The pool of people at risk of overdose from a new type of super-strength synthetic opioid is widening.
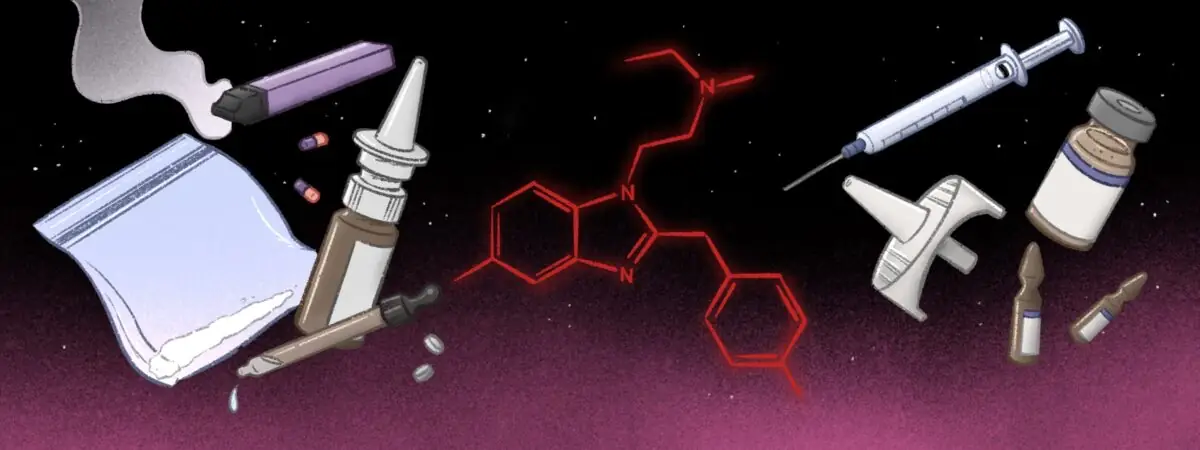
Once linked to contaminated batches of heroin, nitazenes are increasingly being found in counterfeit medicines, including benzodiazepines and oxycodone. In December 2023, a report from the Advisory Council on the Misuse of Drugs (ACMD) noted that nitazene opioids can be sold as powders or in nasal spray form and can be given intravenously or by the sublingual or nasal routes, or even by vaping[1].
The risk now is such that a national patient safety alert advised in July 2023 that NHS staff across primary and secondary care should be made aware of nitazenes’ high potency and toxicity to help avoid further overdoses[2].
What are nitazenes?
A form of synthetic opioid, 2-benzyl benzimidazole — or nitazene — opioids were first developed in the 1950s as analgesics, but were found to be so potent they were never approved or marketed as medicines[1]. Since 2019, they have re-emerged within illegal drug supplies in the United States, UK and other European countries[3].
Manufactured in a laboratory and relatively cheap to make, nitazenes can range from tens to many hundreds of times more potent than morphine, putting people at a high risk of overdose (see Table)[4]. While nitazenes are structurally unrelated to other opioids, they also bind with the mu-opioid receptor, relieving pain and evoking feelings of euphoria followed by drowsiness. Like morphine and heroin, nitazenes also suppress the respiratory system, which can result in death, but the effects of nitazenes are seen at much lower doses[3].
There are several analogues in the nitazene family, with the potential for new ones to be developed. Some of those detected in illegal drug supplies include butonitazene, isotonitazene, protonitazene and metonitazene. Etonitazene has been reported to be the most potent[4].
Caroline Copeland, senior lecturer in pharmacology and toxicology and director of the National Programme on Substance Abuse Deaths at King’s College London, says steps taken by the Taliban to dramatically cut opium production in Afghanistan prompted the appearance of nitazenes on the European heroin market. “We’ve had heroin supplies that have been adulterated by these drugs and that’s because they’re so strong and the heroin is running out.”
She adds that nitazenes have also been detected in cocaine and synthetic cannabis, known commonly as ‘spice’, as well as counterfeit medicines, including benzodiazepines and oxycodone. “That is quite a different demographic [from those injecting heroin] and so it’s a much wider risk.”
It is believed that nitazenes are often manufactured in China before being exported overseas. According to the ACMD, synthetic chemists in China began to explore the manufacturing of new psychoactive substances after legal controls were placed on the production of fentanyl and its analogues between 2016 and 2019[1].
How many deaths have been associated with nitazenes in the UK?
Synthetic opioids, such as fentanyl, have not had the same impact on drug-related deaths in the UK as they have in the United States, but there are warnings that this could be changing, with particular concerns over nitazenes as many users will be unaware of what they are taking[5,6].
Reported nitazene deaths are likely to be the tip of the iceberg
Caroline Copeland, director of the National Programme on Substance Abuse Deaths, King’s College London
Over the six months to December 2023, the National Crime Agency reported 54 deaths in the UK where nitazenes were detected in post-mortem toxicology, with 40 more awaiting results[7]. But Copeland warns that this is likely to be the “tip of the iceberg” since emerging drugs are not routinely tested for.
These latest data compare with 27 fatalities reported to be associated with nitazenes in the UK in 2021[8]. Between 2022 and 2023, nitazenes were also detected in 25 deaths in Scotland[9].
In July 2023, a national patient safety alert warned of an increased number of overdoses in many parts of England over the previous eight weeks[2]. Adulterated heroin was not the only risk, with findings of “potent synthetic opioids in fake oxycodone tablets, and less commonly in fake or ‘street’ benzodiazepines and in synthetic cannabinoids”, it said.
In November 2023, 40 overdoses were reported in Dublin in a 36-hour period, with traces of a “nitazene-type substance” found in heroin supplies[10].
Tracking synthetic opioids is not a simple task, says Amira Guirguis, associate professor of pharmacy at the University of Swansea and an expert in novel psychoactive substances, despite them starting to emerge “in a significant way”.
Guirguis says more information will be needed from drug detection systems to know what we are dealing with, since synthetic opioids are also not always included in clinical toxicology panel tests done in hospitals when treating patients for non-fatal overdose. She adds that the doses involved may be so small as to be undetectable.
The ‘Welsh Emerging Drug and Identification of Novel Substances’ (WEDINOS) drug-checking service has also detected a growth in nitazenes[8]. WEDINOS tests thousands of samples each year sent in by anonymous individuals, night clubs, drug services, healthcare providers and those working in criminal justice settings.
WEDINOS first detected nitazene in April 2021, but has since analysed 45 drug samples found to contain one of five nitazenes. These samples came from across the UK and were submitted with the belief they were something else.
What are the signs of nitazene overdose and how is it treated?
The signs of nitazene overdose are the same as for other opioids, including decreased consciousness, respiratory depression with very slow or shallow breathing, and pinpoint pupils. People might also have nausea and vomiting, be very pale and have low blood pressure or decreased heart rate. Other factors that might suggest overdose in someone who has any of these signs is a known history of drug use or chronic pain.
There is good evidence that naloxone works in cases of nitazene overdose, but delivering it rapidly and completely is “even more critical”, according to the patient safety alert. This is because progression to, and recurrence of, respiratory arrest is more likely. As a result, the duration of action of naloxone may be shorter in such cases and two or three doses may be needed[2].
These patients may require multiple dosing of naloxone
Amira Guirguis, associate professor of pharmacy, University of Swansea
Guirguis, who also chairs the Royal Pharmaceutical Society’s science and research committee, adds: “These patients may require multiple dosing [of naloxone]. We had one guy who came to our clinic, who by the time the ambulance came required 14 doses. It is something to address when someone has taken a potent opioid, one dose [of naloxone] may not do anything.”
What is the UK government doing to curb nitazene-related harm?
There is ongoing work by the National Crime Agency, police and Border Force to try to tackle the rise in synthetic opioids in the UK. There is also a cross-government synthetic opioid taskforce, involving the Department of Health and Social Care and HM Prison Service, which is reviewing the latest evidence to assess the risk of synthetic opioids to the UK, and exploring options for response should the level of risk escalate.
The government plans to introduce new police powers through the Criminal Justice Bill to crack down on anyone intending to use pill presses and encapsulators to manufacture illicit drugs such as nitazenes. In November 2023, the Metropolitan Police announced it had seized the largest ever quantity of the drugs by UK police or border officials; during a raid, it found 150,000 tablets containing a nitazene in north London.
Etonitazene and clonitazene are listed as Class A drugs under the Misuse of Drugs Act 1971 and in schedule 2 of the Misuse of Drugs Regulations 2001. There are also international controls on their use, alongside isonitazene and metonitazene. In 2023, the Home Office agreed to ban 14 more nitazenes, with tougher measures for anyone caught supplying them, including up to life imprisonment, an unlimited fine, or both. It also agreed to move etonitazene and clonitazene into schedule 1 of the Misuse of Drugs Regulations 2001[11,12].
However, Copeland says that banning more nitazenes may not make a huge difference. “We need to be treating this much more at the user level, looking at harm reduction, providing drug testing facilities, safe consumption rooms, because they have been shown to reduce fatal overdose and save lives in other countries.” She adds that King’s College is trialling naloxone delivery by drone to speed up access.
There has been much debate over introducing drug consumption rooms in the UK. In September 2023, Scotland approved the UK’s first facility, which is expected to open in Glasgow in April 2024.
Copeland adds that there is likely to be a high level of awareness of the dangers of nitazenes among heroin users, but less so for those who, for example, buy benzodiazepines or oxycodone off the dark web.
In a paper published in January 2024, Copeland noted that “high levels of structural and social stigma pose a key barrier to drug policy innovation”, preventing initiatives that may reduce deaths[4].
What can pharmacy staff do to support drug users to minimise risks of nitazenes?
Kevin Ratcliffe, a consultant pharmacist in addictions, who leads a specialist service in north Birmingham, West Midlands, and national non-medical prescribing lead for national health and social care charity ‘Change, Grow, Live’, says pharmacy has a vital role in communicating risks and promoting harm reduction as well as providing naloxone.
“We had a spike in [nitazene] overdose deaths in the summer [2023] and they are pinging up all around the country as dealers and service users are experimenting with it,” he says.
The drop off in quality of heroin, together with prices going up, has led some people to start looking at other drugs, such as benzodiazepines and synthetic opioids, he adds.
In Birmingham, all commissioned pharmacies carry naloxone and display stickers in their windows to advertise that they have it on site if patients need it, he explains. “It is also about knowing that you may need more than one naloxone injection and that’s OK. Our commissioned pharmacies supply naloxone and they are trained to administer it, and in emergency, they need to.”
Community pharmacies are right on the front line, so they need to be aware of it
Kevin Ratcliffe, consultant pharmacist in addictions, who leads a specialist service in Birmingham
Ratcliffe says the most powerful weapon we have against synthetic opioids is education. “Community pharmacies are right on the front line, so they need to be aware of it. My organisations and others have been very keen to push that out to community pharmacies.”
He suggests that pharmacy teams that want to know more about how to help should get in touch with their local drug addiction service, which can advise further.
- 1Advisory Council on the Misuse of Drugs. ACMD advice on 2-benzyl benzimidazole and piperidine benzimidazolone opioids. Gov.uk. 2023. https://www.gov.uk/government/publications/acmd-advice-on-2-benzyl-benzimidazole-and-piperidine-benzimidazolone-opioids/acmd-advice-on-2-benzyl-benzimidazole-and-piperidine-benzimidazolone-opioids-accessible-version (accessed 30 January 2024)
- 2Office for Health Improvement and Disparities. Potent synthetic opioids implicated in heroin overdoses and deaths. Central Alerting System. 2023. https://www.cas.mhra.gov.uk/ViewandAcknowledgment/ViewAlert.aspx?AlertID=103236 (accessed 30 January 2024)
- 3Pergolizzi Jr J, Raffa R, LeQuang JAK, et al. Old Drugs and New Challenges: A Narrative Review of Nitazenes. Cureus. 2023. https://doi.org/10.7759/cureus.40736
- 4Holland A, Copeland CS, Shorter GW, et al. Nitazenes—heralding a second wave for the UK drug-related death crisis? The Lancet Public Health. 2024. https://doi.org/10.1016/s2468-2667(24)00001-x
- 5Transform Drug Policy Foundation. Responding to nitazenes in the UK drugs market. Transform Drug Policy Foundation. 2023. https://transformdrugs.org/blog/responding-to-nitazenes-in-the-uk-drugs-market (accessed 30 January 2024)
- 6Davidson C. Nitazenes: synthetic opioids more deadly than fentanyl are starting to turn up in overdose cases. The Conversation. 2023. https://theconversation.com/nitazenes-synthetic-opioids-more-deadly-than-fentanyl-are-starting-to-turn-up-in-overdose-cases-212589 (accessed 30 January 2024)
- 7Homer A, Johal N. Street drugs stronger than heroin linked to 54 deaths in UK. BBC News. 2023. https://www.bbc.co.uk/news/uk-67589364 (accessed 30 January 2024)
- 8WEDINOS. PHILTRE Annual Report 2022/23. Wedinos.org. 2023. https://www.wedinos.org/resources/downloads/Annual-Report-22-23-English.pdf (accessed 30 January 2024)
- 9Public Health Scotland. Update on new synthetic drugs. Public Health Sotland. 2023. https://publichealthscotland.scot/news/2023/december/update-on-new-synthetic-drugs/ (accessed 30 January 2024)
- 10Health Service Executive. Nitazenes detected in heroin samples related to Dublin overdose cluster. Health Service Executive. 2023. https://www.hse.ie/eng/services/news/media/pressrel/nitazenes-detected-in-heroin-samples-related-to-dublin-overdose-cluster.html (accessed 30 January 2024)
- 11Home Office. Synthetic opioids to be banned as government acts to stop drug deaths. Gov.uk. 2023. https://www.gov.uk/government/news/synthetic-opioids-will-be-banned-as-government-acts-to-stop-drug-deaths (accessed 30 January 2024)
- 12Home Office. Fifteen new synthetic opioids to be made illegal. Gov.uk. 2023. https://www.gov.uk/government/news/fifteen-new-synthetic-opioids-to-be-made-illegal (accessed 30 January 2024)