Introduction
Medication errors caused by administration of a drug to which the patient is allergic are recognised patient safety problems and constitute an important preventable adverse event.[1]
,[2]
Reports to the National Patient Safety Agency (NPSA) suggest this occurs most often with antibiotics (penicillins), opioid analgesics and non-steroidal anti-inflammatory drugs (NSAIDs). Although most patients experience little or no harm, such errors have led to a number of deaths in the NHS.[3]
Reducing this type of preventable harm was seen as an NPSA priority, with the NPSA identifying the failure of those prescribing and administering the medication to check any documented allergy status as a contributory factor[1]
.
Acute trusts may have a range of processes to safeguard inpatients from these incidents, including drug charts with a large coloured “allergy box” on the front page, and red alert wristbands for inpatients with allergies to wear.[4]
However, deficiencies in these methods of identification have been reported,[5],[6]
and it is acknowledged that correct identification of allergy status does not protect patients from being prescribed and administered a drug to which they have a documented allergy. Pharmacists have been involved in initiatives (audit, education campaigns) to reduce this type of patient harm.[7],[8]
Local and national[9]
policies recognise a possible lack of knowledge among health professionals relating to safe prescribing in penicillin allergy. For instance, one study[10]
found only 52 per cent of 29 foundation year 2 (F2) doctors and 76 per cent of 38 foundation year 1 (F1) doctors correctly identified antibiotics contraindicated in patients with penicillin allergy; this knowledge gap has been reported for a range of clinical staff.[11]
,[12],[13],[14],[15]
Trend analysis of voluntary incident reports at our organisation of approximately 650 beds over a 12-month period suggests an occurrence of about 28 incidents in which a patient was given a prescribed medicine to which there was documented evidence of allergy, with penicillin antibiotics accounting for about three-quarters of these reports. However, we recognise that this is likely to represent under-reporting of such incidents.
A number of risk minimisation strategies have already been implemented. These include designing materials to promote awareness of which antibiotics may be given to penicillin-allergic patients (displayed on wards), which antibiotics include penicillin (displayed in the drugs trolley), and allergy stickers for drug charts indicating which penicillin antibiotics should not be prescribed. However, these initiatives appear to have had minimal impact on doctors and nurses’ behaviour when measured by tracking incident reports.
As part of a broad initiative investigating how such incidents may be prevented within a teaching hospital we undertook various activities. Stage 1 consisted of a focus group with clinical staff (doctors, nurses and pharmacists) involved in the drug prescribing and administration process to identify where there is potential for such penicillin incidents to arise. Stage 2 consisted of face-to-face semi-structured interviews to explore practitioners’ beliefs and expectations of these incidents and how they could be prevented. Interpretation of the data derived from the two stages was informed by framework analysis[16]
and the findings used to develop an electronic survey instrument that was delivered trust-wide to ascertain staff attitudes and beliefs pertaining to these incidents. We also specifically investigated knowledge among health professionals of prescribing in penicillin allergy. It is the knowledge investigation aspect of the initiative, plus relevant answers from the staff survey, that are reported here.
Method
Knowledge quiz
A structured paper-based quiz to test knowledge gaps about penicillin antibiotics was adapted from elsewhere[11]
and piloted. Staff were asked to state whether 17 named antibiotics used within the trust were safe, contraindicated or could be used with caution in patients with known serious penicillin allergy. The antibiotics were chosen to include a range of classes in addition to examples of drugs identified by the media, the NPSA and the Department of Health as potentially causing confusion due to cross-sensitivity reactions, combination products and branding. A convenience sample of medical, nursing and pharmacy staff was surveyed by pharmacists during March 2011. Staff were asked to complete the quiz in the presence of the pharmacist and without using information sources.
Respondents’ answers were scored according to a set marking scheme written in advance. Data were collated and analysed using Microsoft Excel.
Staff survey
The link to the electronic questionnaire (Survey Monkey), which contained 12 closed questions and a final question inviting free text comments, was emailed to all clinical staff once a week over a five-week period (April to May 2011). The covering email briefly explained the reason for the questionnaire, invited staff to complete it and guaranteed anonymity. The only personal information collected was whether the respondent was a doctor, a nurse or a pharmacist/pharmacy technician.
Results
Knowledge quiz
The quiz was completed by 106 health care staff (40 doctors, 39 registered nursing staff, 12 pharmacists, and 15 year 5 medical students). Results showed that many found it difficult to answer the questions correctly in the absence of reference sources (Tables 1 and 2) and highlighted drugs that are a particular cause for concern. Overall a penicillin antibiotic deemed unsafe according to the literature would or may have been given in 54 instances (7.3 per cent). Meropenem or a cephalosporin would have been given in 117 instances (36.8 per cent). An antibiotic deemed safe to be given to a patient with a history of penicillin anaphylaxis would or may have been withheld in 83 instances (11.2 per cent).
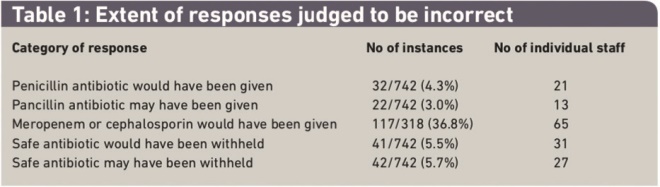
Table 1: Extent of responses judged to be incorrect
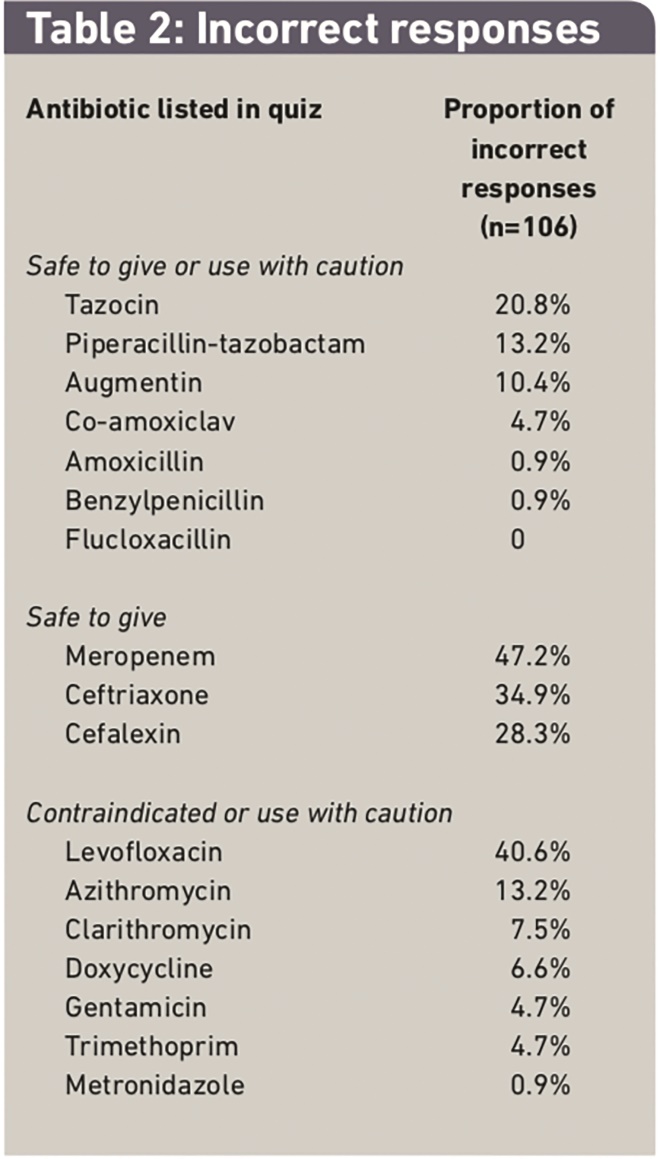
Table 2: Incorrect responses
The individual antibiotics that attracted the most incorrect answers from all 106 staff were meropenem (47.2 per cent), levofloxacin (40.6 per cent) and ceftriaxone (34.9 per cent). Worryingly, combination products (co-amoxiclav and piperacillin/tazobactam as generic or brand name) accounted for 20.5 per cent of all incorrect answers Overall only 29 of the respondents (27.4 per cent) answered all questions correctly, comprising one nurse, 10 pharmacists, one medical student and 17 doctors.
Pharmacists were identified as the professionals who had the greatest knowledge in this area achieving the highest proportion of correct answers. Pharmacists scored 98.5 per cent correct, doctors 92.4 per cent, medical students 84.3 per cent and nurses 76 per cent.
Staff survey
The electronic survey was completed by 235 members of the clinical staff (132 doctors, 71 registered nurses, 32 pharmacy team) though not all respondents answered all the questions. Of those questions in the staff survey that addressed possible knowledge deficits (see Table 3) just under 90 per cent of respondents considered that misinformation or lack of knowledge on which antibiotics contain penicillin medicines was an issue for some or most colleagues.
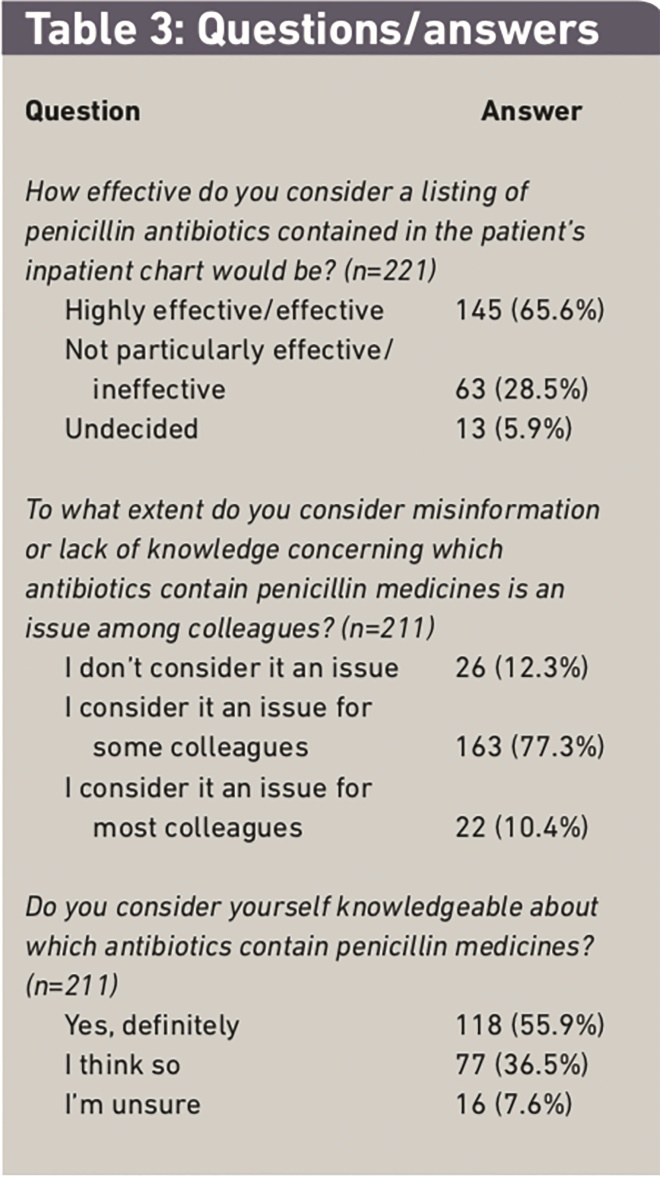
Table 3: Questions/answers
Five possible factors were presented as accounting for allergic patients being prescribed and administered penicillin antibiotics:
- Lack of knowledge/awareness of antibiotics containing penicillins
- Inadequacy of existing safeguard mechanisms
- Constraints on staff time
- Distractions and interruptions
- Poor adherence to policies and procedures
From these, 62 of 201 respondents (30.8 per cent) identified the first option as the single main factor accounting for these medication errors, while just over half of responding staff considered themselves definitely knowledgeable about which antibiotics contain penicillin. Two-thirds of respondents agreed that a listing in the drug chart of penicillin antibiotics would be effective in preventing future prescribing or administration errors.
Discussion
The quiz element of our study confirms that some qualified doctors, nurses and final-year medical students do not recognise antibiotics contraindicated in patients with penicillin allergy. Some of our findings are comparable to other results although different studies may have quizzed staff on a different range of antibiotics. We found that 80 per cent of doctors (32/40) gave the correct answer on the safety of seven listed penicillins. Cavell et al reported that 58 per cent of doctors (93/160) correctly recognised that a choice of six penicillins should be avoided.[17]
Their quiz was repeated after an intervention designed to ensure essential information was available to staff at all times. It was then found that 76 per cent of doctors (214/281) correctly recognised that all of seven penicillins should be avoided. However, statistically significant improvement in doctors’ knowledge was noted for only two of the original six antibiotic choices (with a seventh choice added in for the repeat quiz).
Our study found that 95 per cent of nurses (37/39) gave at least one incorrect answer about contraindicated antibiotics, compared with the 68 per cent of nurses (66/97) reported by others,[11]
although immediate access to a “traffic light” poster improved their results, with only five nurses considering at least one contraindicated antibiotic to be safe. Elsewhere, use of a bright red allergy sticker on drug charts as the intervention appeared to have little effect in improving nurses’ opinion of whether co-amoxiclav, Augmentin and meropenem were safe in penicillin allergy.[14]
We noted that meropenem, levofloxacin and ceftriaxone scored the highest incorrect responses overall (52.1 per cent, 45.7 per cent and 39.4 per cent, respectively) from a total of 94 nurses, doctors and medical students. Two of these antibiotics were also problematic in another study with incorrect combined responses from nurses and doctors of 80 per cent for meropenem and 50 per cent for ceftriaxone (levofloxacin was not listed in this quiz).13 Others have also reported poor awareness among health professionals of the potential for cross-reactivity with carbapenems (40 per cent) and cephalosporins (69 per cent).[12]
For penicillin-allergic patients there is a small risk of cross-sensitivity to cephalosporins and carbapenems so clinicians have to judge carefully when deciding to give or withhold these antibiotics for patients who report they are penicillin-allergic.
This knowledge deficit linked to penicillin antibiotics appears to be recognised among the staff who participated in the electronic survey, with around 90 per cent thinking that misinformation or lack of knowledge concerning which antibiotics contain penicillin is an issue for some or most colleagues. However, only 31 per cent identified lack of knowledge as the main causative factor for medication errors from five possible contributory factors. This would suggest that knowledge improvement on its own will not be sufficient to prevent these errors.
In our survey we found that two-thirds of respondents agreed that a listing of penicillin antibiotics contained in the patient’s inpatient chart would be of value. Where a bright red allergy sticker had been applied most staff (45 per cent to just under 80 per cent, depending on the professional group) thought that it had decreased the risk of allergic patients receiving penicillin or a related drug.[14]
We recognise the limitations of this study. The quiz was undertaken by a relatively small sample of health professionals (106 health care staff out of a total clinical workforce of about 1,800 whole time equivalents), while other studies have ranged from testing fewer than 100 staff[10]
to just over 600.[12]
The artificial setting of the quiz required firm answers without recourse to a reference source, when normally one would expect health professionals who are uncertain about the safety of a specific medicine to seek advice and help rather than make a best guess. The electronic survey results are subject to some of the usual limitations associated with surveys of this nature: we obtained responses from only a small proportion of the total clinical staff workforce, and those who did respond may not be representative of the wider workforce. In addition, predetermined responses may force respondents into selecting an answer that is not entirely accurate.
However the quiz results and answers from the survey show that increased awareness and training are needed at ward level, with particular emphasis on meropenem, cephalosporins, combination products and levofloxacin. Pharmacists’ results for the knowledge quiz show their drug expertise, and confirm the importance of pharmacy involvement in helping to achieve patient medication safety at ward level. Hence an educational awareness programme, including teaching sessions for junior doctors, the redistribution of traffic light posters and the introduction of a revised drug chart containing a list of penicillin medicines, are all planned or are under way, together with a repeat knowledge test. We are aware that the medical team has recently introduced punitive measures for doctors who continue to make penicillin prescribing errors. This was to complement the traditional appraisal system that nurses undergo when they make an administration error because it was believed that although nurses were being disciplined, prescribers who made errors were escaping any sort of follow up, support and possible censure. We are also considering instigating separate storage for penicillin antibiotics on wards although there appears to be limited evidence that this acts as a physical barrier to prevent administration errors.[18]
Using resources[19]
to enable patients to understand better the difference between a penicillin allergy and a side effect is also being considered since this is recognised as a contributory factor to medication errors.[20]
Declaration of interest
Pfizer, through an educational grant, helped facilitate some aspects of the qualitative work described in this paper.
About the authors
Lorraine Moore, MRPharmS, Ian Nicholls, Neil Powell, MRPharmS, and Michael Wilcock, MRPharmS, are all pharmacists at the Royal Cornwall Hospitals NHS Trust, Truro, Cornwall TR1 3LJ.
Correspondence to: Michael Wilcock (email mike.wilcock@rcht.cornwall.nhs.uk)
References
[1] Safety in doses: medication safety incidents in the NHS. Fourth Report from the Patient Safety Observatory. London: National Patient Safety Agency, 2007.
[2] Cranshaw J, Gupta KJ, Cook TM. Litigation related to drug errors in anaesthesia: an analysis of claims against the NHS in England 1995–2007. Anaesthesia 2009;64:1317–23.
[3] Mother’s drug allergy not checked. BBC News Online. 22 March 2006. Available at: http://news.bbc.co.uk/1/hi/england/bradfor d/4833922.stm (accessed 13 December 2011).
[4] Standardising wristbands improves patient safety. London: National Patient Safety Agency, 2007.
[5] Gay KJ, Hill C, Bell T. Accuracy of drug allergy recording in a district general hospital. International Journal of Pharmacy Practice 2009;17:253–5.
[6] Kalliat R, Smith N, Graham-Clarke E,et al. An audit of the completeness and accuracy of allergy status documentation. Clinical Pharmacist 2010;2:369.
[7] Ismail ZF, Ismail TF, Wilson AJ. Improving safety for patients with allergies: an intervention for improving allergy documentation.Clinical Governance: An International Journal 2008;13:86–94.
[8] Kathawala M. Improving drug allergy documentation using a pharmacist-led campaign.British Journal of Clinical Pharmacy 2010;2:244–6.
[9] Department of Health. Building a safer NHS for patients — improving medication safety. London: Department of Health, 2004.
[10] Cavell G. Prescribing skills of F1 and F2 junior medical staff. Pharmacy World and Science 2008;30:633–4.
[11] Bergin C, Cavell G. Promoting safe administration of penicillins and penicillin-containing antibiotics. Pharmacy World and Science 2008;30:972–3.
[12] Llanwarne N. Mendes F, Martin J. Safe prescribing in penicillin allergy: a knowledge-improvement scheme. Available at: http://blogs.bmj.com/agentsforchange/ 2010/06/08/safe-prescribing-in-penicillin- allergy-a-knowledge-improvement-scheme/ (accessed 17 May 2011).
[13] Hughes J, Kaur A, Marriott J. Investigation of allergy status at City Hospital, Birmingham. Clinical Pharmacist 2010;2(Suppl 1):S28.
[14] Oborne CA, Tapya L, Iglesias A, Torrens N. Knowledge of beta-lactams and the impact of penicillin allergy stickers on risk. Pharmacy World and Science 2008;30:1069–70.
[15] Cavell C, Scutt G, Welch J, King C. Teaching doctors to prescribe penicillin safely. Pharmacy World and Science 2008;30:306–7.
[16] Richie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman and Burgess (editors). Analysing qualitative data. London: Routledge, 1994; pp173–94.
[17] Cavell G, Jaffer S. FACT: knowledge of antibiotics contraindicated in penicillin allergic patients can be improved. Clinical Pharmacist 2011;3(Suppl 2):S22.
[18] Oborne CA, Taher F, Torren N et al. Separate storage of beta lactams: impact on practice and knowledge. Clinical Pharmacist 2009;1(Suppl 1):S13.
[19] South West Medicines Safety Partnership. NHS South West and the Association of the British Pharmaceutical Industry Medicines Safety Partnership. Medicine Allergy Matters. Available at: www.swmit.nhs.uk/ SWMSP_AllergySummary.htm (accessed 17 May 2011).
[20] MacPherson RD, Willcox C, Chow C, Wang A. Anaesthetist’s responses to patients’ self-reported drug allergies. British Journal of Anaesthesia 2006;97:634–9.


