Fanatic Studio / Alamy Stock Photo
High blood pressure, or hypertension, is one of the biggest risk factors for premature death in the UK, yet as many as 7 million people are unaware they have it[1]
. Often referred to as the ‘silent killer’, hypertension rarely causes symptoms and is often only diagnosed after a heart attack or stroke. According to a 2017 report by now defunct community pharmacy trade association Pharmacy Voice[2]
, only around a third of adults with hypertension are both diagnosed and managed to recommended levels – that is, below 140/90mmHg for patients aged under 80 years or below 150/90mmHg for those aged over 80 years[3]
.
“Hypertensives are quite a hard group to reach,” explains Alison Warren, consultant cardiology pharmacist at Brighton and Sussex University Hospitals NHS Trust. “[People] don’t feel unwell with high blood pressure, so we’re trying to tackle people who have had high blood pressure for some time but nobody’s ever really told them they should be concerned.” It is not easy to get them to come in for a review, she adds.

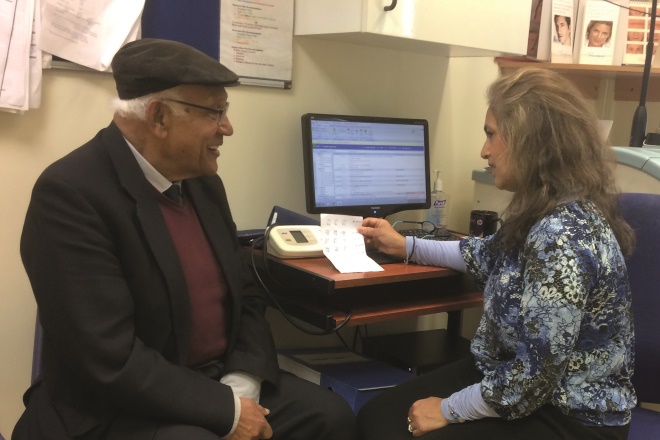
Source: Courtesy of Alison Warren
Alison Warren, consultant cardiology pharmacist at Brighton and Sussex University Hospitals NHS Trust, says that hypertensives are a hard group to reach.
In 2015, as part of a wider hypertension project in Brighton, Warren was asked to run a six-month pilot in a GP practice[4]
. The aim was to evaluate whether a regular, weekly clinic conducted by a pharmacist prescriber could help patients with hypertension optimise their medicines.
The patients, ranging from those who had been prescribed medication to those recently diagnosed, attended between one and five appointments. At the end of the project, 55% of patients were discharged because they had achieved their blood pressure targets. Following its success, Warren is working to expand the service for a group of GP practices.
But GP practices are not the only clinical setting in which pharmacists can provide hypertension services. Secondary care cardiovascular pharmacists in London are now demonstrating how they can provide value in the community and help to free up the time of hypertension consultants in hospitals. And community pharmacies are being recognised by Public Health England (PHE) for the role they are playing through free blood pressure monitoring, on-the-spot lifestyle advice and increasing public awareness of the risk of hypertension. There are plenty of lessons to be learned from overseas, too. Canada in particular has highlighted the financial, as well as public health, benefits of pharmacist-led interventions in hypertension.
Community pharmacy services
In 2014, PHE developed an action plan, in partnership with government, the NHS, volunteer groups and academia, to improve the prevention, early detection and management of high blood pressure in England. In 2017, it produced a report[2]
in collaboration with Pharmacy Voice to highlight the public health role of community pharmacists and the impact they can have in improving the detection and management of hypertension.
Blood pressure is a significant factor [in stroke] and people don’t always know that their blood pressure is raised
One example in the report is the collaboration between Well Pharmacy, the third largest pharmacy chain in the UK, and the Stroke Association, the UK’s leading stroke charity, which started at the beginning of 2017. “Blood pressure is a significant factor [in stroke] and people don’t always know that their blood pressure is raised,” explains Jane Devenish, an NHS Services and Standards pharmacist at Well Pharmacy. “We thought that by working with the Stroke Association we could make a big impact on preventing people from having strokes.”
Devenish believes strongly that community pharmacists are well placed to be able to identify hypertension at the earliest opportunity and help patients make the necessary lifestyle changes to reduce their risk of serious cardiovascular events.
“[Community pharmacists] see a variety of people at all stages of their life: when they are well, when they’re concerned about their health and when they have long-term conditions,” she explains. “If you can pick up that someone’s got elevated blood pressure before they start to have symptoms, they have the opportunity to do something about it at that stage — it’s about giving people the right information at the right time.” As part of the initiative, Well Pharmacy offers free blood pressure checks, which include making lifestyle recommendations that are realistic for individuals and their circumstances.

Source: Courtesy of Jane Devenish
Jane Devenish, an NHS Services and Standards pharmacist at Well Pharmacy, believes that community pharmacists are well placed to be able to identify hypertension at the earliest opportunity and help patients make the necessary lifestyle changes to reduce their risk of serious cardiovascular events.
Devenish says that, with the rise of fitness trackers, she is seeing a definite increase in patients wanting to take charge of their own health. “People want to monitor their own blood pressures, [but] one of the benefits of coming into the pharmacy is that they’re given the information and are then helped to make a change,” she says.
Pharmacist-led community clinics
Improving patient access to services is one of the key drivers of the pharmacist-led, community-based hypertension clinics that have been running across Lambeth and Southwark clinical commissioning groups since 2013.
“The beauty of this service is that it’s proactive,” says Vicki Collings, senior cardiovascular pharmacist at Guy’s and St Thomas’ NHS Foundation Trust. “A lot of primary care services are inherently reactive because GPs aren’t necessarily searching for these patients — if they don’t come back for their annual check-ups, then they just get lost.”
A lot of primary care services are inherently reactive because GPs aren’t necessarily searching for these patients — if they don’t come back for their annual check-ups, then they just get lost
The service was the result of a successful pilot study targeting practices with poor hypertension control and has two main arms: four hypertension clinics across Lambeth and Southwark and virtual clinics run in GP practices[5]
. Both rely on the expertise of specialist cardiovascular disease (CVD) pharmacists, such as Collings and fellow pharmacist Chris Meddings.

Source: Julia Robinson / The Pharmaceutical Journal
Vicki Collings and Chris Meddings, specialist cardiovascular disease pharmacists at Guy’s and St Thomas’ NHS Foundation Trust, lend their expertise to community-based hypertension clinics across Lambeth and Southwark clinical commissioning groups, which have been running since 2013
Unlike GPs, the pharmacists dedicate 30 minutes to each patient
The hypertension clinics are run on specific days of the week at either end of the London boroughs in Streatham, Brixton, Dulwich and Bermondsey. Patients are referred by their GP for specific reasons, such as drug intolerances or non-adherence. Unlike GPs, the pharmacists dedicate 30 minutes to each patient, during which they take full medication histories and record lifestyle choices. They also take the patient’s blood pressure at least three times in both arms to ensure the most accurate reading possible. Following the initial consultation, a treatment plan is drawn up with the patient, tailored to their lifestyle, and they can return for follow-up appointments for as long as they need to.
“[The treatment plan] really depends on what you find out in that first meeting,” says Meddings. “It could be that there’s another, underlying issue. They’re often complex patients with multiple morbidities — such as poorly controlled diabetes, poorly controlled lipids, angina or respiratory disease — so it’s about trying to look at the patient holistically.” Or it could just be as simple as looking at it from a different point of view, he explains. “They may have high blood pressure when they come in but they’re fine once they go home.”
The clinics were evaluated between October 2014 and June 2015, and during this period a total of 291 interventions were made. For patients who attended at least two appointments (n=34) there was a mean decrease in blood pressure of 16/3mmHg (P <0.01) with average improvements from 154/82mmHg (±14/15) at initial visit to 139/79mmHg (±16/16) at discharge. The study concluded that community pharmacist-led clinics had a demonstrably positive impact on blood pressure results and, by focusing on patient and provider-related factors, such as lifestyle modification and medicines optimisation respectively, they increased the number of patients who were able to reach their blood pressure targets.
The success of the project means that the scheme is now being rolled out in other areas, such as Bexley.
Virtual clinics
Collings and Meddings are also involved in virtual hypertension clinics, so named because patients are not present. These include the whole practice team, from healthcare assistants to GPs. Patients with ‘high’ blood pressure — systolic over 160mmHg and diastolic over 100mmHg — are identified through a computer-based audit, and as many as 100 or as few as ten can be discussed during a two-hour clinic.
“The best [clinics] are when we get as many people as possible,” says Meddings. “We’re talking about a variety of patients and not every GP looks after every patient; we can discuss them all at once and someone can say, ‘I know that patient well, I can present it’.”
It’s about trying to educate everyone, he adds.
After the initial clinic, the team draws up a treatment plan for each patient and the GPs manage the follow-up. The pharmacy team will run another audit after six months to see if the clinic has made a difference in patient outcomes.
Data on the most common interventions recommended within clinics throughout 2015 and 2016 reveal that initiation of new medication was suggested for 32.7% of people, titration of current medication was recommended for 21.3%, lifestyle advice was recommended for 9.7% and referral to the community hypertension clinic in Lambeth and Southwark was recommended for 4%.
“Nine and a half times out of ten people love the [virtual] clinics and find it a very valuable service,” says Collings. “It has now been rolled out for lots of other long-term conditions, including respiratory: asthma; chronic obstructive pulmonary disorder; and heart failure.
What’s unique is that we’re secondary care pharmacists but actually we’re doing a lot in primary care to help prevent admissions and save specialists time in hospital and GP time
“What’s unique is that we’re secondary care pharmacists but actually we’re doing a lot in primary care to help prevent admissions and save specialists time in hospital and GP time. That’s the aim.”
GP practice clinics
Primary care pharmacists can also have a positive impact on GP time. In her role as managing partner and pharmacist at Brigstock and South Norwood Partnership in Surrey, Dipti Gandhi’s work revolves entirely around patients who require specialist help in managing high blood pressure. “If they’re difficult to control, they’re referred on to me,” she explains. However, one of the problems she sees time and again is a lack of adherence. “I see the patients and straight away establish whether they’re taking their medicines. Many haven’t got resistant hypertension — they’re just not taking their tablets.”
Source: Courtesy of Dipti Gandhi
Dipti Gandhi, managing partner and pharmacist at Brigstock and South Norwood Partnership in Surrey, looks after patients who require specialist help in managing high blood pressure
Gandhi works closely with the nurses, doctors and healthcare assistants in the practice, particularly the nurse prescriber who has a special interest in diabetes. “Both of us are quite autonomous in our practice and we work really well together. If it’s a blood pressure problem she’ll come to me and vice versa. Long-term condition management doesn’t really go near a GP.”
It was very insular at first, [patients] didn’t catch on that you could be a pharmacist
Gandhi’s role has evolved over the past 14 years, requiring her to build up trust among the practice’s five GPs. But now, she says, seeing a pharmacist is treated no differently from seeing a GP or any other healthcare professional. “It was very insular at first, [patients] didn’t catch on that you could be a pharmacist; they thought you were a nurse or a doctor. ‘Oh you’re in the pharmacy next door?’ ‘No,’ I’d say, ‘I’m based here’.”
Untapped resource
But those in the pharmacy next door remain an untapped resource, according to Warren. She believes that more could be done to help manage patients with hypertension and give them ownership of their health, for example, by encouraging more home blood pressure monitoring and getting patients to fill in their own blood pressure diaries.
“It’s about having something in community pharmacy that almost triages patients before they go to secondary care. Pharmacists have a lot to offer in terms of, do the patients take their medications? If not, why not?”
According to Pharmacy Voice’s report, community pharmacy in the UK has much to learn from best practice in Canada, where 65% of adults with high blood pressure are both diagnosed and managed to recommended levels, compared with just 35% in England. This has been attributed to Canada’s National Strategy for High Blood Pressure Prevention and Control, developed in 2000, as well as its focus on disseminating hypertension recommendations and building a leadership cohort across a broad group of primary care staff including GPs, nurses and pharmacists.
According to Ross Tsuyuki, professor of medicine (cardiology) at the University of Alberta and co-author of a study into the impact of community pharmacist care for Canadians with hypertension[6]
, it can also be attributed to the efficient guidelines process run through Hypertension Canada.

Source: Courtesy of Ross Tsuyuki
Ross Tsuyuki, professor of medicine (cardiology) at the University of Alberta, co-authored a study into the impact of community pharmacist care for Canadians with hypertension
The study showed that having community pharmacists conduct formal consultations with patients resulted in a rare combination of positive outcomes, including projected cost savings of more than CA$15.7bn (£9.2bn) compared with usual care over 30 years.
“Usually when you do an economic evaluation of an intervention, it either provides more health benefits but costs more, or it is cost saving but the health benefits are not as great,” says Karissa Johnston, principal and scientific director at Vancouver-based consultancy Broadstreet Health Economics & Outcomes Research and another author of the study. “What we saw with the pharmacists’ intervention in hypertension is that it saved money and provided a substantial amount of health benefits, including [preventing] cardiovascular events — an expensive issue for the health system to treat.”

Source: Courtesy of Karissa Johnston
Karissa Johnston, principal and scientific director at Vancouver-based consultancy Broadstreet Health Economics & Outcomes Research, says pharmacists’ intervention in hypertension saved money and provided a substantial amount of health benefits
Carlo Marra, lead author of the study and dean of the school of pharmacy at the University of Otago in New Zealand, adds that although community pharmacists are set up to tackle hypertension, in Canada the main issue is financial. “The infrastructure is already provided to do this — we have a lot of well-trained pharmacists in community settings ready to take this on, [but only] if a funding model facilitated it.”
The PHE and Pharmacy Voice report highlights that pharmacists can only make a contribution if hypertension initiatives are integrated with other public health and primary care services, as well as rigorously quality assured and evaluated. Only then can these pockets of good work spread out across the UK.
Rates of blood pressure control vary among GP practices but positive shifts are occurring, with other healthcare professionals having greater involvement in practice hypertension care. At present, pharmacists are involved in hypertension care in only 5% of practices[7]
; however, with NHS England’s pledge to fund more pharmacists in GP practices and an increasing interest in pharmacist-led hypertension clinics, this may be set to change.
“This is all upstream primary prevention,” says Collings. “If we get this right now, in five, ten years’ time, we will reduce the amount of heart attacks and strokes, which will impact secondary care services and also social care in the community. It will have a much wider benefit for everyone.”
References
[1] High blood pressure. British Heart Foundation. Available at: https://www.bhf.org.uk/heart-health/risk-factors/high-blood-pressure (accessed June 2017)
[2] Public Health England, Pharmacy Voice. Tackling high blood Pressure through community pharmacy. February 2017. Available at: http://pharmacyvoice.com/wp-content/uploads/2017/02/Blood-Pressure-Report.pdf (accessed June 2017)
[3] Quality statement 4: Blood pressure targets. Hypertension in adults. National Institute for Health and Care Excellence, March 2013, updated September 2015. Available at: https://www.nice.org.uk/guidance/qs28/chapter/quality-statement-4-blood-pressure-targets (accessed June 2017)
[4] Warren A. Evaluation of pharmacy prescriber clinic for hypertension. Brighton and Sussex Centre for Medicines Optimisation. November 2015. Available at: https://www.brighton.ac.uk/bscmo/research-projects/evaluation-of-pharmacist-prescriber-clinic-for-hypertension.aspx (accessed June 2017)
[5] Williams H. Hypertension: improving blood pressure management in primary care. National Institute for Health and Care Excellence, January 2017. Available at: https://www.nice.org.uk/sharedlearning/hypertension-improving-blood-pressure-management-in-primary-care (accessed June 2017)
[6] Marra C, Johnston K, Santschi V et al. Cost-effectiveness of pharmacist care for managing hypertension in Canada. Can Pharm J 2017;150:184–197. doi: 10.1177/1715163517701109
[7] Mejzner N, Clark CE, Campbell JL et al. Trends in the diagnosis and management of hypertension: repeated primary care survey in South West England. Br J Gen Pract 2017. doi: 10.3399/bjgp17X69046


