
Courtesy of P1vital

Source: Huan Tran / Alamy Stock Photo
When a patient seeks help for depression, the doctor plays a primitive guessing game. Although surrounded by state-of-the-art equipment, the doctor may touch only a keyboard to record the patient’s symptoms and history before producing a prescription for an antidepressant. But it takes weeks to months to determine whether the drug really works.
“It’s kind of shocking how little we have to go on for a life-ruining disorder like depression,” says Leanne Williams, a researcher in psychiatry and behavioural sciences at Stanford University, California. “In any other area of medicine, for a really chronic disease like this, you’d have other information.”

Courtesy of Leanne Williams
Leanne Williams, a researcher in psychiatry and behavioural sciences at Stanford University, says that it can take some patients years to find an antidepressant that works
Around 350 million people worldwide suffer from depression, a condition that is more than just occasionally feeling down. People with depression have an unremitting low mood, and lack of interest in activities they previously enjoyed. The condition is estimated to cost billions in lost productivity in the UK and the United States, and ranks as the second leading cause of disability around the world.
Depression’s large contribution to disability comes, in part, from the prolonged trial and error in treatment: only one-third of patients with the condition get relief from the first antidepressant they try, while the remaining two-thirds try other drugs, often many, and sometimes for years[1]
.
“They’re the ones who end up really unwell, really unable to work, and with a lot of other co-morbid disorders, like diabetes and obesity,” says Williams.
But researchers hope to match patients to an effective drug from the beginning of their treatment by searching for tell-tale features that could predict how they will respond to a particular antidepressant. This personalised approach draws on a range of biological measures, including genetic variation, inflammation-related molecules, and methods of assaying brain function. Ultimately, a combination of these measures — a “biosignature” — may prove most useful.
The growing roster of biomarkers is promising; however, these signs must be tested prospectively to see if they really do predict treatment response. This testing is about 50 years behind that of other diseases, such as cancer or cardiovascular disease, says Madhukar Trivedi, a psychiatrist and depression researcher at the University of Texas Southwestern Medical Center.
Getting personalised
Currently, treatment for depression involves a haphazard improvisation. There is no standardised path, which reflects the heterogeneous nature of depression: one person’s illness may arise for different biological reasons than another’s. One treatment does not fit all.
Luckily, there are lots of treatments to choose from: more than 30 antidepressant medicines, several psychotherapy approaches, and even the drastic, yet effective, electroconvulsive therapy (ECT). The popular selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine and sertraline, are the first-line drug treatment. If after about six weeks on an SSRI, a person with depression has not “responded” — experienced a substantial improvement in their depression scores as measured by a questionnaire — a clinician may opt to increase dosage, or prescribe additional medicines in the same drug class. If there is still no improvement at 12 weeks, the prescriber may consider a switch to a different drug class, such as serotonin and norepinephrine reuptake inhibitors (SNRIs) like venlafaxine, or the older, more side-effect laden, tricyclic antidepressants. Additional talk therapies or exercise may also be recommended.
This armamentarium may soon include therapies such as transcranial magnetic stimulation or ketamine infusions, which seem to relieve depression in some patients almost immediately. But for now, the treatment process is a slow-motion spin at the roulette table — with each treatment change comes a good dose of waiting.
To improve the odds, researchers are trying to decipher which features predict a response to a particular antidepressant. Grouping people based on their clinical symptoms has not proven useful[2]
but more quantifiable biological features have shown promise. Researchers’ investigations have largely occurred on the sidelines of clinical trials designed to test drug efficacy, so not every participant may have given blood or had a brain scan to provide potential biomarker data, which dilutes the power to find a meaningful biomarker.
But two large studies dedicated to finding biomarkers for antidepressant response are changing that. The Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care (EMBARC) trial tracks genes, proteins found in blood, brain function, and cognitive tests in more than 300 people randomised to receive either sertraline or placebo. The study will combine this information to define a profile of features that identifies those who would do better on sertraline or placebo. Trivedi, the trial’s principal investigator, expects the first results to be published by mid-2017.

Courtesy of Madhukar Trivedi
Madhukar Trivedi, a psychiatrist and depression researcher at the University of Texas Southwestern Medical Center, is leading a study to find biomarkers to predict antidepressant response
The second study, the international Study to Optimize Treatment for Depression (iSPOT-D) takes a similar approach, and looks for biomarkers in patients that can predict how people with depression will react on one of three antidepressants: sertraline, escitalopram or venlafaxine. Initial reports from the project, which involves 20 sites across 5 countries, suggest that certain genetic variants, brain activity and connectivity, and childhood trauma are strong predictors of treatment response[3],[4],[5],[6]
. Prospective testing will confirm whether or not using these biomarkers to guide antidepressant choices significantly reduces the time to respond, says Williams, who headed iSPOT-D.
The brain doesn’t function in isolation, it functions in a context of your psychosocial environment — factoring that in is complex, but important
Even if the biomarkers are good predictors, they are by no means deterministic — a person’s lifestyle may well override a biomarker’s forecast, just as a heart drug is unlikely to improve cardiovascular health if a person eats poorly or remains sedentary.
“The brain doesn’t function in isolation, it functions in a context of your psychosocial environment,” Williams says. “Factoring that in is complex, but important.”
Molecular markers
Treatment response can run in families, so a person’s genes may also affect the level of relief they obtain from treatment for depression. Researchers can scan the entire genome for variants, but three such studies failed to detect any associations with treatment response in depression, even when their results were combined[7]
. Genetic variants may have only subtle effects, and even larger studies would be needed to locate them.
Several genetic tests are commercially available, if not yet in widespread use, despite the lack of evidence for genetic influences in depression treatment response. Personalised medicine company Genomind sells a test that scans DNA obtained by a cheek swab for variants in 18 different genes to guide medication decisions for a range of psychiatric disorders, including depression. Many of these genes are known targets of psychiatric drugs, so slight variations in their action could make a difference to how people respond to them.
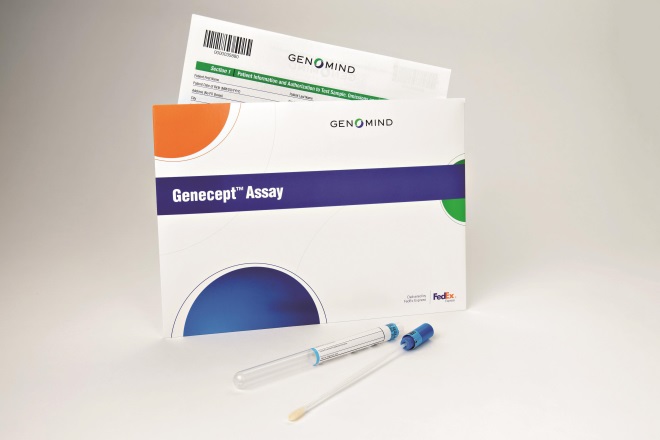
Source: Genomind
Genomind sells a test that scans DNA obtained by a cheek swab for variants in 18 different genes to guide medication decisions for a range of psychiatric disorders, including depression
SSRIs, for example, target SLC6A4, a gene that encodes a protein that shuttles the neurotransmitter serotonin back into cells, which terminates its action on neurons. A certain SLC6A4 variant increases the chance that someone will not respond to SSRIs and may have side effects when using them. With this information in hand, a clinician may decide to use an SNRI right away, rather than choosing the usual first-line SSRI treatment.
Other variants in genes encoding enzymes important for drug metabolism can identify whether someone is a slow or fast metaboliser, which could help to determine dosing.
“All the genes in our panel were chosen because they can give clinically actionable information,” says Kristina Habermann, vice president of marketing at Genomind. “We don’t see the test as a be-all-end-all, but as a tool in a clinician’s toolkit.” The company is currently conducting a randomised controlled trial to see if using the test does, in fact, reduce the time to treatment response.
Others have found clues in markers of pro-inflammatory molecules found in blood. In June 2016, researchers from King’s College London reported that the level of mRNA for macrophage migration inhibitory factor and interleukin-1β could flag people least likely to respond to antidepressants. All those with levels above a certain cut-off were correctly classified as non-responders, and most of those below the cut-off were correctly classified as responders; however, around 40% with low values were in fact non-responders[8]
.
It doesn’t matter whether inflammation is a cause or consequence of depression — the most important thing is that it can help identify the right treatment for patients
Inflammation might sabotage antidepressant action, says Annamaria Cattaneo, a postdoctoral fellow who ran the study, so if a person has high levels of pro-inflammatory molecules, a clinician may augment treatment with a different antidepressant or anti-inflammatory medicines. Other studies have also pointed to gains from exercise[9]
or infliximab[10]
, an anti-inflammatory agent, only in those depressed patients with elevated levels of other pro-inflammatory molecules.
“It doesn’t matter whether inflammation is a cause or consequence of depression,” Cattaneo says. “The most important thing is that it can help identify the right treatment for patients.”
Brain-based readout
Personalised treatment may pay off more quickly if researchers look directly at the organ of interest, rather than genetic or molecular markers that act throughout the body. Still, researchers hope to eventually match molecular markers with particular brain states, which can be probed with brain scans using magnetic resonance imaging, measures of brain activity called electroencephalograms, or even cognitive testing. These investigations may reveal distinct types of brain dysfunction at play in people with depression, and one type may require a different treatment from another.
One effort to test this approach, the Research on Anxiety and Depression (RAD) project, includes anyone who is experiencing depression, anxiety, or distress. The study’s large population of people who are not taking medication for their conditions increases the power to detect brain profiles associated with these symptoms before they are treated.
“We hope to get a set of types at baseline of how those brain systems look,” says Williams, who is leading the project. Using data from RAD, ISPOT-D and multiple other studies, Williams has proposed a taxonomy of eight brain types relevant to depression and anxiety. She suggests that one mixture of two types characterises people who are less likely to respond to first-line SSRIs: they have a rumination brain state, marked by an overactive brain at rest, as well as an anhedonia brain state, in which the neural circuits for processing reward are insensitive to things that usually give pleasure[11]
.
Beyond response to antidepressants, researchers have found markers in people who are likely to benefit from ECT in a brain region called the subgenual cingulate cortex[12],[13]
. Although ECT is largely effective, it doesn’t work for everyone. Predicting patients’ responses to ECT before it is initiated could spare them unnecessary treatment, which involves two to three weeks of ECT, given every other day, under anaesthesia.
“No one would voluntarily go through a course of ECT for nothing,” says Anil Malhotra, who led one of the studies. “If you had a brain scan that predicts failure to respond, then we could go directly to trying something else.”
A cognitive shortcut
Another shortcut through the trial and error process is based on the finding that antidepressants can quickly change the thinking styles of people with depression, who pay more attention to negative things, like sad or angry faces, and interpret ambiguous stimuli such as a slight smile as unpleasant, like derision. These biases fuel depression.

Courtesy of Catherine Harmer
Catherine Harmer, a cognitive neuroscientist at the University of Oxford, is testing the hypothesis that antidepressants work by changing the thinking styles of people with depression, rather than by directly making them feel happy
“That led us to hypothesise that antidepressants work by changing these cognitive biases, rather than by directly making people feel happy,” says Catherine Harmer, a cognitive neuroscientist at the University of Oxford. “The drugs may just affect more subtle processes in how you pick up information, which would make you positive after a while, but not immediately.”
The drugs may just affect more subtle processes in how you pick up information, which would make you positive after a while, but not immediately
Earlier studies by Harmer and colleagues found that, when beginning to take an antidepressant, people with depression who showed greater improvement in accurately recognising emotions in faces flashed on a computer screen were more likely to have a lifted mood weeks later[14]
. A new study called PReDicT (Predicting Response to Depression Treatment) will test this prospectively: if the ability to recognise facial emotion does not change after a week on an antidepressant, a person will be switched to a different drug. The project, funded by a grant from the EU’s Horizon 2020 research and innovation programme, will then measure whether using the test actually decreases the time it takes to get relief compared with treatment as usual.

Courtesy of P1vital
A new study called PReDicT (Predicting Response to Depression Treatment) is testing whether a particular drug can change a person’s ability to recognise facial emotions, and whether using this test can shorten the time to find an effective treatment
Harmer’s approach doesn’t seek to predict the best antidepressant before treatment, but it provides an early and personalised outlook. “You can ask whether a particular medicine is working at a particular dose in a particular person at a particular time,” Harmer says. “It’s a very specific prediction for what [the treatment is] doing right there and then.”
Personalising treatment will come in steps, predicts Trivedi. Laboratory tests in the near future will guide clinicians toward a set of medications and away from others. A truly personalised selection will come later. “My sense is that in 10–20 years, hopefully earlier, we may get to a lab test that tells the doctor to give one treatment — be it medication, exercise, psychotherapy or some form of neuromodulation — and avoid ten others, making your chances of getting relief profoundly better,” he says.
References
[1] Trivedi MH, Rush AJ, Wisniewski SR et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28
[2] Arnow BA, Blasey C, Williams LM et al. Depression subtypes in predicting antidepressant response: a report from the iSPOT-D trial. Am J Psychiatry 2015;172:743–750. doi: 10.1176/appi.ajp.2015.14020181
[3] Schatzberg AF, DeBattista C, Lazzeroni LC et al. ABCB1 genetic effects on antidepressant outcomes: a report from the iSPOT-D trial. Am J Psychiatry 2015;172:751–759. doi: 10.1176/appi.ajp.2015.14050680
[4] Grieve SM, Korgaonkar MS, Gordon E et al. Prediction of nonremission to antidepressant therapy using diffusion tensor imaging. J Clin Psychiatry 2016;77:e436–43. doi: 10.4088/JCP.14m09577
[5] Gyurak A, Patenaude B, Korgaonkar MS et al. Frontoparietal activation during response inhibition predicts remission to antidepressants in patients with major depression. Biol Psychiatry 2016;79:274–281. doi: 10.1016/j.biopsych.2015.02.037
[6] Williams LM, Debattista C, Duchemin AM et al. Childhood trauma predicts antidepressant response in adults with major depression: data from the randomized international study to predict optimized treatment for depression. Transl Psychiatry 2016;6:e799. doi: 10.1038/tp.2016.61
[7] GENDEP Investigators, MARS Investigators, STAR*D Investigators. Common genetic variation and antidepressant efficacy in major depressive disorder: a meta-analysis of three genome-wide pharmacogenetic studies. Am J Psychiatry 2013;170:207–217. doi: 10.1176/appi.ajp.2012.12020237
[8] Cattaneo A, Ferrari C, Uher R et al. Absolute measurements of Macrophage Migration Inhibitory Factor and Interleukin-1-β mRNA levels accurately predict treatment response in depressed patients. Int J Neuropsychopharmacol 2016. doi: 10.1093/ijnp/pyw045
[9] Rethorst CD, Toups MS, Greer TL et al. Pro-inflammatory cytokines as predictors of antidepressant effects of exercise in major depressive disorder. Mol Psychiatry 2013;18:1119–1124. doi: 10.1038/mp.2012.125
[10] Raison CL, Rutherford RE, Woolwine BJ et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry 2013;70:31–41. doi: 10.1001/2013.jamapsychiatry.4
[11] Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry 2016;3:472–80. doi: 10.1016/S2215-0366(15)00579-9.
[12] Argyelan M, Lencz T, Kaliora S et al. Subgenual cingulate cortical activity predicts the efficacy of electroconvulsive therapy. Transl Psychiatry 2016;6:e789. doi: 10.1038/tp.2016.54
[13] Redlich R, Opel N, Grotegerd D et al. Prediction of individual response to electroconvulsive therapy via machine learning on structural magnetic resonance imaging data. JAMA Psychiatry 2016;73:557–564. doi: 10.1001/jamapsychiatry.2016.0316
[14] Tranter R, Bell D, Gutting P et al. The effect of serotonergic and noradrenergic antidepressants on face emotion processing in depressed patients.J Affect Disord 2009;118:87–93. doi: 10.1016/j.jad.2009.01.028


