Abstract
Aim
To determine the proportion of patients attending an accident and emergency (A&E) department who are suitable for management by a pharmacist.
Design
A cross-sectional, retrospective review of patient notes, testing criteria defined from the literature.
Subjects and setting
Adult patients attending an inner London teaching hospital A&E department during a two-week period between March and April 2006.
Outcome measures
The proportion of adult patients attending A&E who can be assessed and treated by a pharmacist.
Results
4,503 patient notes were reviewed. Of these 218 patients (5%) were identified as suitable to be seen by pharmacists based on information documented in the initial nursing assessment. Final assessment of the full case notes identified 87 patients (2%) as suitable for management by a pharmacist. The most common patient group identified by initial assessment was sore throat (44/218, 20%). However final assessment showed requests for medicines were the largest patient group (24/87, 28%). A specificity test result of 97% shows high levels of agreement between patients considered not appropriate for management by a pharmacist and those not identified by the tool. However the positive predictive value of 40% indicates that screening based on initial assessment was less effective at picking up suitable patients.
Conclusion
A pharmacist could treat at least 2% of adults presenting at the study hospital A&E department. This excludes 3% of patients with minor ailments currently well managed by nurses in the study hospital. A pharmacist working in this A&E department could treat an estimated 5,854 patients annually. Incorporating a pharmacist within the team may alleviate the workload of emergency staff and could potentially reduce waiting times.
The Department of Health implemented the four-hour target on UK accident and emergency (A&E) departments in October 2001. This policy states that each A&E department should see and treat all patients within a four-hour period.1 The DoH encourages use of pharmacists in the A&E department as they support skill mix.2 Using pharmacists in A&E could result in a reduction in A&E waiting times and costs, as patients can be directly referred to a pharmacist, rather than wait to see an A&E doctor at increased cost.3
An urgent care centre (UCC) was recently established in an inner London teaching hospital and is based within the A&E department. It acts as a non-appointment primary care medical service. The UCC was established because increasing numbers of patients were presenting with minor injuries, minor illnesses and “self-care” complaints. These patients represent approximately 40 per cent of all A&E attendances in the study hospital. The UCC staff is multiprofessional and includes emergency nurse practitioners, GPs and pharmacists. Patients coming to the UCC are encouraged to attend primary care services for similar problems in the future. The UCC is open from 8am until 11pm.
There is also an adult minor injuries unit (MIU) within the study hospital but this is located at another site. It runs as a non-appointment unit and is open from 7.30am to 9.30pm. It is solely led by nurses rather than a multiprofessional health care team. Occasionally patients attending the adult MIU are referred to the UCC.
From January 2004, a pharmacist was made available to the A&E department, via bleep. Patients booking into the A&E requesting medicines are already seen by a pharmacist4 who, where appropriate, also attempts to link them back to a GP. These patients were previously identified as a group pharmacists could quickly and easily manage.5 This new service reduced patients’ waiting time, optimised skill use, facilitated workflow and has the potential to reduce waiting times across the A&E department.
The NHS plan6 considers patient convenience a key feature of patient care and this was reinforced by the recent paper, “Building on the best; choice, responsiveness and equity in the NHS”.7 Pharmacy-led minor ailment services and schemes are based on this concept.8,9 Minor ailment services are recognised as an essential role for community pharmacists in Scotland and are incorporated within their new community pharmacy contract. Development of local pharmaceutical services (in England) within the new pharmacy contract is a key feature of redesigning pharmacy services around patients’ needs.10 Incorporating minor ailments as an enhanced service within this new contract has been suggested for community pharmacists in England.11
Few studies have been conducted on the role of pharmacists in A&E. One study concluded that 8 per cent of patients attending an A&E department may be suitable to be managed by a pharmacist. This study identified patients according to primary care criteria and the investigator’s pharmacy experience.5 A second study has reported 25 per cent of patients attending an emergency department were seen by a pharmacist. It is unclear what this figure represents: all patients attending A&E or patients attending the MIU. This study also differs from our work as it did not define explicitly any criteria used to refer patients to the pharmacist.12 There are no studies using explicit criteria based on patients presenting symptoms to determine suitability for pharmacist management rather than an investigator’s experience.
In A&E, patients are assessed by a nurse (triage or streaming) before being referred to the appropriate area within the department.
This study investigates the need for a pharmacist within the A&E department by assessing patients presenting with minor ailments that a pharmacist can manage.
The aims of the study were: to define explicit, simple to use, generalisable criteria for referral of A&E patients to a pharmacist; to assess the feasibility of using the criteria as a screening tool; to estimate the proportion of patients attending the A&E department who are suitable to be managed by a pharmacist; and to investigate how many patients requesting medicines were referred to the pharmacist currently available to the department.
Method
Inclusion and exclusion criteria were developed to define patient suitability for pharmacist management (for an example, see Panel 1).
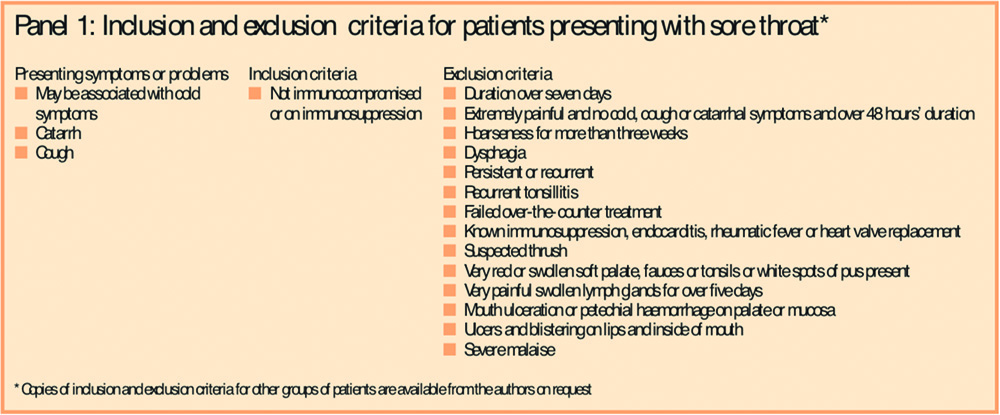
Criteria were based on minor ailments regularly managed by community pharmacists,13,14 the local primary care trust minor ailments scheme protocol15 and the list of conditions suitable for pharmacist management from the Royal Pharmaceutical Society.9 Criteria were reviewed by the A&E pharmacist and the lead UCC GP.
Patient groups considered suitable were: those requesting medicines (including emergency hormonal contraception) and those with hay fever, athlete’s foot, simple colds and nasal symptoms, simple constipation, simple cough, simple diarrhoea, dyspepsia, ear problems, mild eczema or dry skin, head lice, sore throat, vaginal thrush, allergic conjunctivitis, cold sores, threadworms, warts or veruccae. Exclusion parameters were largely based on symptoms indicating a more serious condition.
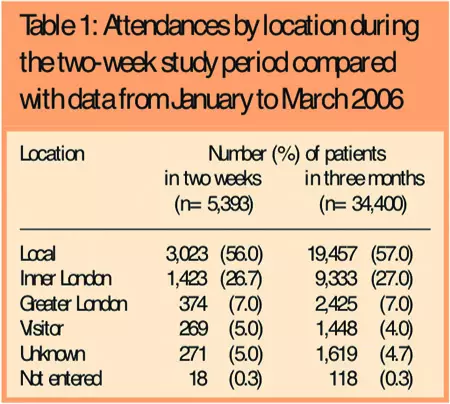
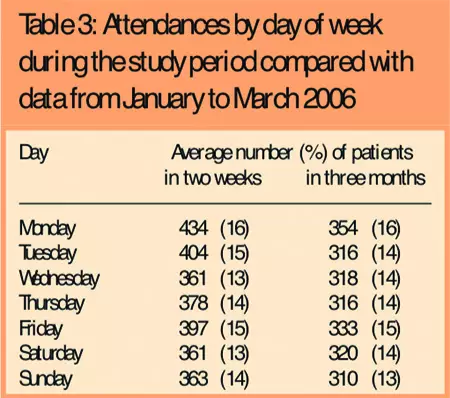
Data were collected at a large, inner London teaching hospital. Most patients (80 per cent) attending A&E in the study hospital are aged under 55 years. Attendances are lowest on Sundays (13 per cent) and highest on Mondays (16 per cent). Over half of patients live locally with 84 per cent living within the inner London boundaries.
The patient destination was the initial inclusion criterion because it was thought that patients referred to the UCC by the streaming nurse were most appropriate to be seen by the pharmacist. Patients directed to majors or resuscitation have more serious injuries or conditions and were therefore excluded. During the hours UCC was closed (11pm to 8am) patients’ presenting symptoms were considered and the streaming destination was discounted.
Data collection forms were designed and piloted to include the time of attendance, where the patient was seen, and whether symptoms for inclusion or exclusion according to the criteria were present. Other information recorded included: A&E number, whether the patient attended UCC, investigations or examinations that led to exclusion of that patient and whether or not they were seen by the pharmacist available to the A&E department.
After the pilot study three more patient groups were added: flu-like symptoms, upper respiratory tract infections and a multiple symptoms category.
Data were collected retrospectively for two weeks between March and April 2006. Patients under the age of 16 years and patients seen in areas other than the UCC or adult MIU during UCC open times were not screened.
Patient details recorded during initial nursing assessment were compared to the inclusion/exclusion criteria. If the initial presenting symptoms or patient group were within the inclusion criteria, the whole A&E notes were examined to assess whether the patient was suitable according to the full clinicians’ record. Thus, patients were suitable by initial and final assessment if the clinician examination showed symptoms and diagnosis fell within the inclusion parameters.
The A&E computer system was used to track missing patient records and to assess the records where patient notes were unavailable, as the hard copy of the notes could not be viewed. Hard copies of all adult MIU cases were unavailable as these patients’ notes were not at the study site.
Inclusion and exclusion criteria were applied to data recorded on the A&E computer database for unavailable notes.
Specificity testing was used to analyse the proportion of patients who were not suitable to be seen by a pharmacist and were correctly identified as such by the screening tool.
The positive predictive values of patient groups were calculated to show agreement between the initial and final assessment.
Results
Demographics
A total of 4,503 adult patients attended during the study period. Patients were mainly under 55 years (3,536, 79 per cent) with median age band 36 to 45 years. A further 890 paediatric cases meant that entire patient attendances were 5,393 during the two-week study period.
Over half of these (3,023, 56 per cent) were from the local area, similar to the usual population (Friedman test, P>0.99) (Table 1).
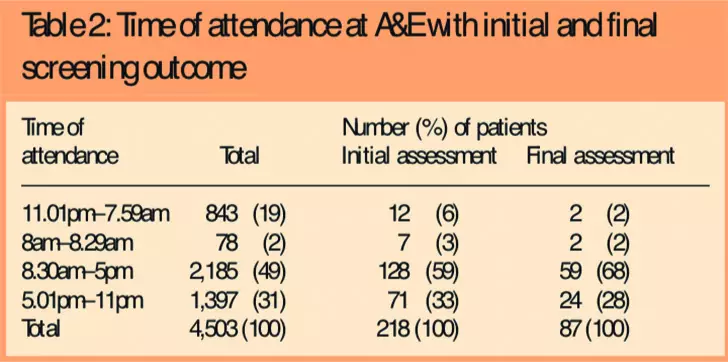
Of the 4,503 adult patients, 3,660 (81 per cent) attended when the UCC was open (Table 2).
Days of attendance (Table 3) were similar to the usual A&E attendance (Friedman test, P>0.99) with fewest patients presenting to A&E on Wednesdays and Saturdays (both 13 per cent) most on Mondays (16 per cent).
Review of notes
For 1,019/4,503 adult patients (23 per cent), electronic notes were reviewed rather than the hard copy of full notes. Of these, hard copy notes were missing for 388 patients (8.6 per cent) and 631 patients (14 per cent) attended the Adult MIU, which was on another site, therefore hard copy notes were not available for these patients.
Most patients were referred to majors and resuscitation (2,663, 59 per cent). Over a quarter (1,209, 27 per cent) were referred to the UCC and 631 (14 per cent) were seen in the Adult MIU. Of the 4,503 adult patients, 218 (4.8 per cent) were deemed suitable to be seen by the pharmacist according to the information documented during the initial nursing assessment (Table 4). Of these, 165 patients (76 per cent) attended the UCC, 12 (6 per cent) attended when the UCC was closed and 35 (16 per cent) had been seen in the Adult MIU.
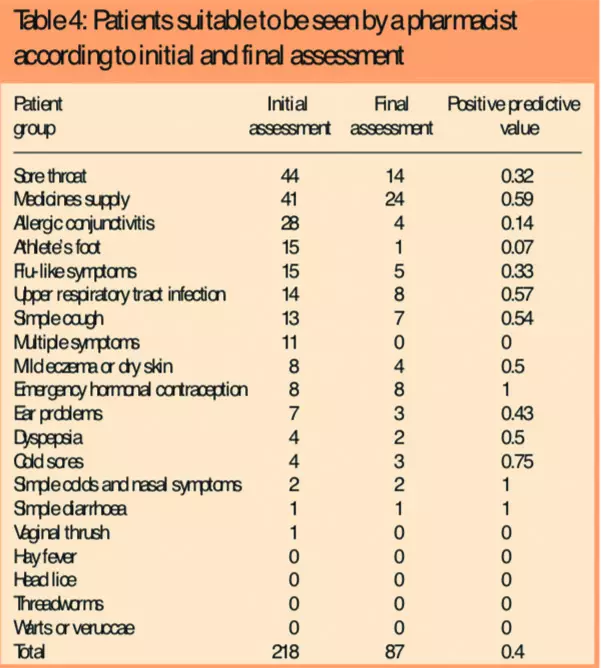
Patient destinations by final assessment were similar as 68 patients (78 per cent) attended the UCC and 17 (20 per cent) were seen in the Adult MIU. However only two suitable patients attended outside UCC hours (Table 2). Of the 218 patients identified by initial assessment only 87 (40 per cent) were suitable by final assessment. They amounted to 2 per cent of all the patients reviewed (87/4,503). The patient group with the highest difference between the initial and final assessment was those with sore throat (Table 4).
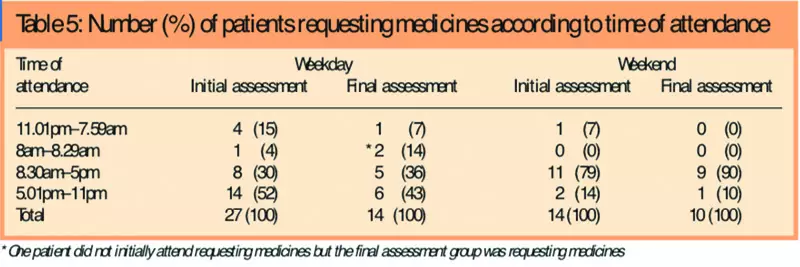
By initial assessment attendance with sore throat was highest with 44 cases (Table 4). Although 41 attendees requested medication none was referred to the pharmacist (Table 5). No cases of hay fever, head lice, threadworm, warts or veruccae were identified.
Criteria selectivity and specificity
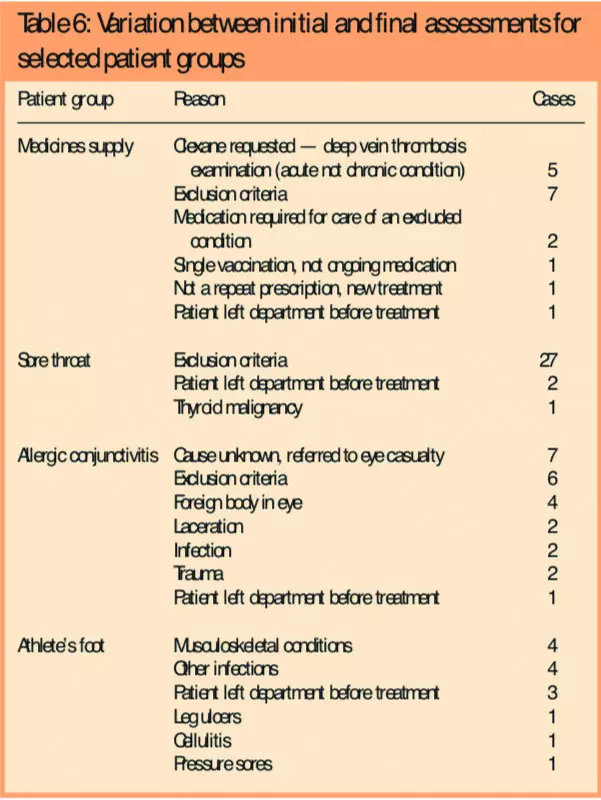
Patient groups with differences of greater than 10 cases between initial and final assessment are shown in Table 6.
The overall data showed a specificity of 97 per cent, therefore there was a high level of agreement between the proportion of patients who are not suitable to be seen by a pharmacist and the number identified as not being suitable. The overall positive predictive value was 40 per cent, indicating patients found suitable to be seen by a pharmacist were less efficiently selected, compared with the 97 per cent specificity showing unsuitable patients were appropriately categorised. A sensitivity test could not be performed on the overall results as this would require an assumption of zero false negatives.
Discussion
Objective, quick and simple to apply criteria used to identify patients who may be suitable to be seen by a pharmacist in UK A&E departments have been developed and tested. The explicit inclusion criteria are based on presenting problems likely to be reported by patients and recorded in patients’ notes at initial assessment by nursing staff. Symptoms were used rather than diagnoses, since a diagnosis is not usually available at initial assessment and the pilot study highlighted patients do not usually attend knowing their condition. The simple, explicit criteria lend themselves to prospective use at initial assessment in A&E, as nursing staff have only a short time to evaluate each patient.
The criteria have been reviewed by an experienced GP working in A&E, an experienced A&E pharmacist and a senior hospital pharmacist with both community and hospital pharmacy experience. Further review and consensus agreement by a wider expert group including primary and secondary health care professionals is planned.
Previous work in an inner London A&E department found 8 per cent (208/2,636) of patients were potentially suitable to be seen by a pharmacist, based on subjective assessment largely using pharmaceutical expertise.5 This work included 128/208 patients (62 per cent) with diarrhoea and vomiting, abdominal pain, other pain including headache and toothache, wounds, urticaria, burns and infections. These conditions were excluded in the current study either because they were thought to be well managed under current systems or were not suitable for pharmacist management. Excluding these patients from the previous study results gives 3 per cent of patients (80/2,636) potentially suitable to be seen by a pharmacist. This figure is not dissimilar to our finding using explicit criteria which can be applied independent of experience.
The discrepancy between the proportion of suitable patients found in this study compared with Bednall et al5 may partially be due to the high percentage of notes screened using electronic notes rather than hard copy. These are less detailed than paper-based notes and key symptoms or presenting complaints may not have been recorded. For patients attending A&E rather than Adult MIU, notes may have been unavailable due to misfiling or retention for follow-up as these tend to be more unwell patients. Screening of electronic notes may have systematically underestimated the proportion of patients suitable for pharmacist management.
Close agreement between demographics (age, postcode and day of attendance) in the study period compared with three months data indicates a representative sample was obtained (Tables 1 and 3).
The most common problem was medication supply by final assessment. A pharmacist is already available in the study A&E department to see this patient group. However during the study period no patients were recorded as having been seen by the pharmacist. Four-fifths of patients (19/24, 79 per cent, Table 5) requesting medicines attended when the A&E pharmacist was unavailable, eg, outside working hours or at weekends. This is likely to reflect patients’ working hours and suggests that the pharmacist could be available for longer hours such as weekends. This is in line with previous work which found 24 per cent of patients attending A&E requesting medicines were seen by the pharmacist and patients not seen attend outside office hours.16
Almost all cases (98 per cent) appropriate to be seen by the pharmacist attended when the UCC was open. This overlaps with community pharmacies usual opening hours, therefore these patients could be treated by community pharmacists. Reasons for patients attending the A&E rather than a community pharmacy could include lack of awareness of the role of community pharmacists, an impression that their condition is unsuitable for community pharmacists to deal with or the cost of over-the-counter medicines.
Streaming patients direct to a pharmacist through application of explicit criteria by a nurse at initial assessment may reduce the number of staff processing patients, reduce length of stay, increase patient convenience and may also have financial advantages. Patient acceptability of pharmacist management in A&E still requires investigation, particularly if patients had this choice in primary care and decided not to access treatment this way.
Positive predictive value varied between patient groups. Prospective application of the criteria, including nurse training, is needed to assess whether availability of the criteria during initial nurse assessment improves appropriate patient identification and positive predictive value.
The greatest variations between the initial and final assessment patient numbers occurred with medicines supply, sore throat, flu, athlete’s foot and allergic conjunctivitis. Differences between medicines supply, sore throat and flu-like symptoms were largely due to data on exclusion criteria not being documented in the initial assessment. This could be improved in prospective application of the criteria; if initial assessment nurses were familiar with the exclusion criteria they could apply them at initial assessment and refer patients direct to the pharmacist more appropriately. Low predictivity with the latter two patient groups is less easily addressed. Nurses do not examine athlete’s foot because patients are not asked to remove footwear in the waiting room. The main problem with initially included foot cases was they turned out to be musculoskeletal or lacerations of a differing nature. When initial assessment stated symptoms of “red eye” or “eye problem” which could include allergic conjunctivitis, full examination found serious problems such as foreign bodies or lacerations. The study hospital also has a 24-hour eye casualty, and most eye patients are seen in this specialist unit. Potential for pharmacists to see patients presenting with allergic conjunctivitis in hospitals which do not have specialist eye facilities may be explored with ophthalmology consultants.
No cases of hay fever, head lice, threadworms, warts or veruccae were seen. Lack of patients presenting with hay fever may have been due to seasonal variation whereas there were no cases of head lice and threadworm probably because children were excluded. None of the patients presenting with multiple symptoms was suitable to be seen by a pharmacist confirming that explicit, patient group-specific criteria should be used to select patients.
Conclusion
Explicit criteria for referral of specific groups of patients attending A&E to a pharmacist have been developed and applied. The positive predictive value varied between patient groups. The conservative criteria aimed only to identify patients clearly suitable to be seen by a pharmacist, because patients attending A&E include more complex cases than those who choose to visit a community pharmacy. This low risk approach is appropriate for A&E departments.
A minimum of 2 per cent of adult attendances at the study hospital were suitable to be seen by a pharmacist.
Acknowledgements
We thank Felicity Smith, professor in practice and policy at the University of London School of Pharmacy, for her help with this project and are grateful to A&E department staff.
This paper was accepted for publication on 30 March 2007.
About the authors
Sana Ahmed was a fourth year undergraduate at the School of Pharmacy University of London. Ursula Collignon, BPharm, MRPharmS, is senior pharmacist, emergency medicine, and
C. Alice Oborne, PhD, MRPharmS, is principal pharmacist, medicines use research, at Guy’s and St Thomas’ NHS Foundation Trust.
Correspondence to: Ms Collignon at Pharmacy Department, St Thomas’ Hospital, Lambeth Palace Road, London SE1 7EH (e-mail ursula.collignon@gstt.nhs.uk)
References
- Department of Health. 4-hour checklist: Reducing delays for A&E patients. London: DoH, 2004.
- Department of Health. Medical Practices Committee. Skill mix in primary care — implications for the future. London: DoH, 2001.
- Philips Z, Whynes D, Parnham S, Slack R, Earwicker S. The role of community pharmacists in prescribing medication for the treatment of head lice. Journal of Public Health Medicine 2001;23:114–20.
- Collignon U, Oborne CA, Ellis C. Who, why and what? Patients requesting a supply of medication in the emergency department — is this a job for the pharmacist? Pharmacy World and Science 2005;27(Suppl):A1–A14.
- Bednall R, McRobbie D, Williams D. Identification of patients attending accident and emergency who may be suitable for treatment by a pharmacist. Family Practice 2003;20:54–7.
- Department of Health. The NHS plan: a plan for investment, a plan for reform. London: DoH, 2000.
- Department of Health. Building on the best; choice, responsiveness and equity in the NHS. London: DoH, 2003.
- Minor ailment schemes can help meet access targets for PCTs, says NPA. Pharmaceutical Journal 2002;269:238.
- Royal Pharmaceutical Society. Better management of minor ailments: using the pharmacist. London, The Society, 2003.
- Department of Health. Pharmacy in the future — implementing the NHS plan. London: DoH, 2000.
- Pharmaceutical Services Negotiating Committee. Pharmacy contract, enhanced services. Available at: www.psnc.org.uk (accessed 22 June 2007).
- Davies S, Richmond PW, Hiom S. A study to identify the impact of a pharmacist working in the minor injuries area of a hospital emergency department. International Journal of Pharmacy Practice 2004;12(Suppl):R39.
- Blenkinsopp A, Paxton P. Symptom sin the pharmacy. A guide to the management of common Illness (4th ed).London:Blackwell Science Ltd, 2003.
- EdwardsC,StillmanP.Minorillnessormajordisease?Respondingtosymptomsinthepharmacy(3rded).London:Pharmaceutical Press, 2002.
- King M. Minor ailments scheme — community pharmacy. London: Lambeth Primary Care Trust, 2005.
- Collignon U, Oborne CA, Parfitt A, Ellis C. Pharmacist sees patients in the emergency department: new model of care. Pharmacy World and Science. In press.
