT area for half of the PCTs commissioning this service. Services involving patient group directions had the highest level of provision per PCT, for three-quarters of all PCTs (75 per cent) these were provided in 76 to 100 per cent of community pharmacies in the PCT area. This is unsurprising, however, due to the broad nature of these services.
Other services commissioned by PCTs
Commissioning of services outside the 19 enhanced services was found to be low. Weight management appeared to be the most popular additional service, being commissioned by six PCTs (3 per cent). Three PCTs (1 per cent) had commissioned a pharmacy-led home carers scheme. An emergency/ major incident service, a men’s health check scheme and a free condom scheme had been commissioned by one PCT (0.5 per cent) each.
Commissioning before the new pharmacy contract
Table 2 shows the number of PCTs commissioning enhanced services before and after implementation of the new contract.
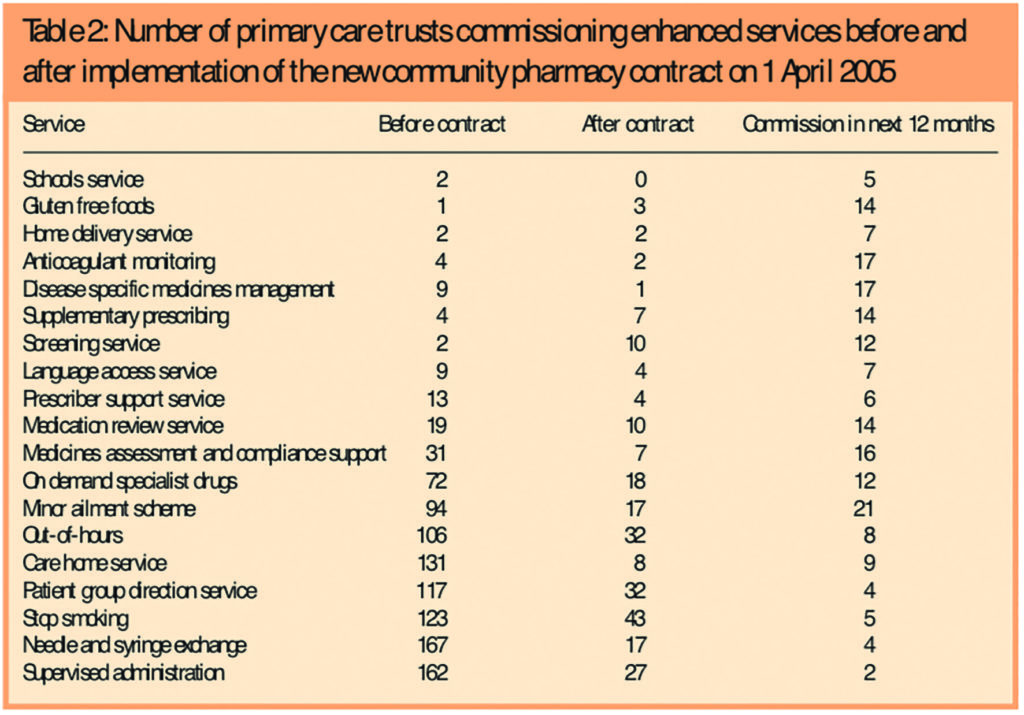
Eighty-one per cent (1,068/1,312) of all enhanced services commissioned across all PCTs had been commissioned before the start of the new contract on 1 April 2005. For 15 of the 19 enhanced services commissioned, over half of the PCTs which had commissioned these services had done so before the start of the new pharmacy contract. Ninety-four per cent of PCTs (131/139) commissioning a care home service had commissioned this service before the new contract, while the corresponding figure for needle exchange services was 91 per cent (167/184). Similarly, 86 per cent (162/189) had previously commissioned a supervised administration service. Both of the PCTs commissioning schools services had done so before the new contract. The services most commonly commissioned after the new contract were found to be screening services, with 83 per cent of PCTs (10/12) commissioning this after the new contract. Seventy-five per cent of PCTs (3/4) commissioned a gluten free foods service and 64% (7/11) commissioned supplementary prescribing after the implementation of the new contract.
In terms of numbers, however, stop smoking was the service commissioned most by PCTs after the new contract (43 PCTs), as Table 2 demonstrates, followed by out-of-hours and services involving patient group directions (both 32 PCTs).
Future plans for commissioning services
Table 2 also profiles commissioning intentions. The service with the highest level of commitment to commission in the next 12 months was minor ailments. Twenty per cent of those PCTs that had not already commissioned this service (21/105) had committed to commission minor ailments in the next 12 months. In percentage terms, this was followed by needle and syringe exchange (13 per cent, 4/32), care home services (12 per cent, 9/77), out-of-hours (10 per cent, 8/78) and stop smoking (10 per cent, 5/50). The services with the lowest level of commitment to commission in the next 12 months were schools services (2 per cent, 5/214), prescriber support (3 per cent, 6/199), language access (3 per cent, 7/203) and home delivery (3 per cent, 7/203). Table 2, however, shows that in terms of PCT numbers, the services with the highest commitment to commission in 12 months, apart from minor ailments were anticoagulant testing and disease-specific medicines management services (both 17 PCTs), and medicines assessment and compliance support (16 PCTs).
Contractual arrangements
Service level agreements (SLAs) were by far the most frequently used contractual arrangement by PCTs for commissioning community pharmacy services. Sixty-nine per cent (724/1,042) of all the enhanced services commissioned by PCTs were provided via an SLA. SLAs were used over and above any other contractual option for 16 of the 19 enhanced services. For the top five enhanced services commissioned by PCTs over 70 per cent of PCTs had contracted these services through SLAs. Ninety-six of the 724 services commissioned using an SLA (13 per cent) were commissioned after the implementation of the new contract.
Discussion
This paper has presented the first national overview of the commissioning of enhanced services by PCTs, following the implementation of the new community pharmacy contract. The results have shown that the commissioning of enhanced community pharmacy services varies widely across PCTs. Substance misuse and smoking cessation services are clearly high on the PCT commissioning agenda, demonstrated by the high level of commissioning for supervised administration, needle and syringe exchange and stop smoking services. Community pharmacy provision varied between individual enhanced services, with some services having only limited provision. It will be important to determine how well this provision meets the needs of local populations.
The recent White Paper, “Our health, our care, our say”, outlines the Government’s plans to shift service provision from secondary to primary and community care and to increase patient access to health care.6 Community pharmacy can potentially play an important role in both these areas.
Improving public health is also high on the Government’s agenda, and the White Paper outlines plans to focus on the prevention of ill health. Previous work has shown the important contribution that community pharmacy can make in improving public health, especially in the areas of smoking cessation and drug misuse.7 It is perhaps not surprising therefore, that these are the areas in which most community pharmacy commissioning has taken place.
Stop smoking appears to be the most rapidly expanding service among community pharmacies; it has the highest level of community pharmacy provision and more PCTs have commissioned this service since the start of the new contract than any other enhanced service. Comparison of these results with findings from an earlier survey of PCTs, conducted in 2003,8 suggest that the commissioning of smoking cessation services from community pharmacy may have increased by 30 per cent during this time. These findings show that community pharmacy is addressing national health priorities to reduce smoking rates set out in the White Paper “Choosing health”9 and also contributing to a number of national service framework aims.10–12
In terms of future aspirations for commissioning, the results suggest that few PCTs are planning to increase their commissioning of pharmacy services over the next 12 months. This is hardly surprising given that many PCTs are facing a period of uncertainty with the impending reconfiguration of PCTs later this year. Previously, we have identified a number of barriers to community pharmacy commissioning such as access to funds, lack of capacity and the impending PCT reconfiguration.13 These factors offer some insight into why new enhanced service commissioning following the implementation of the new contract has not been more extensive.
Minor ailments appears to be the service that will be commissioned by most PCTs in the next 12 months and those services with low levels of commissioning at present may see a small increase in the next 12 months. The top 10 enhanced services commissioned by PCTs map on to the 10 services for which service specifications have been produced, with the exception of patient group directions. Once the remaining nine service specifications have been published, it is possible that commissioning of these services may increase.
Most enhanced services were reported to have been commissioned before the start of the new pharmacy contract on 1 April 2005. Although this survey incorporated the 19 enhanced services outlined by the Department of Health directions, it is clear from the results that most of the services commissioned by PCTs were in fact already in existence before the publication of the directions. These findings indicate that the impact of the new contract on commissioning levels has been modest.
Previously, we have reported that PCT respondents considered the new pharmacy contract to be the most important driver to commissioning community pharmacy services by PCTs.13 Despite this, the level of new enhanced service commissioning through the new contract has been comparatively low. PCTs appear to view the new contract as an important driver to commissioning, but translating this into practice may be more difficult. Further evidence suggesting that this may be a challenging and slow moving process is the finding that although nearly all PCTs had conducted a pharmaceutical needs assessment (PNA) less than half of these (45 per cent) had used their findings to commission services from community pharmacy.4 Approximately 40 per cent of PCTs had not conducted their PNAs before the start of the new contract and, not surprisingly, even fewer PCTs (38 per cent) had commissioned services based on their findings.
Acknowledgements
We thank colleagues in PCTs who put significant effort into providing us with a huge amount of detailed data during a period of considerable turbulence. This study was funded by the Department of Health.
This paper was accepted for publication on 7 August 2006.
About the authors
Fay Bradley, MA (Econ), and Rebecca Elvey, MA (Econ), are research associates, Darren Ashcroft, PhD, MRPharmS, is director of the Centre for Innovation in Practice and Peter Noyce, PhD, FRPharmS, is professor of pharmacy practice at the University of Manchester.
Correspondence to: Fay Bradley, Centre for Innovation in Practice, The Workforce Academy, School of Pharmacy and Pharmaceutical Sciences, University of Manchester, Oxford Road, Manchester M13 9PL (e-mail fay.bradley@manchester. ac.uk).
References
- Department of Health. The Pharmaceutical Services (Advanced and Enhanced services) (England) Directions 2005. London: The Department; 2005.
- Enhanced service specifications. Available at: www.psnc.org.uk (accessed 28 July 2006).
- National Pharmacy Association. Commissioning resource pack. St Albans: NPA; 2005.
- Elvey R, Bradley F, Ashcroft DM, Noyce P. Commissioning services and the new community pharmacy contract: (1) Pharmaceutical needs assessments and uptake of new pharmacy contracts. Pharmaceutical Journal, 2006; 277:161–3.
- The Information Centre. General pharmaceutical services in England 2005–06. Leeds: The Information Centre; 2006.
- Department of Health. Our health, our care, our say: a new direction for community services. London: The Department; 2006.
- Anderson C, Blenkinsopp A, Armstrong M. The contribution of community pharmacy to improving the public’s health. Report 1: Evidence from the peer-reviewed literature 1990–2001. London. PharmacyHealthLink and Royal Pharmaceutical Society of Great Britain; 2003.
- Celino G. Commissioning additional services. What is driving community pharmacy development? Pharmaceutical Services Negotiating Committee Conference 2003. Available at: www.psnc.org.uk (accessed 28 July 2006).
- Department of Health. Choosing health: making healthy choices easier. London: The Department; 2004.
- National Health Service. National service framework for coronary heart disease. London: Department of Health; 2000.
- National Health Service. The NHS cancer plan: a plan for investment, a plan for reform. London: Department of Health; 2000.
- Department of Health. National service framework for older people. London. The Department; 2001.
- BradleyF,ElveyR,AshcroftDM,NoyceP. Commissioning services and the new community pharmacy contract: (2) Drivers, barriers and approaches to commissioning. Pharmaceutical Journal, 2006; 277: 189–92.


