JL / Shutterstock.com
Diabetes is often associated with damage to the kidneys, so it is no surprise that as the incidence of diabetes rises, so does the incidence of chronic kidney disease (CKD)[1]
. Around 40% of people with type 1 and type 2 diabetes (T2DM) are estimated to develop CKD in their lifetime[2]
.
In 1993, a small randomised placebo-controlled trial demonstrated the benefit of captopril (an angiotensin-converting enzyme [ACEI]) in delaying onset of diabetic nephropathy[3]
. In further randomised controlled trials, this renoprotective benefit was shown to be a class effect of ACEIs[4]
,[5]
. Then, in 2001, a large randomised double-blinded placebo-controlled trial demonstrated the renoprotective benefit of angiotensin-receptor blockers (ARBs), which provided a much-needed alternative for patients who could not tolerate ACEIs[6]
. This evidence led the National Institute for Health and Care Excellence (NICE) to recommend ACEIs and ARBs to manage CKD in patients with diabetes[7]
.
A lack of advancements in renoprotective therapies has left patients with diabetes who are intolerant of ACEIs and ARBs unprotected from declining renal function
However, since then, there have been no advancements in renoprotective therapies. This has left patients with diabetes who are intolerant of ACEIs and ARBs unprotected from declining renal function[8]
. However, that may be about to change.
Focus on cardiovascular outcomes
Cardiovascular disease (CVD) is the leading cause of mortality for patients with diabetes, so there has recently been a focus on cardiovascular outcome trials of hypoglycaemic treatments.
In 2015, the CVD outcomes trial EMPA-REG OUTCOMES (a randomised double-blind placebo-controlled trial of 7,020 patients) showed a significant reduction of major adverse coronary events, cardiovascular deaths, and hospitalisations owing to congestive cardiac failure in the 4,687 patients treated with empagliflozin, compared with the placebo group[9]
. This was the first time this benefit had been demonstrated by a hypoglycaemic agent in a randomised controlled trial since metformin in the 1998 UK Prospective Diabetes Study[10]
.
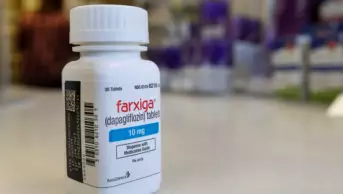
This trial was later followed by canagliflozin cardiovascular assessment studies CANVAS and CANVAS-R, as well as DECLARE-TIMI 58, which focused on dapagliflozin — all of which were multicentre randomised double-blind placebo-controlled trials that demonstrated similar cardiovascular benefits with other sodium glucose cotransporter-2 (SGLT2) inhibitors[11]
,[12]
.
And, in 2017, the CVD REAL (Comparative effectiveness of cardiovascular outcomes in new users of SGLT2 inhibitors) trial showed that the impressive CVD outcomes shown with empagliflozin were a class effect, which led SGLT2 inhibitors to be recommended by the European Association for the Study of Diabetes (EASD) and the American Diabetes Association (ADA) as second-line agents following metformin to reduce the risk of CVD in patients with T2DM[13]
,[14]
.
An added renal bonus
Sub-group analysis of these cardiovascular outcomes revealed that SGLT2 inhibitors could also benefit people with diabetes and CKD. While the analyses were not powered to demonstrate superiority, there was a trend toward reduced progression of albuminuria, reduced need for renal replacement therapies and a sustained eGFR in the canagliflozin group — benefits that required further investigation[11]
.
The CREDENCE (Canagliflozin and renal events in diabetes with established nephropathy clinical evaluation) trial, published in the New England Journal of Medicine in June 2019, was the first trial of its kind to primarily investigate the renal outcomes of hypoglycaemic agents. It showed remarkable results with the use of canagliflozin in patients with T2DM and CKD[15]
.
The trial included 4,401 patients with T2DM on standard treatment, all of whom had mild-to-moderate CKD with an estimated glomerular filtration rate (eGFR) of 30–90ml/min/1.73m2; presence of albuminuria with an albumin-creatinine ratio (ACR) of greater than 300mg/g; and were taking either an ACEI or ARB (the current gold-standard treatment). The primary endpoints investigated were composite of end-stage renal failure (requiring dialysis for at least 30 days, transplantation, or sustained eGFR of <15ml/min/1.73m2), a doubling of serum creatinine, or death from renal or CVD causes. Secondary endpoints included CVD death, myocardial infarction, hospitalisation owing to heart failure, and death from any cause.
The trial was stopped prematurely after a planned interim analysis following 405 patients reaching the primary endpoint. There was a median follow-up of 2.62 years[15]
. In this time, canagliflozin had shown a 30% reduction in patients reaching the primary endpoint of composite end-stage renal failure, compared with placebo, and this effect was consistent across all renal outcomes measured[15]
.
The evidence challenging current guidelines
Currently, SGLT2 inhibitors are licensed for initiation in patients with mild CKD (an eGFR of >60ml/min/1.73m2) and for continuation only if eGFR is consistently above 45ml/min/1.73m2. However, this licensing is based only on SGLT2 inhibitors’ efficacy for lowering blood glucose. CREDENCE showed an even greater renal benefit in patients who were initiated on canagliflozin with a baseline 45–60ml/min/1.73m2— with a 48% relative risk reduction compared with the placebo group[15]
. More importantly, this benefit was still observed in patients in the canagliflozin group, whose baseline was 30–45ml/min/1.73m2: a patient group in which SGLT2 inhibitors are not licensed. CREDENCE suggests that SGLT2 inhibitors could be used in patients with marked chronic renal impairment and albuminuria, for more than simply glucose control.
Encouragingly, CREDENCE echoed the CVD benefits seen in CANVAS and EMPA-REG OUTCOMES, in a patient group with a low eGFR in which SGLT2 inhibitors are not currently licensed for initiation. The secondary endpoint results were equally impressive in the CREDENCE canagliflozin group, with a relative risk reduction of hospitalisation owing to heart failure of 39%, and reduction of CVD death, MI or stroke by 20%[15]
.
Almost two decades have passed since the last preventative drug for T2DM-related CKD was established; this research offers a much-needed treatment option.
Possible adverse effects
However, no treatments are without risk. A higher rate of diabetic ketoacidosis (DKA) was noted in CREDENCE’s canagliflozin group, as noted in trials of other SGLT2 inhibitors[11]
,[12]
,[15]
.
Patients should be counselled on the common signs of diabetic ketacidosis: nausea, vomiting, breath smelling of pear drops, deep and laboured breathing, rapid heartbeat, and confusion
Patients with CKD and diabetes are at increased risk of metabolic acidosis owing to hyperglycaemia and insulin resistance associated with progressive nephropathy. In 2016, the Medicines and Healthcare products Regulatory Agency published guidance on SGLT2 inhibitors and the risk of DKA; there have been cases of patients on these medicines presenting with DKA without the characteristically raised blood glucose, which can delay diagnosis and treatment[16]
.
Patients should be advised to stop taking their SGLT2 inhibitor when they are unwell (‘sick day rules’), to decrease the risk of DKA, and to restart them when they are feeling well (however, patients on insulin should be reminded not to stop their insulin). Patients should be counselled on the common signs of DKA: nausea, vomiting, breath smelling of pear drops, deep and laboured breathing, rapid heartbeat, and confusion. They should be advised to seek help if they think they are developing DKA; a healthcare professional should then check their ketones.
Practice-changing results
NICE currently recommends SGLT2 inhibitors for T2DM as monotherapy when metformin, sulphonylureas or pioglitazone are inappropriate, or as a third-line option used alongside any combination of the latter[17]
. But, until recently, guidance on these agents has been based solely on evidence of their efficacy for lowering blood glucose.
CREDENCE is the first clinical trial powered to demonstrate the benefits of an SGLT2 inhibitors in T2DM-related CKD and showed fantastic results for its primary endpoint. SGLT2 inhibitors appear to not only reduce the risk of CVD, but also preserve renal function in CKD; they delay, and, in some cases, prevent the need for renal replacement therapies. They provide this benefit even in patients with low eGFR, regardless of glucose efficacy.
The results of subsequent renal outcome trials, EMPA-KIDNEY (Study of heart and kidney protection with empagliflozin) and DAPA-CKD (Study to evaluate the effect of dapagliflozin on renal outcomes and cardiovascular mortality in patients with chronic kidney disease) are eagerly awaited. NICE must consider the results of these trials, and CREDENCE — which suggests huge changes to current treatment pathways — in updates to its diabetes guidance.
The structure of our national guidance should be updated to reflect the more individualised approach adopted by the EASD and ADA, where SGLT2 inhibitors become a first-line treatment option for patients with diabetes-related CKD.
Matthew Heppel, clinical pharmacist, Hull and East Yorkshire Hospitals NHS Trust
References
[1] Diabetes UK. 2018. Available at: https://www.diabetes.org.uk/resources-s3/2019-02/1362B_Facts%20and%20stats%20Update%20Jan%202019_LOW%20RES_EXTERNAL.pdf (accessed September 2019)
[2] Diabetes UK. 2019. Available at: https://www.diabetes.org.uk/professionals/resources/shared-practice/kidney-care (accessed September 2019)
[3] Lewis EJ, Hunsicker LG, Bain RP et al. N Engl J Med 1993;329:1456–1462. doi: 10.1056/NEJM199311113292004
[4] Ravid M, Brosh D, Levi Z et al. Ann Intern Med 1998;128:982–988. doi: 10.7326/0003-4819-128-12_part_1-199806150-00004
[5] Heart Outcomes Prevention Evaluation (HOPE) Study Investigators. Lancet 2000;355(9200):253–259. doi: 10.1016/S0140-6736(99)12323-7
[6] Brenner BM, Cooper ME, Zeeuw D et al. N Engl J Med 2001;345:861–869. doi: 10.1056/NEJMoa011161
[7] National Institute for Health and Care Excellence. 2014. Available at: https://www.nice.org.uk/guidance/cg182 (accessed September 2019)
[8] Umanath K, Lewis JB. Am J Kidney Dis 2018;71(6):884–895. doi: 10.1053/j.ajkd.2017.10.026
[9] Zinman B, Wanner C, Lachin JM et al. New Engl J Med 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720
[10] UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352(9131):837–853. doi: 10.1016/S0140-6736(98)07019-6
[11] Neal B, Perkovic V, Mahaffey KW et al. New Engl J Med 2017;377:644–657. doi: 10.1056/NEJMoa1611925
[12] Wiviott SD, Raz I, Bonaca MP et al. New Engl J Med 2019;380:347–357. doi: 10.1056/NEJMoa1812389
[13] Kosiborod M, Cavender MA, Fu AZ et al. Circulation 2017;136(6):249–259. doi: 10.1161/CIRCULATIONAHA.117.02919
[14] Davies MJ, D’Alessio DA, Fradkin J et al. Diabetologia 2018;61(12):2461–2498. doi: 10.1007/s00125-018-4729-5
[15] Perkovic V, Jardine MJ, Neal B et al. New Engl J Med 2019;380:2295–2306. doi: 10.1056/NEJMoa1811744
[16] Medicines and Healthcare products Regulatory Agency. 2016. Available at: https://www.gov.uk/drug-safety-update/sglt2-inhibitors-updated-advice-on-the-risk-of-diabetic-ketoacidosis (accessed September 2019)
[17] National Institute for Health and Care Excellence. 2015. Available at: https://www.nice.org.uk/guidance/ng28 (accessed September 2019)