Download the full print version of the infographic here.
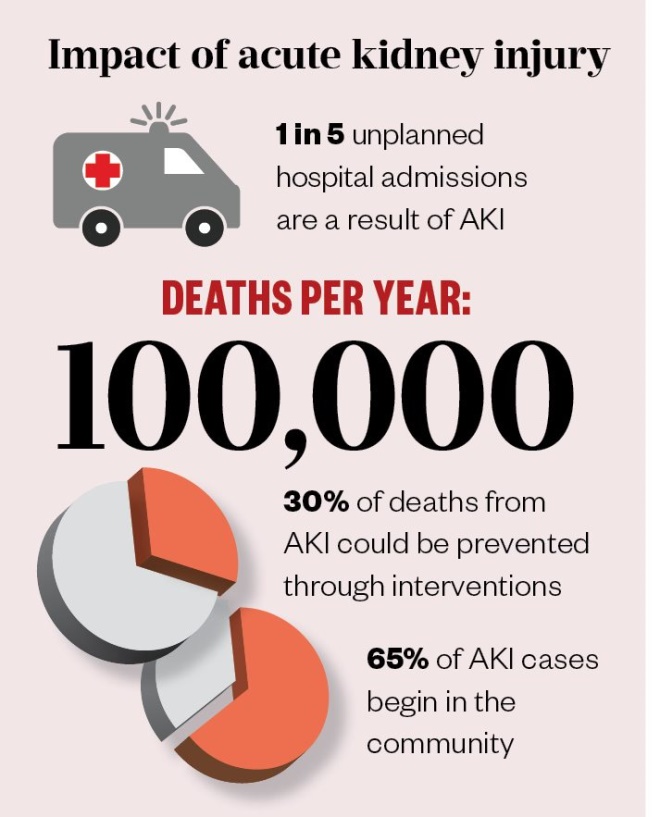
What is acute kidney injury?
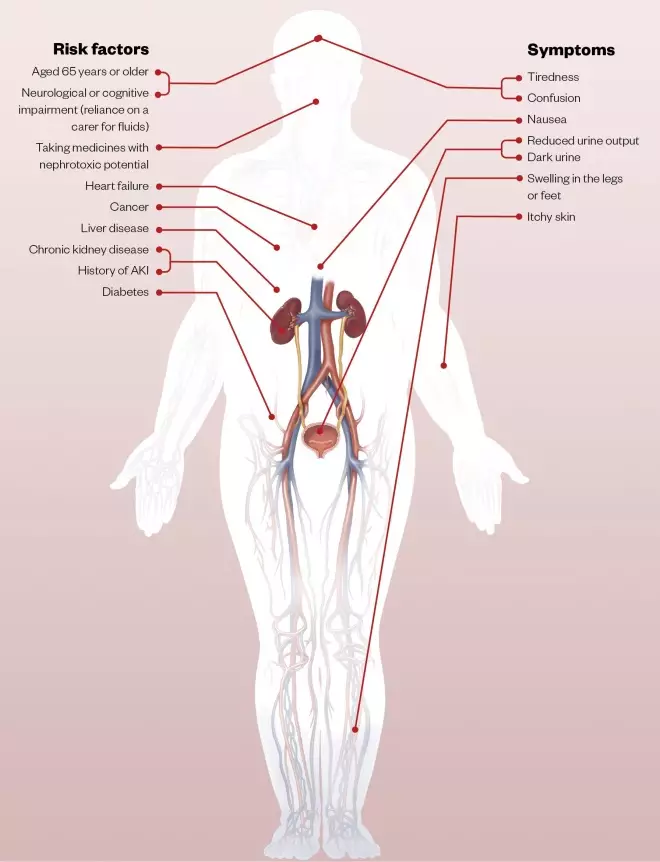
- Acute kidney injury (AKI) is a sudden reduction in kidney function. Without treatment, the balance of fluids, electrolytes and the acid-base cannot be maintained, which can lead to pulmonary oedema and metabolic acidosis;
- AKI mostly occurs as part of an acute illness, such as influenza or gastroenteritis, owing to several factors: the infection itself, loss of salt and water, and low blood pressure. This can be compounded by medicines that the patient may be taking for this or other conditions;
- The diagnosis of AKI is based on a serum creatinine increase of 26.5 micromol/L within 48 hours and a urine output of <0.5mL/kg/hour for more than 6 consecutive hours.
Causes of acute kidney injury
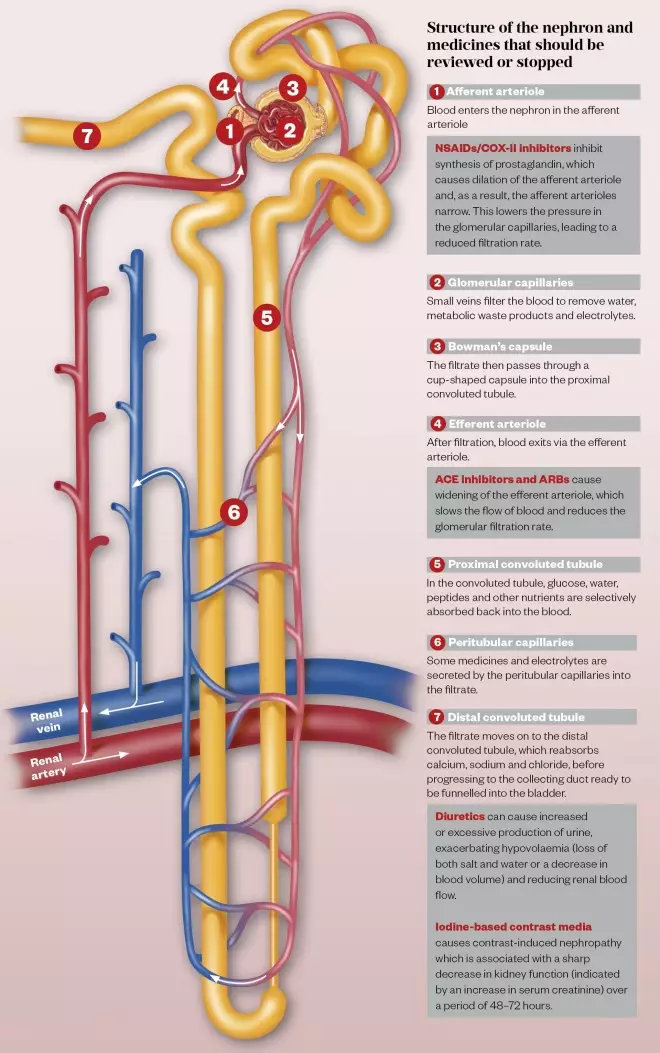
Pre-renal AKI is caused by a prolonged fall in blood pressure, often exacerbated by medicines, such as non-steroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs), in the context of acute or serious illness;
Intrinsic AKI is caused by damage to the kidney following use of certain medicines, a sustained drop in blood pressure, or as a result of kidney disease.
Post-renal AKI is caused by obstruction of urinary flow within the renal tract (e.g. owing to enlarged prostate, medicines that precipitate insoluble crystals or kidney stones).
COVID-19
Patients with COVID-19 and pre-existing chronic kidney disease (CKD) will be at increased risk of AKI through fever, reduced fluid intake, diarrhoea, and NSAIDs used for treatment of myalgias and headaches. Patients without pre-existing CKD may also develop AKI when presenting with COVID-19 and require renal replacement therapy.
Drugs that need monitoring or dose adjustment owing to accumulation or other effects on the kidneys
Analgesics
- Benzodiazepines, opioids, tramadol.
Antibiotics/antifungals/antivirals
- Acyclovir, aminoglycosides, intravenous (IV) amphotericin, co-trimoxazole, fluconazole, ganciclovir IV, penicillin, teicoplanin, tetracycline, trimethoprim, valganciclovir, vancomycin.
Antiepileptics
- Levetiracetam, pregabalin and gabapentin.
Antihypertensives
- Beta blockers, calcium-channel blockers, thiazide and loop diuretics.
Hypoglycaemics
- Dipeptidyl peptidase-4 inhibitors, metformin.
Immunosuppressants
- Calcineurin inhibitors (e.g. ciclosporin, tacrolimus), methotrexate.
Other
- Allopurinol, digoxin, lithium, low-molecular-weight heparins;
- Bisphosphonates;
- Nicorandil, nitrates.
Note: this list is not exhaustive and is only intended to act as an aide-memoire to the medicines optimisation of patients with AKI
Medicines review after acute kidney injury admission
- Eliminate potential cause (e.g. medicines with nephrotoxic potential);
- Avoid inappropriate combinations of medicines;
- Ensure all medicines are clinically appropriate;
- If a medicine must be used, amend doses appropriate to renal function, monitor blood levels of drugs wherever possible and keep course as short as possible;
- Following discharge, advise patient if and when to restart medicines.
References
ACE inhibitors: angiotensin-converting enzyme inhibitors; ARBs: angiotensin II receptor blockers; COX-II: cyclooxygenase-2
Sources: Think Kidneys, Royal College of General Practitioners, National Institute for Health and Care Excellence
Editorial adviser: Clare Morlidge, advanced renal pharmacist, East and North Hertfordshire NHS Trust
Illustration: Alex Webber

