Charlotte Gurr / The Pharmaceutical Journal
For Claire*, the fear that her 32-year-old son could be taken off the antipsychotic clozapine for the second time as a result of blood monitoring is huge.
“This outdated rule caused months of suffering. My son didn’t eat for a month; he couldn’t sleep for three months,” she says. Claire’s son was on clozapine for three years before receiving a ‘red alert’ blood test result.
“There was no negotiation. The rule meant that he had to stop all medications immediately and then retest the following day.”
Lisa* lives in fear that her 24-year-old daughter will experience the same. “The fear of every four weeks having to go for that blood test and potentially that happening is huge, because it’s the only medication that has given her a quality of life back.”
Following retests, and a period including a “horrific rebound psychosis”, Claire’s son was eventually put back on clozapine.
“He still must get his blood drawn every month to get clozapine, which exacerbates both mine and his trauma of potentially getting his clozapine stopped again, which would be catastrophic.”
Both mothers are part of the Clozapine Support Group UK — a group of carers who are campaigning for better access to the drug.
In the UK, around 37,000 people are prescribed clozapine, which is the only recommended drug for treatment-resistant schizophrenia1. First marketed as a ‘wonder drug’ for schizophrenia in the early 1970s, it was quickly withdrawn worldwide in 1975, following a series of deaths in Finland from agranulocytosis — a condition in which a patient has a severely low number of neutrophils. In the UK, clozapine is associated with around 400 deaths per year2.
Clozapine is also associated with neutropenia, a condition characterised by a reduced number of neutrophils, though it is less severe than agranulocytosis. The two conditions are distinct, primarily differentiated by the degree of neutrophil depletion – which can vary based on factors such as ethnicity and gender. Symptoms of both can include fever, chills, fatigue, a sore throat and mouth ulcers. If left untreated, agranulocytosis can lead to life-threatening infections, including sepsis, and can be fatal.
In the early 1990s, a study by Kane et al. revealed clozapine to be effective for treatment-resistant schizophrenia, leading to clozapine’s reintroduction in the UK under strict blood monitoring requirements, which have remained relatively unchanged3. However, the Medicines and Healthcare products Regulatory Agency (MHRA) announced in April 2025 that it would be reviewing the requirements in the coming months.
Currently, the monitoring requirements involve a white blood cell count, including an absolute neutrophil count (ANC), which is taken weekly for the first 18 weeks after a person starts the drug. As the risk of developing agranulocytosis and neutropenia decreases over time, the frequency of tests then drops to once every two weeks for the rest of the first year and every four weeks thereafter.
False labels
While these requirements may “sound perfectly reasonable”, says David Taylor, director of pharmacy and pathology at the Maudsley Hospital and professor of psychopharmacology at King’s College London, “the monitoring scheme tends to falsely label people as being at risk to a much greater extent than it correctly identifies people who are at risk”.
If you have two of those low neutrophil counts, then you’re prohibited from ever having clozapine again
David Taylor, director of pharmacy and pathology at the Maudsley Hospital and professor of psychopharmacology at King’s College London
“One of the reasons for this is that it uses what’s called a threshold system,” he adds. “So, if you drop below a certain neutrophil count in your blood, that kind of flicks a switch, and if you have two of those low counts, then you’re prohibited from ever having clozapine again.”
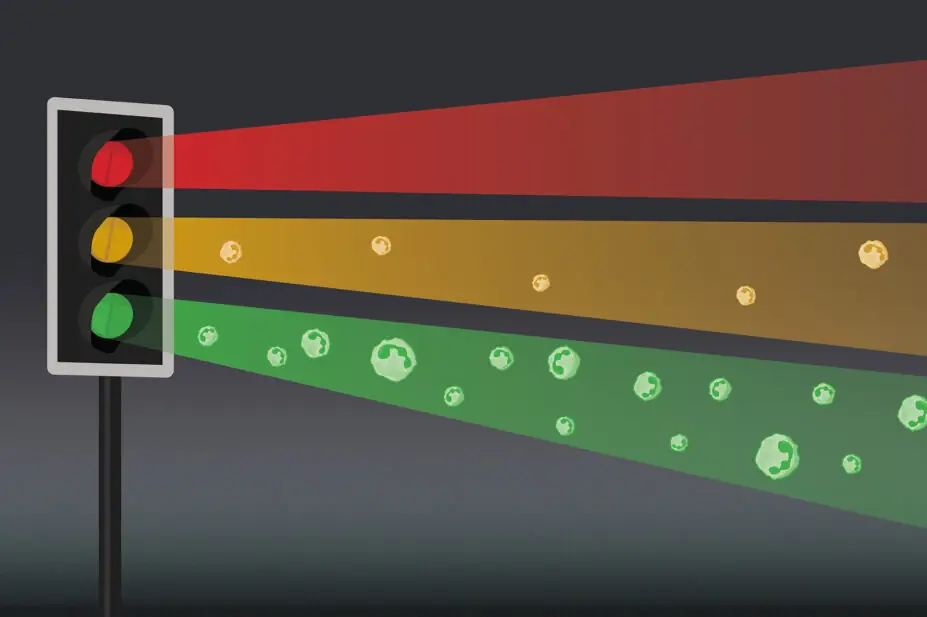
Depending on their blood test results, patients are currently assigned either:
- A ‘green’ result, meaning they can continue taking clozapine at the current dose and monitoring schedule;
- An ‘amber’ result, meaning they can continue, although with a reduced clozapine supply and more frequent monitoring;
- A ‘red’ result, which indicates blood dyscrasia and means clozapine must be stopped immediately.
If a patient receives repeated red results, they are placed on the UK Clozapine Central Non-Rechallenge Database, meaning they cannot be prescribed clozapine again, apart from in rare circumstances — for example, where the risks of withholding treatment are greater than the risks of rechallenge.
“We know that that is overdoing it,” says Taylor. “ [Our research shows] when you look at people on the non-rechallenge database and you give them clozapine again, at least 80% of them don’t get any problems again, so it’s massively overcautious.”4
Patients are also at risk of being falsely labelled “as a consequence of surveillance bias”, says Taylor.
“I don’t think clozapine really does cause neutropenia, as opposed to agranulocytosis. I think it only causes [agranulocytosis],” he adds.
“The neutropenias that you pick up are what you pick up in normal practice. So, if you do a kind of cross-sectional study of any people, you’ll find about 1% or 2% of them have neutropenia, or at least their neutrophils are low enough for it to be classed as neutropenia.
“So, you can imagine, if you keep testing people’s blood over and over again, 30 times a year, you’re going to find lots of cases of neutropenia. And then if you say, well, that’s the clozapine causing that, that’s not a conclusion that can be logically drawn,” he adds.
Further complicating things is another form of neutropenia: benign ethnic neutropenia (BEN) — a condition in which people of certain ethnicities, particularly those of African descent, are genetically predisposed to having lower neutrophil counts, without an increased risk of infection. Patients are usually diagnosed with the condition following a clinical assessment and the exclusion of other causes of neutropenia, although the condition can also be detected by genetic testing, which is not currently part of clozapine monitoring requirements.
“There’s a paper by my team … which shows that if you use genetic testing in people on clozapine, you find a lot of people have got BEN that you didn’t know about. And a lot of those people get stopped from clozapine because they drop their ANCs, but that’s perfectly normal for them. But if you don’t know that they have the BEN gene, then you assume it’s the clozapine,” Taylor explains.
There’s a kind of accidental prejudice against black people because they are more likely to have the BEN gene
David Taylor, director of pharmacy and pathology at the Maudsley Hospital and professor of psychopharmacology at King’s College London
That 2024 study, led by Taylor and colleagues, found that after genetically testing 108 patients on medium-to-long-term clozapine treatment, 26 (24%) had undiagnosed BEN5.
Owing to current monitoring requirements, Taylor adds: “There’s a kind of accidental prejudice against black people because they are more likely to have the BEN gene.”
Is monitoring still necessary?
Some experts believe that monitoring could be phased out completely, owing to evidence showing that the risk of agranulocytosis from clozapine is low. Results from a 2019 international meta-analysis of more than 260,000 people taking clozapine revealed the overall prevalence of agranulocytosis and death caused by agranulocytosis to be 0.4% and 0.05%, respectively6.
Evidence also suggests that the risk of agranulocytosis from clozapine drops over time. In 2024, a population-based study of more than 14,000 patients taking clozapine in Finland showed that the risk of developing agranulocytosis was 36 times more likely in the first 6 months for patients taking clozapine, compared with those taking other antipsychotics; however, this risk decreased to 4 times more likely after 4.5 years[7]. Out of 3,559 individuals starting clozapine during the study period, one patient died owing to clozapine-induced agranulocytosis7.
Another study by Taylor and colleagues, published in May 2025, evaluated extending blood monitoring for clozapine from every 4 weeks to every 12 weeks — a practice that was adopted during the COVID-19 pandemic — in patients who have been on clozapine for more than one year8. The study found that there were no cases of agranulocytosis among the 1,025 patients during the median follow-up of 4 years8.
However, Taylor says that even this level of monitoring is unnecessary. “If you go on the basis that real clozapine-induced agranulocytosis is a very rapidly developing catastrophic event that occurs in less than two weeks, then the further you space out blood monitoring, the less useful it becomes. I would say that monthly is nearly useless — three-monthly is definitely useless.
“In the paper, nobody got agranulocytosis in nearly 4,000 patient years, so we’re doing a hell of a lot of blood monitoring for no good purpose.”
Taylor argues instead that patients should carry a warning card and wear a bracelet, like those with diabetes or epilepsy.
“[The card] would say, ‘I am on clozapine. I may have agranulocytosis. I have developed a fever. I need an urgent full blood count’,” he says.
The international landscape
Hélène Verdoux, professor of adult psychiatry at the University of Bordeaux and a member of the European Clozapine Taskforce, agrees that monitoring should be phased out completely. “What we are asking for in the European Clozapine Taskforce is to decrease the frequency after the first year, and then to stop monthly blood monitoring after the first two years, except if there is a history of severe neutropenia.”
The European Clozapine Taskforce is a group of psychiatrists and pharmacologists practising in 18 countries under European Medicines Agency (EMA) regulation, including France, Germany and the Netherlands. Rules around clozapine monitoring are not consistent between countries, despite being under the same regulation. As a result, some countries already have less stringent rules than others, although Verdoux stresses that these are “off label”.
In France, like in the UK, there is a rule ‘no blood, no drug’ — the pharmacist is not allowed to dispense clozapine without blood results
Hélène Verdoux, professor of adult psychiatry at the University of Bordeaux and a member of the European Clozapine Taskforce
“In France, for example, like in the UK, there is a rule ‘no blood, no drug’, and that is that the pharmacist is not allowed to dispense clozapine without blood results. But in other countries in Europe, this rule does not apply,” she says.
One such country is the Netherlands, which follows recommendations from the Netherlands Clozapine Collaboration Group, established in 2006. As a result, patients have the option of stopping blood monitoring after six months, providing they are mentally competent and well informed of the risks.
Outside of Europe, the United States stopped its risk evaluation and mitigation strategies (REMS) programme for clozapine monitoring in February 2025, following an evaluation of the programme9. At the time, the US Food and Drug Administration announced that while it still recommended that prescribers monitor patients’ ANC levels, it did not expect them to participate in the REMS programme or to report results of blood tests before pharmacies dispense clozapine9.
Loss of contact
Emilio Fernandez-Egea, a consultant psychiatrist at Cambridgeshire and Peterborough NHS Foundation Trust and assistant professor in the Department of Psychiatry at the University of Cambridge, is more cautious about relaxing the rules.
He notes that while there is “overwhelming evidence” that blood monitoring for clozapine patients is not needed indefinitely, it has its benefits, including the regular contact patients have with healthcare professionals.
He argues that if the rules are relaxed. “50, 60, 70% of the people on clozapine right now will be discharged to primary care, and these are the people with the more severe end of the illness,” he says.
“They have cognitive problems, they have negative symptoms, they have a lot of side effects of the medication, and they tend to be isolated, so they don’t seek help at all. I fear that they might have difficulties in accessing the care that they might need.”
Other side effects from the drug include dizziness, drowsiness, confusion and constipation that can lead to potentially fatal complications, such as intestinal obstruction10. Lisa’s daughter, for example, struggles with constipation. “It’s taken over a year and a half to get her to be able to manage constipation better,” she explains.
“We’ve got a system now where we track it on a calendar, but before that, it was constant having to check in with her to remind her about drinking water and try and get her to eat better. And these are everyday things that we have to keep on top of. But if somebody’s on their own, it’s quite worrying, because are they going to be able to do that?”
Fernandez-Egea advocates for improving the experience of monitoring, rather than removing it completely. “For instance, wider acceptance of not using venous blood tests and using a finger prick [blood test instead], that will be a big difference.”
Finger prick tests have been introduced for patients taking clozapine at South London and Maudsley NHS Foundation Trust, which allow samples to be taken in patients’ homes and give instant results.
Fernandez-Egea adds that making clozapine clinics more flexible would also help. “For instance, [during the COVID-19 pandemic], we started having clinics outside of the normal hours, so from 17:00–19:00, in order to help people who are working full time.”
The path forward
Questions about the monitoring of clozapine patients were raised in 2023 by Louise Hunt, a senior coroner for Birmingham and Solihull, following the death of a man with treatment-resistant schizophrenia in 2022 who had been taking clozapine.
Although concluding that the cause of death was “natural causes”, Hunt wrote to the MHRA to express concern that systems were not in place to monitor abnormal levels of clozapine.
As part of the review announced in April 2025, the MHRA said it would be “seeking views in the summer [2025] from patients, patients’ families and healthcare professionals on methods to improve awareness of the risks associated with clozapine and how to manage them”. At the time of publication, the MHRA told The Pharmaceutical Journal that the review is still ongoing.
Whether the monitoring requirements change in the UK is “entirely dependent on the MHRA”, says Taylor.
Verdoux is waiting to hear the EMA’s response to the European Clozapine Taskforce’s recommendations. “If the EMA follows our suggestions, this will be a very big victory,” she says, adding that she is “convinced that if the EMA agrees, the MHRA will also agree”.
Clozapine is the medication that does significantly help people. It’s brought my daughter back to me
Lisa*, whose 24-year-old daughter takes clozapine
However, Fernandez-Egea says he is worried. “I understand the point of not doing anything that is not necessary. I think that in general, in the current NHS system or state, reducing cost is a priority. And having clozapine clinics is expensive.”
“50% of the people with psychosis in my trust are on clozapine and it’s similar everywhere … that will represent discharge of a huge amount of people. And I don’t think they’re well equipped to be in the community without the very strong support that the clozapine clinic provides.”
Whatever the outcome of the MHRA’s review of monitoring requirements, the stakes are high. Clozapine is the only treatment option that offers quality of life for thousands of people, yet its side effects can be severe — even fatal. Whichever view the experts take, patients remain at the heart of this debate.
“Clozapine is the medication that does significantly help people,” says Lisa. “It’s brought my daughter back to me.”
*Names have been changed to protect identities
- 1.Whiskey E, Barnard A, Oloyede E, Dzahini O, Taylor DM, Shergill SS. An evaluation of the variation and underuse of clozapine in the United Kingdom. Acta Psychiatr Scand. 2021;143(4):339-347. doi:10.1111/acps.13280
- 2.Fernandez-Egea E, Flanagan RJ, Taylor D, et al. Mortality associated with clozapine: what is the evidence? Br J Psychiatry. 2024;225(3):357-359. doi:10.1192/bjp.2024.88
- 3.Kane J. Clozapine for the Treatment-Resistant Schizophrenic. Arch Gen Psychiatry. 1988;45(9):789. doi:10.1001/archpsyc.1988.01800330013001
- 4.Oloyede E, Whiskey E, Casetta C, et al. Relaxation of the criteria for entry to the UK Clozapine Central Non-Rechallenge Database: a modelling study. The Lancet Psychiatry. 2022;9(8):636-644. doi:10.1016/s2215-0366(22)00188-2
- 5.Aziri H, Vallianatou K, Balgobin B, Taylor D. Genetic identification of undiagnosed benign ethnic neutropenia in patients receiving clozapine treatment. Br J Psychiatry. Published online December 9, 2024:1-5. doi:10.1192/bjp.2024.236
- 6.Li XH, Zhong XM, Lu L, et al. The prevalence of agranulocytosis and related death in clozapine-treated patients: a comprehensive meta-analysis of observational studies. Psychol Med. 2019;50(4):583-594. doi:10.1017/s0033291719000369
- 7.Rubio JM, Kane JM, Tanskanen A, Tiihonen J, Taipale H. Long-term persistence of the risk of agranulocytosis with clozapine compared with other antipsychotics: a nationwide cohort and case–control study in Finland. The Lancet Psychiatry. 2024;11(6):443-450. doi:10.1016/s2215-0366(24)00097-x
- 8.Taylor D, Gee S, Helthuis M, Oloyede E. The Safety of 12‐Weekly Monitoring of Neutrophil Count in Long‐Term Clozapine Patients. Acta Psychiatr Scand. Published online May 3, 2025. doi:10.1111/acps.13818
- 9.Frequently Asked Questions | Clozapine REMS Modification. US Food and Drug Administration. 2025. Accessed July 2025. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/frequently-asked-questions-clozapine-rems-modification
- 10.Clozapine: reminder of potentially fatal risk of intestinal obstruction, faecal impaction, and paralytic ileus. Medicines and Healthcare products Regulatory Agency. October 2017. Accessed July 2025. https://www.gov.uk/drug-safety-update/clozapine-reminder-of-potentially-fatal-risk-of-intestinal-obstruction-faecal-impaction-and-paralytic-ileus
1 comment
You must be logged in to post a comment.



Great to see this issue being discussed and acknowledgement that structures put in place to improve patient safety can end up doing the opposite. Any transition to different monitoring arrangements will need a careful approach. As described in the article, clozapine is a complex treatment with holistic monitoring (far beyond the mandated FBCs) required to use it safely and effectively. If any proposed changes are used as a reason to discharge patients from current support arrangements, that could have serious consequences. Hopefully any changes will instead facilitate a more responsive and individualised approach to monitoring for patients taking this medicine.