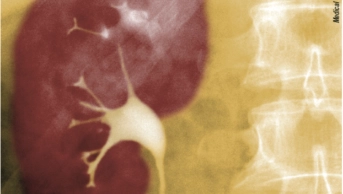
Shutterstock.com
Researchers have identified the drug classes that are frequently implicated in causing acute kidney injury (AKI) after analysing adverse drug reactions (ADRs) in a French national pharmacovigilance database.
While there were no great surprises in the final list, the data highlight which drugs are linked with this potential adverse outcome, the researchers say.
The team from Amiens University Hospital looked at all ADRs in the database reported as acute renal disease and compared them with other drug reactions recorded in the same period. The selected ADRs were recorded in the database between 1 January 2015 and 31 December 2015.
Of 38,782 ADRs recorded in the database, they found 3.2% (or 1,254 patients) were acute kidney injury in patients who had a mean age of 69 years, they reported in the British Journal of Clinical Pharmacology
[1]
(online, 14 March 2017).
In all, 434 drugs were reported as being suspected – i.e. definitely or probably responsible – of causing acute kidney injury over the year studied and 68 of those were found to be associated with a significant relative risk.
The most frequently implicated drugs in the adverse events reported were systemic antibacterials (528 reports; 29.5%); diuretics (328 reports; 18.5%); drugs acting on the renin-angiotensin system (289 reports; 16.3%); antineoplastic agents (180 reports; 10.2%); and anti-inflammatory drugs (95 reports; 5.4%).
Gentamicin, eplerenone, candesartan, cisplatin and aciclovir had the highest relative risk of causing acute kidney injury.
Two-thirds of the cases involved two or more concomitantly administered drugs, the research found, which supports other studies showing that polypharmacy is a particular risk for causing acute kidney problems.
Of patients who had suffered acute kidney damage, 15% had needed renal replacement therapy, such as dialysis and kidney transplant and 4.6% died.
Most of the drug classes identified by the researchers were already known to be linked to potential kidney problems but the database “should raise physicians’ awareness of the compounds responsible for triggering this potentially life-threatening condition”, they write.
Prescribers need to be aware of the need for “highly responsive” monitoring with treatments where the chances of nephrotoxicity are significant, they added.
Commenting on the research, Oscar Della Pasqua, chair of clinical pharmacology and therapeutics at the school of pharmacy/school of life & medical sciences at University College London, says the study had a number of limitations.
“First, we need to be aware of the fact that the figures do not reflect the true incidence of the ADRs. The reporting odds ratio corresponds to the risk of spontaneous notification of an ADR. In addition, as the authors state, the data in the database on the patient’s medical history (including chronic kidney disease and diabetes) were sparse, which prevented them from analysing other risk factors possibly associated with AKI.”
He says this is important given the fact that the drugs included in the list are used to treat acute and chronic diseases, some of which can also promote the occurrence of AKI (for example, heart failure, hypertension, diabetes, infectious diseases and cancer).
“This confounding can lead to biased estimates of the actual risk,” he says.
He also points out that the authors do not consider inter-individual differences (variability) in pharmacokinetics as a potential determinant of ADRs.
“They conclude therefore that withdrawal of nephrotoxic treatments should be considered. Such a recommendation needs to be revisited, as some drugs can be critical for the patient, for example, stopping antibiotics can lead to life-threatening complications. Instead, the use of therapeutic drug monitoring as well as the development of dosing algorithms may offer concrete opportunities for treatment personalization and ultimately reduce the incidence of AKI for these drugs.”
References
[1] Pierson-Marchandise M, Gras V, Moragny J et al. The drugs that mostly frequently induce acute kidney injury: a case − noncase study of a pharmacovigilance database. Br J Clin Pharmacol 2017; doi: 10.1111/bcp.13216