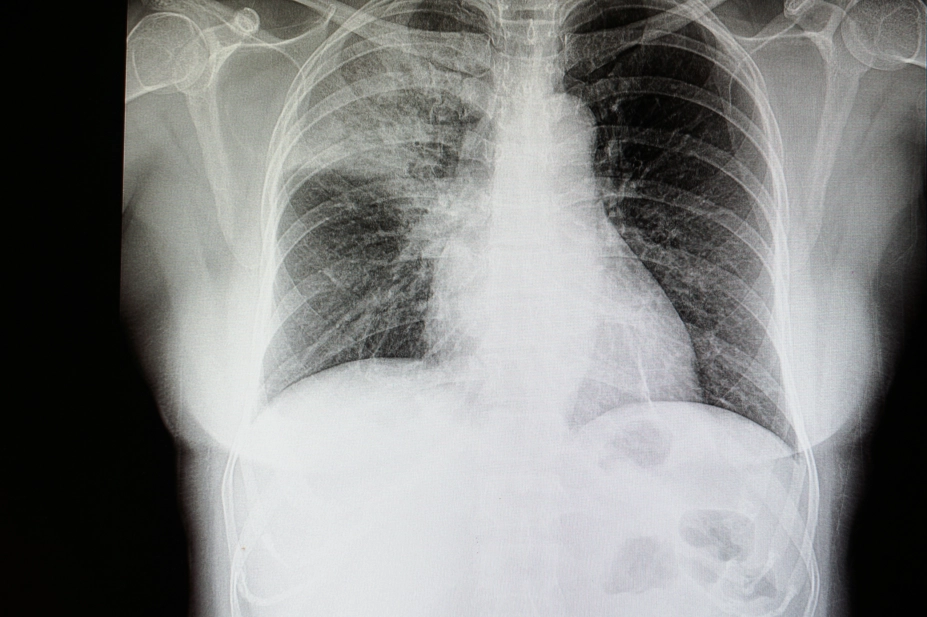
Shutterstock.com
Antimicriobial treatment for hospital and community-acquired pneumonia should be started within four hours of diagnosis, or within one hour if sepsis is suspected, according to updated guidance from National Institute for Health and Care Excellence (NICE) and Public Health England (PHE).
The final draft of the guidance, published on 16 September 2019, now also warns clinicians of the dangers associated with fluoroquinolone antibiotics.
While the guidance says that levofloxacin — a type of quinolone — may be used as an alternative to first-choice antibiotics if the patient has an allergy or a severe infection, it signposts to Medicines and Healthcare products Regulatory Agency (MHRA) restrictions and precautions when using fluoroquinolone drugs.
The guidance says the MHRA document should be consulted in light of “very rare reports of disabling and potentially long-lasting or irreversible side effects affecting musculoskeletal and nervous systems”.
The guidance update comes after the European Medicines Agency said on 11 March 2019 that medicines containing the quinolines cinoxacin, nalidixic acid and pipemidic acid, and the fluoroquinolone flumequine, should have their marketing authorisations suspended, while other fluoroquinolone antimicrobials, including those containing levofloxacin, should have restricted use.
NICE and PHE have developed two guidance documents – one for hospital-acquired pneumonia (HAP), and another for community-acquired pneumonia (CAP).
As both types of pneumonia can be life threatening, the guidance now recommends antibiotic treatment start as soon as possible “and certainly within four hours” of diagnosis or “within one hour if the person has suspected sepsis”.
While guidance published in 2014 said that patients with HAP should receive antimicrobial treatment within four hours, as should patients with CAP who are admitted to hospital, the latest version extends that advice to patients with CAP receiving non-hospital treatment in the community.
“Rapid treatment of pneumonia is vital, but these new guidelines seek to refine the length of time that patients are using antibiotics,” said Susan Hopkins, deputy director of PHE’s national infection service.
“This will contribute to efforts across the healthcare system to tackle antibiotic resistance. By supporting clinicians to make treatment decisions based on the risk factors that impact the progression of pneumonia, we can encourage appropriate and targeted use of antibiotics.”
The guidance recommends antimicrobial treatment for HAP be reviewed after five days and stopped if the patient is stable, with treatment for CAP stopped after five days, unless microbial tests, or symptoms, show a need to continue.
Commenting on the draft guidance published in February 2019, Paul Chrisp, director of the centre for guidelines at NICE, said it was important that patients with suspected pneumonia are “given the antibiotics they need as soon as possible”, adding that microbiological testing “helps determine what antibiotic will be most effective and helps limit antimicrobial resistance”.
According to the British Lung Foundation, around 220,000 people are diagnosed with pneumonia in the UK each year, with around 29,000 of those dying from the disease. This figure means the UK has the third highest pneumonia mortality rate in Europe.
The charity’s data also shows regional variation, with more cases in the East Midlands and north west of England compared with the rest of the UK.


