Shutterstock.com
In June 2016, the first wave of preregistration trainees will sit the General Pharmaceutical Council (GPhC) registration assessment in its new format. The GPhC advise that the 2016 assessment has a greater patient focus — trainees need to appreciate that the patient is at the centre of their practice. This will be reflected in the style of questions within the assessment. There may be more than one correct answer for a particular question, but candidates need to decide which would be the correct choice for the patient, based on their given particulars.
The assessment is held on one day and candidates sit two papers (See ‘Figure 1: Summary of General Pharmaceutical Council registration assessment’).

Figure 1: Summary of General Pharmaceutical Council registration assessment
The assessment is broken down into two papers. The first contains calculations and the second is multiple choice questions.
Approaching your revision
The GPhC has published a framework for the assessment that candidates should use as a foundation for revision. Trainees should ensure that they have made notes on and revised each and every outcome within the framework. The assessment is not independent from material covered in the MPharm degree course so candidates should ensure that they refer to and build on their previous learning when revising.
The framework is divided into high, medium and low weighted outcomes, which represent the proportion of questions on that particular outcome (see ‘Table 1: Weighting of questions within the GPhC framework’). However, it is important that candidates cover all aspects of the framework — not just the high and medium weighted outcomes. Missing out aspects of the framework when revising could be the difference between success and failure.
| Weighting | Proportion of questions |
|---|---|
| High | 60–70% |
| Medium | 25–35% |
| Low | Up to 10% |
Revising for calculations
The calculations assessment is a free text paper and candidates are allowed to bring a calculator. Candidates must ensure they have a GPhC-specified make and model of calculator for the assessment:
- Casio MX-8S-WE
- Aurora HC133
- Aurora DT210
Candidates should also bring a spare calculator in case of any malfunctions on the day.
Each assessment is likely to include at least one calculation question involving each of the following:
- Doses and dose regimens;
- Dosage and unit conversions;
- Estimations of kidney function;
- Displacement volumes and values;
- Concentrations (e.g. expressed as w/v, % or 1 in x);
- Dilutions, including concentrated waters;
- Molecular weight;
- Using provided formulae;
- Infusion rates;
- Pharmacokinetics;
- Health economics;
- Quantities to supply.
Calculations are all about practice so it is recommended that candidates attempt some every day during the revision period. Candidates should refer to their undergraduate notes for a refresher on how to manipulate pharmaceutical calculations. There are many books published by Pharmaceutical Press, part of the Royal Pharmaceutical Society, that can be useful learning and practice tools. There are also a range of pharmaceutical calculation apps that can be accessed on smart devices for extra practice.
Trainees should time themselves when they are revising and should try to complete each calculation in three minutes or less (for less challenging calculations). This will help with effective time management on the day of the assessment.
Revising for multiple choice questions
The second paper is made up of 120 multiple choice questions, including 90 single best answer questions and 30 extended matching questions. This is an example of a single best answer question:
Mrs RT has been taking digoxin for the past two months and furosemide for the past month. She comes in for her repeat prescription and explains that she is not feeling well. After questioning her, you suspect she is suffering with symptoms of digitalis toxicity which may have been brought on by the furosemide tablets.
You speak with the prescriber and jointly decide to discontinue the furosemide.
Which of the following medicines would be the most suitable to prescribe for Mrs RT to help reduce the risk of toxicity?
A. Bendroflumethiazide
B. Bumetanide
C. Indapamide
D. Amiloride
E. Lisinopril
Bendroflumethazide, bumetanide and indapamide are all diuretics that commonly cause hypokalaemia as a side effect. These would not be an appropriate choice for this patient because hypokalaemia may potentiate digitalis toxicity. Lisinopril may cause hyperkalaemia as a side effect but would not be the most suitable choice for this patient, because they need diuretic therapy. Amiloride is a potassium sparing diuretic that may be used to manage the hypokalaemia, which is causing the possible toxicity.
All outcomes mentioned in the GPhC framework may be tested in this paper. The GPhC has given a clear indication on the weighting of key therapeutic areas to focus on for the assessment (see ‘Table 2: Weighting of therapeutic areas’).
| Therapeutic area | Weighting |
|---|---|
| Adapted from www.pharmacyregulation.org | |
| Cardiovascular system | High |
| Nervous system | High |
| Endocrine system | High |
| Infection | Medium |
| Genitourinary tract system | Medium |
| Gastrointestinal system | Medium |
| Respiratory system | Medium |
| Malignant disease | Medium |
| Blood and nutrition | Medium |
| Musculoskeletal system | Low |
| Eye | Low |
| Ear, nose and oropharynx | Low |
| Skin | Low |
| Vaccines | Low |
| Anaesthesia | Low |
Each assessment is likely to include one or more questions on the following drugs or drug classes:
- Antibiotics
- Anticoagulants
- Antihypertensives
- Chemotherapy
- Insulins
- Intravenous drugs
- Drugs with a narrow therapeutic index
- Non-steroidal anti-inflammatory drugs
- Methotrexate
- Opiates
- Oral antidiabetic drugs
It is important that candidates do not learn by rote but rather have a deeper understanding of why certain treatments or practices occur so that they are able to make informed decisions based on individual patient cases. Trainees should be prepared to answer complex case questions that are linked to more than one therapeutic condition — for example, a patient with cardiovascular disease suffering with chronic obstructive pulmonary disease.
When revising drugs and drug classes, candidates should focus on the mechanism of action, general monitoring parameters, common and risky side effects, any cautions and contraindications and interactions.
Different methods work for different people — colourful spider diagrams often help visual learners whereas reading aloud repetitively helps others.
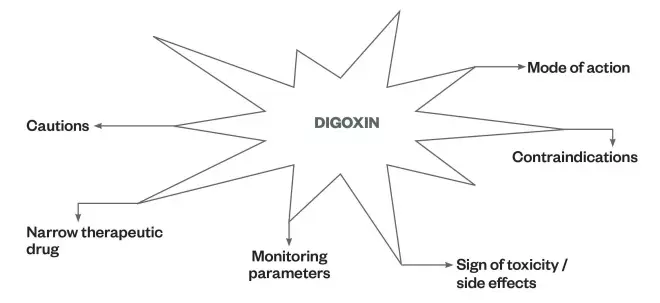
Example of a spider diagram
Creating spider diagrams can be helpful for visual learners.
It is also important to note that there may be calculation questions in paper 2, which candidates are expected to attempt without the use of a calculator. These include calculations that would be used in everyday practice as a pharmacist, such as the number of tablets needed for a particular prescription. This assesses the concept of ‘number sense’.
Using additional artefacts effectively
In paper 2 you will be provided with an extract booklet containing additional artefacts. This could have extracts from the British National Formulary (BNF), BNF for Children, medication charts, patient medication records and summaries of product characteristics (SPCs). Such extracts are helpful when assessing candidates’ application of science to practice.
SPCs are published for all legal categories of drugs — general sale list, pharmacy and prescription only medicines. It would be beneficial for candidates to familiarise themselves with the important pieces of information common to all SPCs. These are summarised below.
Qualitative and quantitative composition
This is a description of the active ingredients and their corresponding quantities.
Clinical particulars
This section forms the main body of an SPC and includes information about therapeutic indications, dosage regimen and method of administration, contraindications, special warnings and precautions for use, information collated on known interactions, effects on fertility, pregnancy and lactation, effects on ability to drive and use machines, undesirable effects and overdose.
The information contained in this section may be of particular importance if the question requires candidates to select the most appropriate dose or regimen for a patient with hepatic or renal insufficiency or is deficient in a particular liver enzyme, for example.
Pharmaceutical particulars
This section contains important information, including a list of excipients, incompatibilities, shelf life, special precautions for storage, nature and contents of container, and special precautions for disposal and other handling.
Legal category
Candidates should think about how the information in this section could be used in the assessment — for example, assessing understanding and application of law or ethics.
As part of their revision, candidates could review SPCs for the most common drugs that the assessment framework has highlighted as ‘high weighting’. If candidates are already familiar with these SPCs, they will feel more confident if they are assessed on them.
If trainees are members of a peer-learning group, each member could take responsibility for one SPC and write multiple choice questions or extended matching questions for their peers. This is an example of active learning where candidates give themselves the opportunity to ask how the information they have recently read could be used to ask and answer an exam question. SPCs are available at: http://www.medicines.org.uk/emc/.
Preparing for the assessment
In the weeks leading up to the assessment, candidates should check their emails and post for updates from the GPhC. This will include a letter detailing the venue where they will take the assessment and the time registration will open. It is advisable that candidates become familiar with the route to the venue and account for unexpected delays. It may be easier to stay near the venue the night before the assessment.
The GPhC will also provide a detailed list of which items have been approved to take into the assessment room. Candidates must adhere to these instructions and should ensure they have their belongings in order the night before.
Assessment day
On the day of the assessment, candidates should arrive in good time and try to remain calm. Once they have entered the assessment room, candidates should read the instructions on each booklet carefully. There are sample booklets available on the GPhC website so it would be beneficial to read these instructions in advance of the assessment.
Candidates should plan their time during the assessment carefully, factoring in time to check and transcribe their answers. They should read each question thoroughly, underlining key words and allowing sufficient time to process the information.
If candidates feel unsure about a particular question, they should take a deep breath and relax for a moment before thinking about the information presented logically and trying to associate it with information from revision and practice. This may involve picturing a situation from their training year where they had to use this information. If they still cannot answer the question, they should draw an asterisk next to it and move on to the next question, returning to it if there is enough time.
Useful resources
The following resources may be useful in preparing for the assessment:
- Programmes from the Centre for Pharmacy Postgraduate Education (CPPE);
- National Institute of Health and Care Excellence (NICE) Clinical Knowledge Summaries. After clicking on a topic at this link, select resources and then select ‘education and learning’. This will display clinical case scenarios, which can help consolidate useful concepts;
- NICE pathways;
- GPhC webinar on the new exam format.
Top revision tips for preregistration trainees
- Create a timeline or Gantt chart so you can plan your time and revision appropriately.
- Be realistic when creating a revision timetable — having a full-time job and juggling with completing competencies, audits and studying may be challenging.
- Start your revision in good time. Last minute cramming is not effective for this assessment — it is about understanding and deep learning.
- The BNF and BNFC should be the main reference sources for revision. Use these when revising therapeutic areas and drugs.
- Around 20% of questions in the assessment will relate to paediatric patients so it is important this is not overlooked. The BNFC is a good resource for this.
- Stay up to date with pharmacy law and ethics. This is an important aspect of being a qualified pharmacist and should not be neglected.
- Responding to symptoms is an essential component of the assessment. The CPPE has a useful package on responding to symptoms.
- Link everything you are revising together. For example, if you are revising about opioids, consider the law, how to prescribe, store and dispense the medicines, the World Health Organization’s analgesic ladder, pharmaceutical aspects etc.
- Study groups can be helpful, especially if you have a mixture of hospital and community preregistration trainees in the group.