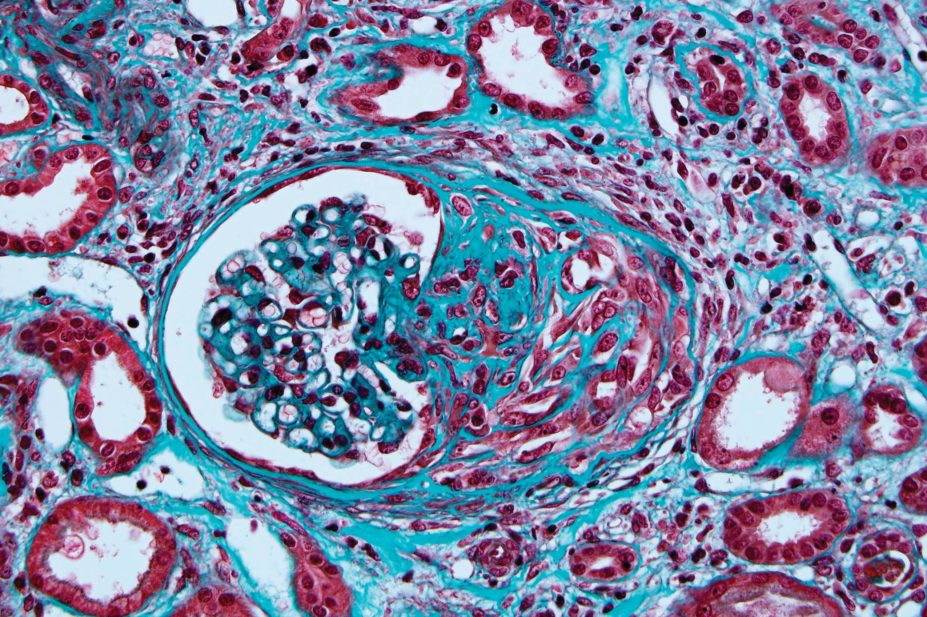
JL Kemeny ISM/Science Photo Library
Proton-pump inhibitors (PPIs), widely used for acid suppression therapy, are associated with long-term kidney damage even in patients who have not experienced acute kidney injury (AKI), according to results from a new observational study.
The researchers say the findings mean that AKI cannot be relied upon as a sole warning sign of kidney damage in PPI users.
“Our results indicate kidney problems can develop silently and gradually over time, eroding kidney function and leading to long-term kidney damage or even renal failure,” says lead author Ziyad Al-Aly, a nephrologist at the Washington University School of Medicine in St Louis, Missouri.
Their study, published in Kidney International
[1]
(online, 22 February 2017), analysed a cohort of mostly older white male veterans. The team looked at data on 125,596 new users of PPIs and 18,436 new users of histamine H2 receptor antagonists from the Department of Veterans Affairs databases.
Overall, compared with patients taking H2 blockers that suppress gastric acid by blocking the histamine receptors in acid-producing cells in the stomach, users of PPIs — that shut down the proton pumps in the stomach — were significantly more likely to develop chronic renal outcomes. These include a decline in estimated glomerular filtration rate (eGFR) to below 60ml/min/1.73m2, and eGFR decline over 30% or 50%.
PPI users were also significantly more likely to develop incident chronic kidney disease (CKD) and end-stage renal disease during the five-year follow-up.
However, the team found that only around 50% of chronic renal outcomes emerging in PPI users could be explained by AKI.
The researchers say the findings indicate healthcare professionals should pay close attention to kidney function in PPI users even if they show no signs of a problem. They should also consider whether to prescribe the drugs at all.
“In general, we always advise clinicians to evaluate whether PPI use is medically necessary in the first place because the drugs carry significant risks, including a deterioration of kidney function,” says Al-Aly.
Previous research has already linked PPIs to an increased risk of AKI, CKD and end-stage renal disease, and it was generally assumed that PPI-related AKI was a stepping stone for some patients on the way to chronic renal outcomes.

Source: Courtesy Kidney Research UK
Proton pump inhibitors may cause “slow, grumbling kidney inflammation”, says David Wheeler, professor of kidney medicine at University College London and spokesperson for Kidney Research UK
David Wheeler, spokesperson for the charity Kidney Research UK, who is also professor of kidney medicine at University College London, explains that a small proportion of patients who take PPIs will present with acute interstitial nephritis and that not all of these patients go on to fully recover their kidney function. He says that this latest research is worrying as it now indicates that PPIs may cause “slow, grumbling kidney inflammation”.
“There are patients here who clearly lost kidney function over time without presenting with acute kidney injury,” he says.
Wheeler says the research raises the question of whether PPI users should be added to the groups of patients whose kidney function should be routinely monitored through blood testing. Screening for kidney problems could be particularly prudent for PPI users with high blood pressure or other risk factors, he suggests.
The research also indicates that when a patient with CKD is taking PPIs, healthcare professionals should consider whether the drugs — some of which are available over the counter — might be driving the disease if there’s no other obvious cause, Wheeler adds.
“It’s all about awareness, at the present time,” Wheeler says. “Awareness of a potential link, and consideration that these drugs may cause, not only sudden damage to the kidney that may not get completely better, but also in the longer term they may cause a progressive loss of kidney function that’s not immediately apparent to the patient.”
References
[1] Xie Y, Bowe B, Li T et al. Long-term kidney outcomes among users of proton pump inhibitors without intervening acute kidney injury. Kidney International 2017; doi: 10.1016/j.kint.2016.12.021


