
JL / Science Photo Library / Shutterstock.com
Several personal stories of sepsis survivors and deaths from sepsis have been published in the media, highlighting the importance of sepsis as a major cause of preventable deaths in the UK. This article will provide an overview of sepsis with particular focus on the role of pharmacy professionals in recognition and referral.
Pathophysiology
Sepsis is characterised by a systemic inflammatory response to an invasive infection that has become unregulated[1]
. White blood cells and pro-inflammatory cytokines are released causing widespread vasodilation and an increase in capillary permeability, resulting in the loss of fluid from circulation. This results in hypovolaemia and a fall in systemic vascular resistance, which in turn leads to a fall in blood pressure and a decrease in organ perfusion, culminating in tissue hypoxia and organ failure[1]
.
There are around 250,000 cases of sepsis annually in the UK, 20% of which are fatal[1],
[2]
. The UK Sepsis Trust estimates that early diagnosis of sepsis and the application of evidence-based treatment could save 14,000 lives per year[2]
. Therefore, the timely identification of sepsis can lead to rapid treatment and potential mortality reduction.
Symptoms
Initial recognition of sepsis relies on identifying symptoms, which presents challenges for healthcare professionals as the common symptoms are not specific to sepsis and could be caused by non-infective pathology (e.g. trauma, pancreatitis, burns)[3]
.
The inflammatory-response-induced hypovolaemia affects the brain and can cause confusion, slurred speech and loss of consciousness. Similarly, as the kidneys are affected, there is a reduction in glomerular filtration resulting in a drop in urine output and development of acute kidney injury[1],[3]
.
Gas exchange across the alveoli is compromised as fluid and proteins leak into the lungs, causing a drop in systemic oxygen saturation and a rise in carbon dioxide levels. The body attempts to compensate by increasing its respiratory rate, but the problem is ultimately compounded as the drop in organ perfusion affects the lungs, meaning that even if oxygen-rich air is present, there is little blood flow with which gas exchange can take place[1],[3]
.
Initially, the heart rate increases in an attempt to compensate for the drop in blood pressure. However, the reduction in circulating volume and the fall in systemic vascular resistance ultimately undermine this action. This is because a reduction in venous return prevents the ventricles from properly filling before they contract, reducing the cardiac output[1]
.
The typical signs and symptoms of sepsis may vary across different age groups, be general or may not all be present. Examples of moderate- and high-risk symptoms include:
- Reduced urine output (e.g. dry nappies in babies and toddlers);
- Feeling cold with shivering or chills;
- Rapid breathing (increased resting breaths per minute);
- Rapid heart rate (increased resting heart rate per minute);
- Mottled (see Photoguide A) or ashen appearance;
- Cyanosis (blue tint) of skin, lips or tongue (see Photoguide B);
- Non-blanching rash (see Photoguide C)[1],[4]
,[5]
.
Additional signs in babies and young children (aged under five years)
- Not responding normally to social cues (e.g. does not smile);
- Visibly unwell (e.g. floppy or overly passive);
- Wakes only with prolonged stimulation or, if roused, does not stay awake;
- Weak high-pitched or continuous cry;
- Parent or carer is concerned that the child is behaving differently from normal;
- Has a seizure or convulsion;
- Pallor of the skin, lips or tongue;
- Cold extremities, but head and torso may be hot to the touch;
- Change in temperature (e.g. red flag temperatures are over 38o C in those aged under 3 months, 39o C in those aged 3–6 months and less than 36o C for any age)[1],[4]
,[5]
.
Additional signs that can affect patients aged over five years
- Evidence of new-onset confusion (history may be from a parent, carer, relative or friend);
- Slurred speech;
- Signs of potential infection (e.g. redness, swelling or discharge at surgical site, breakdown of the wound);
- Leg pain;
- Tympanic temperature less than 36o C;
- New onset arrhythmia[1],[4]
,[5]
.
If sepsis is suspected, the patient should be immediately referred for emergency medical assessment.
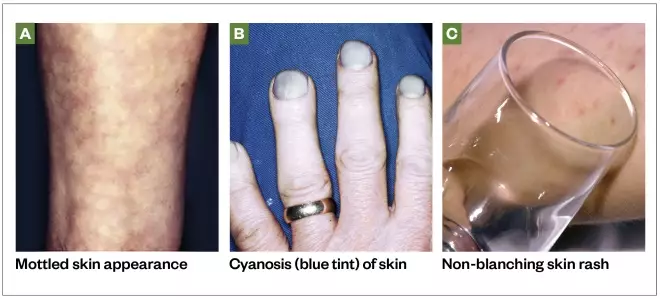
Photoguide: symptoms of sepsis
Source: Science Photo Library / Shutterstock.com
At-risk groups
Sepsis can affect anyone, but there are some patient groups that should be considered to be more susceptible to the development of sepsis, including:
- Very young children (aged under 1 year);
- Frail or older people (aged over 75 years);
- Immunocompromised people (e.g. those being treated for cancer with or without chemotherapy, post-splenectomy, taking long-term steroids or other immunosuppressant drugs);
- People who have had surgery or other invasive procedures in the past six weeks;
- People with any breach of skin integrity (e.g. cuts, burns, blisters or skin infections);
- People who misuse drugs intravenously;
- People with indwelling lines or catheters;
- Pregnant women;
- Women who have given birth or who have had a termination of pregnancy or miscarriage in the past six weeks[4]
.
Understanding the patient risk factors may help improve timely diagnosis of suspected sepsis.
Diagnosis
Sepsis can occur in response to a wide range of infections, but is most commonly associated with bacterial infection of the lungs, urinary tract, abdomen, central nervous system, or skin and soft tissues[1]
. It is primarily diagnosed by a clinical assessment. Any number or combination of signs and symptoms may be present on diagnosis.
The National Institute of Health and Care Excellence (NICE) and the UK Sepsis Trust have published risk stratification tools to facilitate appropriate recognition of sepsis and the level of risk to the patient. Most NHS organisations use these tools or a locally approved variation of them[1],[4]
. These tools cater to a wide range of patients of different ages and the recommended action differs depending on whether patients’ symptoms are recognised in the primary or secondary care setting.
Patients who meet the high-risk criteria (see Box for the criteria for children aged under five years) should be sent urgently for emergency care (at a setting with resuscitation facilities). These patients should receive intravenous antibiotics with an appropriate level of cover within one hour of recognition of sepsis, along with other treatments and investigations[1],[4]
.
Box: high-risk criteria for children aged under five years outside of the hospital setting
Behaviour
- No response to social cues;
- Appears ill to a healthcare professional;
- Does not wake, or if roused, does not stay awake;
- Weak high-pitched or continuous cry.
Heart rate
- Aged under one year: 160 beats per minute or more;
- Aged one to two years: 150 beats per minute or more;
- Aged three to four years: 140 beats per minute or more;
- Heart rate less than 60 beats per minute at any age.
Respiratory rate
- Aged under one year: 60 breaths per minute or more;
- Aged one to two years: 50 breaths per minute or more;
- Aged three to four years: 40 breaths per minute or more;
- Grunting;
- Apnoea;
- Oxygen saturation of less than 90% in air or increased oxygen requirement over baseline.
Temperature
- Aged under three months: 38°C or more;
- Any age: less than 36°C.
To see examples of mottled skin or ashen appearance, non-blanching rash of the skin, and cyanosis of the skin, lips or tongue, see the Photoguide.
Source: National Institute for Health and Care Excellence[8]
Initial blood tests should be requested to aid diagnosis and further inform on the likelihood of infection and prognosis. These should include:
- C-reactive protein — to detect inflammatory response;
- Full blood count — to detect immune response;
- Lactate — to detect tissue hypoxia.
Other investigations, such as a chest X-ray or lumbar puncture, may also be indicated depending on the likely focus of the suspected infection.
Point-of-care testing and future diagnostics
In the future, point-of-care testing facilities for key biomarkers may have a greater role in both primary care and hospital emergency departments, aiding healthcare professionals in diagnosing infection and sepsis. Recently published research into the use of sensor technologies designed to rapidly report on raised levels of biomarkers closely associated with sepsis (notably interleukin-6) may have the potential to aid sepsis diagnosis in the future[6]
,[7]
.
Case studies
Case study 1: a 12-month-old baby with suspected sepsis
A mother brings her 12-month-old daughter Alice* into the pharmacy and asks to speak to the pharmacist. The mother clearly appears concerned and expresses that Alice seems very poorly and is not her usual self.
Consultation
The mother explains that her daughter attended nursery today and the nursery staff phoned in the afternoon to report that Alice was not feeling well. As she had a temperature of 39o C, they administered a dose of paracetamol. The nursery staff also said that Alice had not been eating or drinking well and her nappies were dry all day.
Alice takes no regular medicine and has no ongoing health problems. She seems withdrawn and is not smiling or engaging with anyone, which the mother insists is unusual behaviour.
When assessing the patient, Alice’s hands feel cold despite her body and head feeling hot. During the interaction with Alice, she is noticeably very passive and inactive, and seems floppy in her mother’s arms. Alice does not appear to have a rash, though her skin appears pale.
Alice’s breathing appears very rapid.
Diagnosis
Information given in the consultation suggests that Alice may have sepsis. Use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for children aged under five years out of hospital and compare it to the information obtained during the consultation[8]
. By doing so, it is apparent that the following moderate-to-high risk criteria were demonstrated by the patient:
- Behaviour: parent or carer concern that the child is behaving differently than usual; not responding normally to social cues; no smile; and decreased activity;
- Cold hands or feet;
- Reduced urine output;
- Between 40 and 49 breaths per minute (normal resting respiratory rate for a 12-month-old is typically 20–40 breaths per minute);
- Pallor of skin, lips or tongue.
Although her temperature was high (39oC), this would only be a moderate-risk criterion if Alice was aged between 3–6 months of age outside the hospital setting.
Advice and recommendations
Alice’s symptoms clearly indicate moderate-to-high risk of sepsis. According to the risk stratification tool, Alice should be referred either for a definitive diagnosis for treatment outside the hospital (i.e. to the patient’s GP), or to hospital for further review.
Considering the risk of sepsis and the importance of timely management, referral to hospital is the best choice for this patient. Calmly and clearly explain to the mother that Alice may have a serious infection and that the best course is for her to go to the hospital immediately.
Case study 2: an 11-year-old child with a viral infection
An 11-year-old boy called Liam* is brought into the pharmacy by his parents. They explain that he has not been feeling well for the past few days. The parents want to know if Liam’s symptoms can be treated with an over-the-counter (OTC) product or whether they should take him to the GP.
Consultation
Liam has been unwell for the past three or four days and his condition does not seem to be improving. He has not yet taken any medicine for this illness. His temperature was 37.8o C when most recently checked using an ear thermometer at home.
Liam says that he has a sore throat, a cough and a blocked nose. Liam describes the severity of his throat pain as three out of ten. Liam has been eating and drinking normally, has no long-term medical conditions and takes no regular medicine.
Liam and his parents agree that his behaviour and function are normal and he appears alert and coherent through the consultation. Liam’s breathing rate does not appear to be raised and his skin and lips appear normal, with no signs of a rash.
Diagnosis
Liam may have an infection, which is likely to be viral, but does not require medical attention at present. However, to rule out sepsis, use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for children aged 5–11 years out of hospital and compare this to the information obtained during the consultation[8]
. By doing so, it is apparent that no moderate-to-high risk criteria were demonstrated by the patient.
Advice and recommendations
Liam can be treated with OTC analgesics to alleviate his throat pain and his raised temperature. Liam’s parents should ensure he is taking plenty of fluids and continue to monitor his temperature. If they become concerned about his condition, his behaviour or general functional ability, they should return to or call the pharmacy. Particular symptoms you advise them to look out for include development of a rash, if his skin becomes pale or mottled, his urine output drops, his breathing rate increases, or any general concern that mental state or activity is not normal.
Case study 3: an adult with red flag sepsis
Rahul*, a 28-year-old man, comes into the pharmacy and asks to see the pharmacist as he has begun to feel very unwell.
Consultation
Rahul works as a driver, and he fell and scraped his leg while getting out of his van the previous day. Rahul explains that at the time he did not think much about the cut, so he did not clean or dress the wound and has not yet taken any medicine for it. Although the wound began to swell and weep overnight, Rahul went into work this morning, but left when he suddenly started to feel seriously unwell — around an hour ago.
Rahul says the wound now looks much worse than it previously did. On examination you find the wound is very red and swollen, the tissue around the wound is blistering and weeping, and there are red track marks extending further up Rahul’s leg. It is clear that this wound is infected.
Rahul uses inhalers for mild asthma, but otherwise takes no regular medicine.
Rahul says he is feeling hot and sluggish, and is clearly struggling to maintain his train of thought. His condition appears to be worsening by the minute. He needs to be referred for further help, but more information is required to decide whether he is referred to his GP or to a hospital emergency department.
Rahul’s temperature is 35.8o C. His breathing appears to be rapid. His blood pressure is 92/58mmHg and his heart rate is 140 beats per minute. Rahul does not appear to have a skin rash, although his lips seem to have a blue tint.
Diagnosis
Rahul is likely to have a serious infection, which requires urgent attention. Use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for people aged 18 years and over outside of the hospital setting and compare this to the information obtained during the consultation[8]
. The patient has moderate- to high-risk criteria, such as tympanic temperature less than 36o C and signs of potential infection. He also has several high-risk criteria that require urgent referral to emergency care:
- Altered behaviour or mental state;
- Respiratory rate over 25 breaths per minute;
- Heart rate more than 130 beats per minute;
- Cyanosis of skin, lips or tongue.
Advice and recommendations
Tell Rahul that it is likely that he has a serious infection, and ask him to sit and wait in the pharmacy while an ambulance is called. It is not safe for him to drive to hospital. Share his information with the 999 operator and make another note of the details gathered during the consultation to hand over to the ambulance team upon arrival.
*All cases are fictional
Useful additional resources
- The UK Sepsis Trust. The Sepsis Manual. 2017–2018: Available at: https://sepsistrust.org/wp-content/uploads/2018/06/Sepsis_Manual_2017_web_download.pdf
- National Institute for Health and Care Excellence. Sepsis: risk stratification tools. Available at: https://www.nice.org.uk/guidance/ng51/resources/algorithms-and-risk-stratification-tables-compiled-version-2551488301
- For patients who are interested in finding out more about sepsis you can direct them to the NHS website. Available at: https://www.nhs.uk/conditions/sepsis/
References
[1] The UK Sepsis Trust. The Sepsis Manual. 2017–2018. 2017. Available at: https://sepsistrust.org/wp-content/uploads/2018/06/Sepsis_Manual_2017_web_download.pdf (accessed October 2019)
[2] The UK Sepsis Trust. Professional Resources. Available at: https://sepsistrust.org/professional-resources/ (accessed October 2019)
[3] Gotts JE & Matthay MA. Sepsis: pathophysiology and clinical management. BMJ 2016;353:i1585. doi: 10.1136/bmj.i1585
[4] National Institute for Health and Care Excellence. Sepsis: recognition, diagnosis and early management. NICE guideline [NG51]. 2016. Available at: https://www.nice.org.uk/Guidance/NG51 (accessed October 2019)
[5] National Health Service: Overview — Sepsis. 2019. Available at: https://www.nhs.uk/conditions/sepsis/ (accessed October 2019)
[6] Russell C, Ward AC, Vezza V et al. Development of a needle shaped microelectrode for electrochemical detection of the sepsis biomarker interleukin-6 (IL-6) in real time. Biosens Bioelectron 2019;126:806–814. doi: 10.1016/j.bios.2018.11.053
[7] Dolin H, Papadimos T, Stepkowski S et al. A novel combination of biomarkers to herald the onset of sepsis prior to the manifestation of symptoms. Shock 2018;49(4):364–370. doi: 10.1097/SHK.0000000000001010
[8] National Institute for Health and Care Excellence. Sepsis: Risk stratification tools. 2017. Available at: https://www.nice.org.uk/guidance/ng51/resources/algorithms-and-risk-stratification-tables-compiled-version-2551488301 (accessed October 2019)


