Abstract
Aim
To explore community pharmacists’ perceptions of motivations and barriers influencing their engagement in continuing professional development (CPD) over time.
Design
A prospective longitudinal study comparing the perceptions of trained and non-trained community pharmacists at two points in time.
Subjects and setting
Community pharmacists working in three primary care trusts: Barking & Dagenham, Havering, and Tower Hamlets PCTs.
Outcome measures
Pharmacists’ perceptions.
Results
Five themes of motivations for, and six themes of barriers to engaging in CPD emerged from the interviews at two points in time. Few differences were found between trained and non-trained groups. The three main barriers included a lack of information, a lack of motivation and a lack of time; supply of more information, becoming self-motivated, and integration of CPD into work were suggested as remedies. Over time, the proportion of pharmacists engaging in CPD increased in the trained group.
Conclusions
No change occurred in the motivations for engaging in CPD over time. The pharmacists perceived that they would engage in CPD to attain and maintain competence. However, by the end of the study, a greater proportion of trained pharmacists had begun engaging in CPD whereas non-trained pharmacists participated only in continuing education. These findings suggest that pharmacists may need support to engage fully in CPD.
The Department of Health has emphasised the link between lifelong learning and the quality of healthcare provided by the NHS, encouraging healthcare professionals to identify and meet their learning needs to maintain their competence.1 Continuing professional development (CPD) has been recommended as one way to ensure the competence of healthcare professionals, including pharmacists.1–6 The Royal Pharmaceutical Society of Great Britain7,8 has defined the aim of CPD as “to provide a means for the profession to reassure the public that pharmacists maintain and enhance their capabilities throughout their working lives”, which emphasises the link between CPD and patient safety. Past research has shown that pharmacists may also perceive other factors, such as “the opportunity to break the routine” provided by learning, “having the opportunity to interact and exchange ideas with others” and “requirements for maintenance of professional licensure” to influence their participation in learning activities.9,10
Since 2005, when registering to practise pharmacists have had to commit to undertake and record CPD unless they declare themselves as non-practising8,11 and, in 2007, the Pharmacists and Pharmacy Technicians Order was approved by the Parliament, bringing the implementation of mandatory CPD nearer.12 However, pharmacists have reported different reasons for not participating in learning activities, for example, a lack of time and resources.10,13–17 “Plan and record continuing professional development” offers little support in identifying and prioritising learning needs as it encourages pharmacists to reflect on their current competence to form learning objectives.7 There is also little support for accessing learning opportunities, which may become a barrier for community pharmacists, who often work alone. Few studies have explored whether community pharmacists’ motivations and perceptions about barriers to engaging in CPD change over time. The aim of this study was to explore community pharmacists’ perceptions of factors influencing engagement in CPD during 2002 and 2004. At that time pharmacists were required to participate in continuing education (CE) or learning activities which are part of a CPD cycle comprising identifying learning needs, planning learning activities, learning (activities), and evaluating learning outcomes, and changes to professional development requirements were anticipated.18,19 The perceptions of a group of pharmacists trained to provide medication reviews were compared with perceptions of a non-trained group.
Methods
The study explored perceived motivations and barriers to engaging in CPD of trained and non-trained community pharmacists using in-depth individual interviews during a training programme in 2002 and in 2004, following provision of medication reviews in 2003 and 2004.
The study was based within the North East sector of the London Strategic Health Authority. A medication review service development project in community pharmacy was conducted within Barking and Dagenham, and Havering Primary Care Trusts.20 This study was conducted in these two PCTs and in the nearby Tower Hamlets PCT where the service was not developing. Ethics approval (code: LREC 2001 [B&H] 167) was obtained for the medication review study. Although it was not required for the current study, the study protocol was reviewed by independent researchers at the School of Pharmacy, University of London.
Sample
Trained pharmacists
In 2001, Barking and Dagenham, and Havering PCTs invited all 80 community pharmacists working within the PCTs to provide medication reviews and 43 were recruited (the trained group). Thirty-seven pharmacists completed clinical pharmacy training and were accredited as reviewers in 2002; two withdrew for personal reasons.21 The training, provided by the Robert Gordon University, Aberdeen, comprised a 30-credit clinical pharmacy distant learning course at postgraduate certificate level, comprising four compulsory modules (pharmaceutical care planning, cardiovascular therapeutics I and II, and endocrine therapeutics) and one optional module (respiratory, musculoskeletal or gastrointestinal therapeutics), a two-day workshop on patient interviews and care planning and a one-day workshop on IT-training. Twenty-six pharmacists provided medication reviews in 2003 and 2004; workload and other reasons prevented nine from further participation.
Non-trained pharmacists
Community pharmacists working within Tower Hamlets PCT were recruited to the non-trained group; they had not been offered the possibility to participate in the medication review project and did not participate in the training. Contact details of 35 pharmacies were identified through the NHS website for local pharmacy services and 29 pharmacists agreed to participate.
Developing interview guides
Phase 1
A postal questionnaire was developed to capture the pharmacists’ demographics and to explore their professional perceptions parallel to the interviews. To explore pharmacists’ perceptions of CPD in-depth, an interview guide with six topics was developed and reviewed for its face validity for interviews with the trained group.22 Content validity was ensured by allowing the guide to respond to the interviewees’ responses23 and three topics were added during the first few interviews. The refined guide was also used for interviews with the non-trained group.
Phase 2
An interview guide was developed to explore any changes in perceptions. Three topics remained the same, five were modified and one was omitted. The face validity of this guide was again reviewed and it was used in the interviews with both groups.
Interviews
Appointments were arranged with both the trained group and the non-trained group who had responded to the survey. In 2002, face-to-face interviews were conducted with trained pharmacists and telephone interviews with non-trained pharmacists while, in 2004, telephone interviews were conducted with both groups because these were found to provide as rich data as the face-to-face interviews. All interviewees consented for audio-taping of the interviews that were then transcribed verbatim.
Data handling and analytical procedures
All interview data were stored safely and anonymised. The data were entered onto a database using NVivo 1.3 software for data storage, coding of the interviews and data retrieval. Iterative processes of analysis were employed at phases 1 and 2. A grounded approach was employed and the codes and themes emerged from the transcripts.23 The perceptions of the trained group were compared with those of the non-trained group and between the phases to assess any changes in perceptions.
Results
Sample
In 2002, all 43 pharmacists participating in the training were interviewed. In the non-trained group, 14 of 18 survey respondents were interviewed. Two pharmacists were too busy and refused; another two could not be traced for an interview.
In 2004, 33 of 35 trained pharmacists were interviewed; one was too busy and another had retired. Five of seven non-trained survey respondents were interviewed; two were too busy.
The characteristics of the pharmacists are shown in Table 1. In 2002, six, and in 2004, four interviewed trained pharmacists did not complete the survey. Therefore, data on most characteristics were available for 51 interviewees in 2002, and 34 interviewees in 2004.
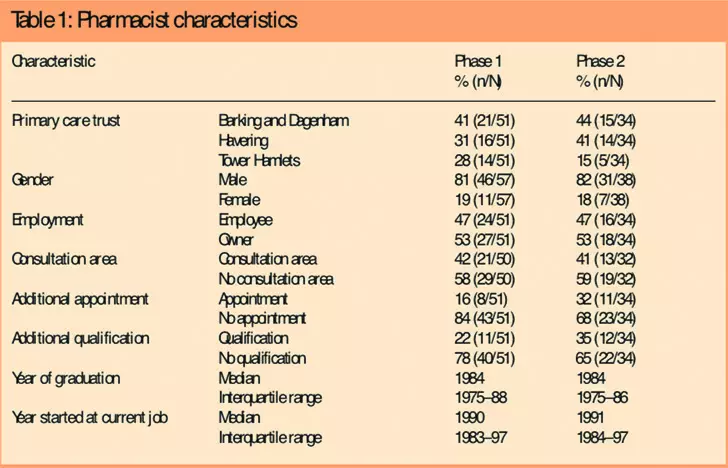
In 2004, sample attrition may have influenced the perceptions of the non-trained group. Female pharmacists or any with a consultation area in their pharmacy were not interviewed.
Phase 1: Motivations and barriers to engaging in CPD
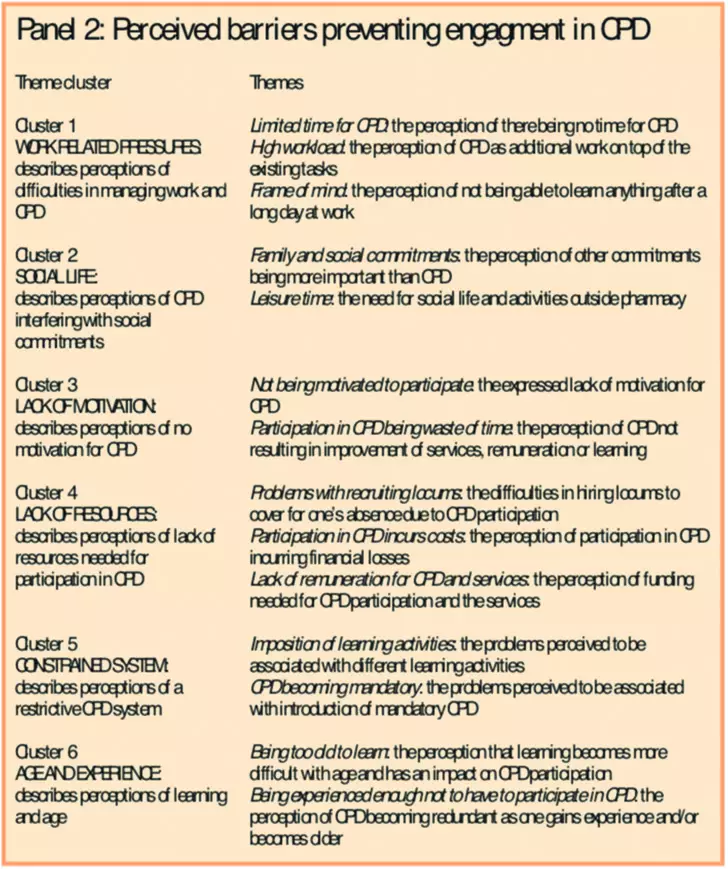
In 2002, many community pharmacists felt motivated to develop themselves, but barriers may have prevented them from engaging in CPD (Panels 1 and 2). There were few differences between trained and non-trained groups.
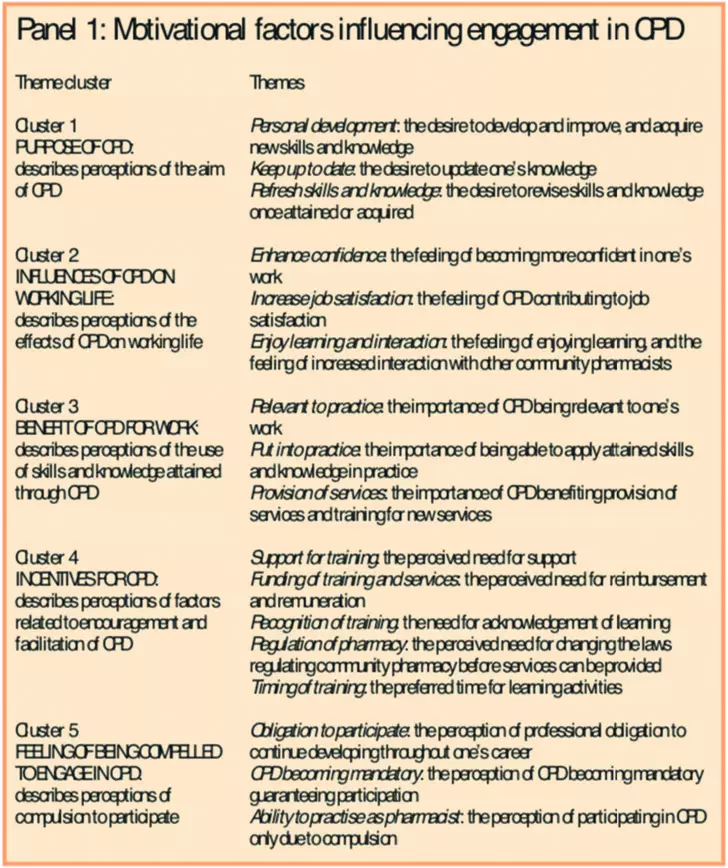
Personal development, keeping up to date and refreshing skills and knowledge (motivational cluster 1) were important motivators for community pharmacists to participate in learning activities. The desire to learn motivated pharmacists to engage in professional development, thus reflecting its purpose:
Motivates? Well, […] I want to do it better for myself […] and for people. If I’m going to serve them and that would help them, wouldn’t it, if I improve myself I improve my services.
1001B, male, trained, section 3
Some trained older pharmacists admitted not having participated in CE. While they had concentrated in ensuring a profitable business, their knowledge had deteriorated. The introduction of CPD presented an opportunity for the pharmacists to acquire new skills and knowledge.
Pharmacists were motivated by their desire to enhance confidence, increase job satisfaction, enjoy learning and interaction (motivational cluster 2) and wanted to be able to use the acquired skills and knowledge in practice (motivational cluster 3), especially to provide expected new services, introduced in 200524:
I think when you talk to the patient [CPD] gives you more confidence. And so, it’s probably part of the job satisfaction what you are doing.
1040B, male, trained, section 3
If there is to be new services then I would, of course, need more training. If we start measuring blood pressure, blood glucose levels or cholesterol I would need to do training.
1081B, male, non-trained, section 3
However, the realisation that CE activities did not always have an application in community pharmacy had led some trained pharmacists not to participate in further activities; their efforts had been futile.
Although many understood the benefits of CPD, most perceived difficulties in managing both work and CPD which created stress (barrier cluster 1). Many did not wish to study or were not able to concentrate after work. During the day paid work was prioritised:
We have our patients and we have to keep the GPs and nurses happy and we have to keep up with our deliveries that all has to [be] taken into consideration before we can talk about doing CPD.
1096B, male, non-trained, section 6
Pharmacists resented CPD for interfering with other commitments (barrier cluster 2). Female pharmacists reported that family came first:
Family life. […] After I finish work, [I] go home and start another shift, […], that is one obstacle.
1032B, female, trained, section 4
Some form of compulsion and recognition of pharmacists’ contribution to healthcare was regarded as important as an incentive for engaging in CPD (motivational cluster 4). As CPD would help pharmacists to provide new services, they wanted to be remunerated for service provision. Others thought that a lack of motivation (barrier cluster 3) and a lack of resources (barrier cluster 4) would be barriers to their participation:
There are more obstacles than there […] is provision of encouragement for us to take part in CPD.
1096B, male, non-trained, section 1
The proposed CPD system was thought to be restrictive (barrier cluster 5). Pharmacists thought that they should not be required to employ all different learning activities but be allowed to continue with the one they felt comfortable with and which facilitated their studies. Some disapproved of the introduction of mandatory CPD, six trained male pharmacists considered quitting, and others felt intimidated.
Some older pharmacists perceived that they were experienced enough not to participate in CPD, whereas younger pharmacists thought they were still developing their competence. Perhaps due to the training experience, some older trained pharmacists perceived that studying became more difficult with age (barrier cluster 6):
Mind isn’t as absorbent as it used to be. I have to read something three or four times to grasp it and I am hoping it’ll stick but I am not too sure about that either. Because three weeks later I may need to read it again.
1003B, male, trained, section 22
Phase 2: Overcoming barriers to engaging in CPD
The interviewees were categorised into three groups according to their level of engagement in learning:
- Participants in CPD — able to identify their own learning objectives, which they tried to fulfil through participation in identified learning activities
- Participants in CE — participated in learning activities but did not identify learning objectives
- Non-participants — had no motivation or time to participate in learning activities
By 2004, pharmacists seemed more positive about mandatory CPD participation, compared to being threatened by it in 2002.
A greater proportion of trained pharmacists had begun engaging in CPD; they were able to identify their own learning needs which they tried to fulfil:
I think that based on my knowledge I realise that I am lacking certain areas. I know it is going to be good […]The most important thing is to make sure I know what I am doing.
1008F, male, trained group, section 7
Attrition may have influenced the non-trained group, but none had become more accountable for his or her own learning: they did not engage in CPD.
Although no new motivations or barriers emerged in 2004, pharmacists suggested remedies to minimise the influence of the three main barriers — a lack of information on CPD, a lack of motivation and a lack of time to engage in CPD — and how to overcome these (Figure 1).
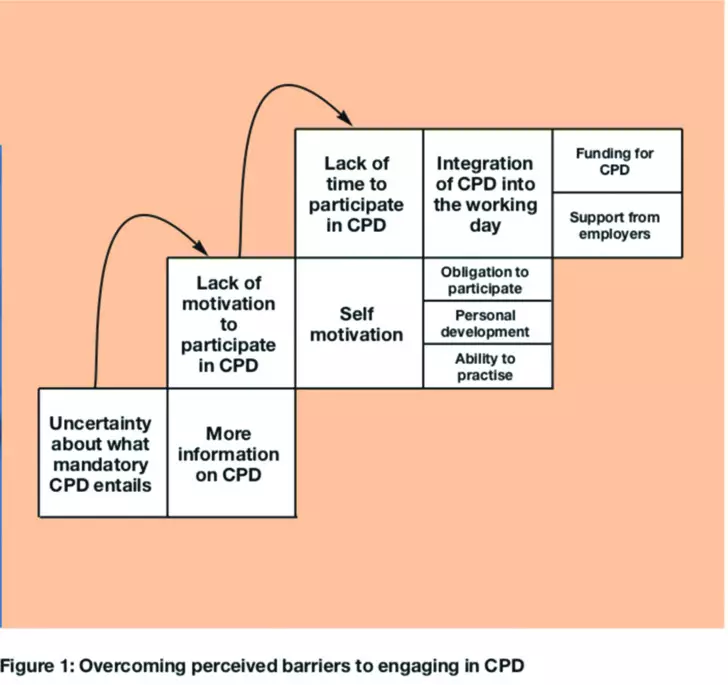
The first barrier to overcome was a lack of information about CPD. More information was suggested to ensure full engagement of pharmacists in CPD:
I think there is a lot of confusion at the minute as to what CPD actually means and exactly what it involves. […] I think it hasn’t been made clear as to what it is that you need to do and how to do it […] there needs to be a little bit more explanation.
1021F, male, trained, section 2
The second barrier was a lack of motivation. Becoming self-motivated to learn and develop and realising the benefits of engaging in CPD were perceived to help those who lacked motivation to study. Few in the trained group perceived that everyone should be motivated enough to engage in CPD, although others thought that engaging in CPD was an obligation:
I think as it’s very relevant to the practice and [if] you find certain areas difficult for you to practise, then the only way […] to improve […] them is by trying to take on a course or asking them how you can improve on that. The motivation […] would be a better service to what one is doing.
1011F, male, trained, section 2
Well informed and motivated pharmacists faced yet another hurdle: lack of time. Thus, integration of continuing professional development into the working day through support from employers and offering funding for CPD was perceived to support their engagement in CPD:
It would be nice, how these barriers could be lifted, would be if the employer […] gave me time to do these things in workplace. Rather than expecting for me to do it in my own time.
1013F, male, trained, section 2
Discussion
The five themes of motivations for, and six themes of barriers to, engaging in CPD were stable over time. Supply of more information, becoming self-motivated, and integration of CPD into work were suggested to overcome the three main barriers.
Strengths and limitations
Although the recruitment of community pharmacists was geographically restricted and allocation to groups was not random and the findings may not be generalisable, the findings provide an insight into community pharmacists’ perceptions on complex issues.23
Attrition of respondents is to be expected in a longitudinal study23; the findings represent the perceptions of those who were interviewed twice. No non-trained female pharmacists were interviewed in 2004 which may influence the findings. The pharmacists were contacted a minimum of three times in an attempt to persuade them to interview but various practical factors mean that some are bound to drop out of such a study.
Ideally, the phase 1 interviews should have been conducted before the recruitment to the service development project to decrease the potential for bias in perceptions of professional development. However, the PCTs had recruited the trained pharmacists and the interviews were conducted as soon as practically possible. The non-trained group was recruited from another PCT and there were few differences between the groups’ perceptions, implying this bias was minimised.
Overcoming barriers to engaging in continuing professional development
At the time, engaging in CPD was soon expected to become mandatory. Similarly to other studies, personal development, keeping up-to-date, refreshing skills and knowledge and desire to learn were important motivations for community pharmacists to participate in learning activities.9,10,17,25,26 However, in the US, complying with a professional obligation was a more important motivator for pharmacists who had to participate in mandatory CE than personal development itself.9,10 After a shift from voluntary to mandatory participation in CPD the influence of “competency-related curiosity” was reported to have decreased while “compliance with external influence” increased,26 suggesting that similar changes in motivations that can influence learning outcomes may also occur in the UK.
Hanson and DeMuth suggested that the greater the internal motivation to learn, the greater number of learning activities pharmacists participated in.27 Possessing a postgraduate degree or working full-time had also been reported to influence participation.27,28 However, mandatory participation in CE had not increased participation in a greater number of learning activities.27 In this study, some pharmacists had not participated in CE in the past. Engaging such pharmacists is essential for successful implementation of mandatory CPD to ensure pharmacists’ continued competence.
Time constraints and other commitments were perceived as barriers to engaging in CPD. Indeed, pharmacists working full time, those who are newly qualified or are in their 30s or 40s may feel further constraints on their CPD engagement.10,14 In this study, female pharmacists felt torn between their family and work commitments.
As reported in other studies, some perceived that a “lack of remuneration” prevented them from participating in learning activities.13,14,16 The proposed CPD system was regarded as restrictive, suggesting that the expected changes in professional requirements may even have led others to withdraw their registration.29
In this study, older pharmacists felt experienced enough not to participate in CPD, whereas younger pharmacists thought they were still developing their competence. In contrast, “being out of date” has previously been reported as a reason for not participating in learning activities and newly qualified pharmacists have perceived that they were at the peak of their pharmaceutical knowledge and did not need to participate in CE, but instead needed to develop their communication skills through experience.14,15 This not only indicates potential skill and knowledge gaps and differences in motivations to learn between generations but also shows that in the past CE may have been perceived to be useful for attaining pharmaceutical knowledge only.
By 2004, pharmacists seemed more positive about mandatory CPD participation. The intervention and CPD policies may have influenced this change in opinion. While more trained pharmacists seemed to be engaging in CPD, they had completed a predesigned course and were only allowed to choose one training module; independent planning of learning was not promoted.
The conceptual shift from CE to CPD may have caused uncertainty around what mandatory CPD would entail, also reported by Swainson and Silcock17 and Attewell et al.25 A “lack of information about CPD” was perceived to be a barrier to engaging in CPD, supported by Bell et al,16 highlighting one of the main barriers to implementing mandatory engagement in CPD.
Feeling disillusioned with community pharmacy was common and also observed by Ward et al.14 Hanson and DeMuth,10 Mottram et al15 and Attewell et al17 suggested that pharmacists may have perceived that a “lack of relevant learning opportunities” prevented their engagement. Despite being motivated, as reported by others, a lack of time seemed to be a perpetual barrier to engaging in CPD.10,13,15–17
Conclusions
No change occurred in the motivations for engaging in CPD over time. In general, as supported by literature, the community pharmacists perceived that they would engage in CPD to attain and maintain competence.9,10,17,25,26
However, by the end of the study, a greater proportion of trained pharmacists had begun engaging in CPD whereas non-trained pharmacists participated in CE. These differences illustrate that engagement in CPD may be prevented by an uncertainty of what it entails, a lack of motivation to engage in learning as well as a lack of time, also observed in other studies.10,13–17,25
Pharmacists suggested that more information on CPD is required, that they should become self-motivated, and that they may need more support and facilitation than is currently available to embark fully on engaging in CPD.
Acknowledgements
The Barking and Dagenham, and Havering Primary Care Trusts funded this service development project. Raisa Laaksonen was supported by the Osk Huttunen Fund, Finland. We thank the PCTs for recruiting the community pharmacists, the Robert Gordon University for providing the training, and the pharmacists for participating.
About the authors
Raisa Laaksonen, PhD, MRPharmS, was, at the time of the study, research pharmacist in the department of practice and policy at the School of Pharmacy, University of London. She is now lecturer in pharmacy practice at the University of Bath.
Catherine Duggan, PhD, MRPharmS, was director of academic department of pharmacy at Barts and The London NHS Trust. She is now associate director of clinical pharmacy at the School of Pharmacy, University of London.
Ian Bates, MSc, MRPharmS, is professor and head of educational development at the School of Pharmacy, University of London.
Correspondence to: Dr Raisa Laaksonen, Department of Pharmacy and Pharmacology, University of Bath, Bath BA2 7AY (tel 01225 383829, e-mail r.laaksonen@bath.ac.uk).
References
- Department of Health. A first class service: quality in the new NHS. London: HM StationeryOffice; 1998.
- Department of Health. Continuing professional development: Quality in the new NHS. London: HM Stationery Office; 1999.
- Department of Health. Pharmacy in the future — implementing the NHS plan. A programme forpharmacy in the National Health Service. London: HM Stationery Office; 2000.
- Department of Health. Learning from Bristol: the report of the public inquiry into children’s heartsurgery at the Bristol Royal Infirmary 1984–1995. London: HM Stationery Office; 2001.
- Department of Health. Working together — learning together. A framework for lifelong learningfor the NHS. London: Department of Health Publications; 2001.
- Department of Health. Clinical governance in community pharmacy. Guidelines on good practicefor the NHS. London: Department of Health Publications; 2001.
- Royal Pharmaceutical Society. Plan & record continuing professional development version 1.1. Available at: www.uptodate.org.uk/home/PlanRecord.htm (accessed 15 June 2004).
- Royal Pharmaceutical Society. Medicines, ethics and practice 2005. London: The Society; 2005.
- Mergener M A, Weinswig MH. Motivations of pharmacists for participating in continuingeducation. American Journal of Pharmacy Education 1979;43:195–9.
- Hanson A L, DeMuth JE. Facilitators and barriers to pharmacists’ participation in lifelong learning. American Journal of Pharmacy Education 1991;55:20–29.
- Bellingham C. To practise or not: that is the question. Pharmaceutical Journal2004;273:809–10.
- Royal Pharmaceutical Society. Section 60 Order heralds new era for pharmacy (news release 9February 2007). Available at: www.rpsgb.org.uk/pdfs/pr070209.pdf (accessed 4 June 2007).
- Mottram DR, Rowe PH. Evaluation of the impact of recent changes in postgraduate continuing education for community pharmacists in England. International Journal of Pharmacy Practice1996;4:123–8.
- Ward PR, Seston EM, Wilson P, Bagley L. Perceived barriers to participating in continuing education: the views of newly registered community pharmacists. International Journal of Pharmacy Practice 2000;8:217–24.
- Mottram DR, Rowe P, Gangani N, Al-Khamis Y. Pharmacists’ engagement in continuingeducation and attitudes towards continuing professional development. Pharmaceutical Journal 2002;269:618–22.
- Bell H, Maguire T, McGartland LF. Perceptions of continuing professional development within the pharmacy profession. Journbal of Social and Administrative Pharmacy 2002;19:87–98.
- Attewell J, Blenkinsopp A, Black, P. Community pharmacists and continuing professional development — a qualitative study of perceptions and current involvement. Pharmaceutical Journal 2005;274:519–24.
- Society moves nearer to mandatory continuing professional development. Pharmaceutical Journal 2001;267:527–32.
- Royal Pharmaceutical Society. Medicines, ethics and practice 2002. London: The Society; 2002.
- Mackie C A, Mohammed A, Corlett S, Laaksonen R, Bates I, Duggan C et al. A randomised controlled trial of medication review by accredited community pharmacists. International Journal of Pharmacy Practice 2005;13(Suppl):R17.
- Laaksonen R, Duggan C, Bates I, Mackie C. Performance in clinical therapeutics training of community pharmacists. Pharmacy Education 2007;7:167–75.
- Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook (2nd ed). Thousand Oaks: Sage Publications; 1994.
- Smith F. Research methods in pharmacy practice. London: Pharmaceutical Press; 2002.
- Department of Health. Implementing the new community pharmacy contractual framework. Information for primary care trusts. London: Department of Health Publications; 2005.
- Swainson D, Silcock J. Continuing professional development for employee pharmacists: a survey to compare practice in the hospital and community sectors. Pharmaceutical Journal 2004;272:290–3.
- Mergener MA. The effect of mandatory continuing education on pharmacists’ motivations for participating in continuing education. American Journal of Pharmacy Education 1981;45:273–7.
- Hanson AL, DeMuth JE. A study of pharmacists’ behavior as lifelong learners. American Journal of Pharmacy Education 1992;56:335–43.
- Laaksonen R, Mills ER, Duggan C, Davies JG, Bates I, Mackie C. The effect of training and service provision on the self-assessed competence of community pharmacists. International Journal of Pharmacy Practice 2007;15:141–7.
- Hassell K, Seston L. Workforce update — joiners, leavers, and practising and non-practising pharmacists on the 2006 Register. Pharmaceutical Journal 2006;277:576–8.