“I would need to spend my day off completing training in a surgery, but my role is so exhausting I need the day off to recover. Also, the opportunity to use the [independent prescribing] qualification is almost nothing.”
This comment from a community pharmacist based in England, responding to The Pharmaceutical Journal’s 2024 salary and job satisfaction survey, sums up some of the frustrations about independent prescribing (IP) that are felt within the existing workforce.
From 2026, all newly qualified pharmacists will have an IP qualification — a crucial turning point in the drive for community pharmacists to expand their scope of practice and be commissioned to provide a wider range of NHS services.
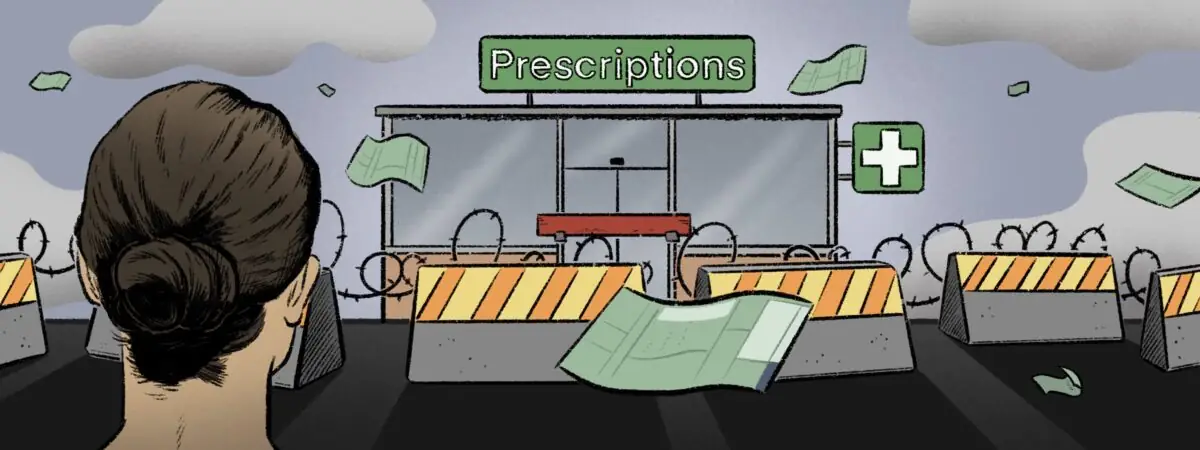
However, there are significant barriers for experienced community pharmacists in becoming an independent prescriber, such as a lack of time to do the course, minimal protected learning time and difficulty securing supervision. And, for those who have managed to undertake a prescribing qualification regardless, it is rare they get to use it.
Results from the survey of 1,372 UK pharmacists across all sectors, conducted between 15 April 2024 and 30 April 2024, show that only one in six community pharmacists (14% of 322 respondents) are currently prescribers, compared with 53% of 417 hospital pharmacists and 71% of 213 pharmacists in general practice.
Almost a third of community pharmacist respondents (30% of 271) said they have no interest in becoming an independent prescriber when asked to list the barriers preventing them from gaining the qualification (see Figure 1). Other barriers included having no access to a designated prescribing practitioner (DPP) (52%) and having no time to do the course (48%).
Barriers to qualifying as an independent prescriber appear to be higher for community pharmacists, with 21% of 276 community pharmacists currently training to be an independent prescriber or having plans to do so within the next year, compared with 30% of 195 hospital pharmacists and 77% of 60 pharmacists working in general practice.
Unlike their counterparts in general practice and hospital pharmacy, there is a lack of incentive for community pharmacists to gain the IP qualification for its usefulness, with more than a quarter of community pharmacist prescribers (26% of 46) saying they had never actually prescribed and 9% saying they prescribe less than once a year (see Figure 2).
Community pharmacist respondents said that barriers to prescribing included a lack of opportunity (70%) and lack of funding (37%) required to undertake the role (see Figure 3).
Lack of opportunity
Having all pharmacists ready to prescribe from the point of registration “will only be transformational if there are widespread opportunities for community pharmacists to apply prescribing skills within properly funded NHS services,” says Gareth Jones, director of external affairs for the National Pharmacy Association (NPA).
If such a service is implemented correctly, he says there is potential for a “step change” in the way people experience pharmaceutical care, whether for long-term conditions or acute episodes.
I would love to use independent prescribing more
Ifesinachi Anyamene, superintendent pharmacist, Fieldway Pharmacy, Croydon, Greater London
Ifesinachi Anyamene, superintendent pharmacist at Fieldway Pharmacy in Croydon, Greater London, has been a prescriber for about four years but rarely has the opportunity to use her skills. “I would love to use it more. My area of competence was hypertension and we do the blood pressure checking service but I can only advise.”
Under the ‘Community pharmacy blood pressure check service’, pharmacies are remunerated for referrals to other parts of the NHS if a patient is found to have high blood pressure. Anyamene’s locum is in the same position after specialising in dermatology.
Sam Chidlow, policy and programmes manager at the Company Chemists’ Association (CCA), agrees that the biggest barrier for everyone — whether they are already a prescriber, are thinking about becoming one or will be part of the new cohort coming through in 2026 — is the lack of NHS commissioned services.
We have a lot of independent prescribers working for us that can only ever use their skills in private services
Sam Chidlow, policy and programmes manager, Company Chemists’ Association
“We have a lot of independent prescribers working for us that can only ever use their skills in private services,” says Chidlow. “Data from [NHS England’s 2022] ‘Community pharmacy workforce survey (CPWS)’ show that only about 17% of independent prescribers use their qualification, despite the fact that there are 1,576 independent prescribers across the community pharmacy sector1.”
The Labour Party manifesto included a pledge to create a ‘Community pharmacist prescribing service’, “granting more pharmacists independent prescribing rights where appropriate”2. The NPA has called for this policy to be pursued “vigorously”.
Groundwork for this is already being laid through NHS England’s ‘Independent prescribing pathfinder programme’ for community pharmacies, which was first announced in August 2022, with the aim of informing future commissioning and tackling logistics. But this is proving slow to get going. Speaking at the Clinical Pharmacy Congress in May 2024, Wasim Baqir, senior pharmacist at NHS England’s pharmacy integration fund, said that of 210 sites planned, only 14 had got off the ground, with another 180 ready for roll out.
In August 2024, NHS Engand announced that the electronic prescribing system needed for the service was ready for roll out to all sites, but noted that it was still “working with them [integrated care boards] regarding the next steps”.
In comparison, Community Pharmacy Wales says 181 of 686 pharmacies are providing the ‘Pharmacy independent prescribing service’, with more than 92,000 consultations completed in the year up to the end of April 2024. And, in Scotland, there are currently 354 out of 1,243 community pharmacies providing the independent prescribing Pharmacy First Plus service. Community Pharmacy Scotland’s aim is to have one independent prescriber in every pharmacy to provide 100% coverage by 2030.
Our focus is getting pharmacists through these qualifications so that all communities have access to an independent prescriber
Sarah Scott, policy and public relations pharmacist, Community Pharmacy Scotland
“Our hope is, in time, that new services will grow,” says Sarah Scott, policy and public relations pharmacist at Community Pharmacy Scotland. “Currently, our focus is getting pharmacists through these qualifications so that all communities have access to an independent prescriber for these acute clinical conditions.”
CCA data — submitted to the CPWS 2023 — suggest that one in five pharmacies in England have a prescriber present at some point during the week. “That is a huge amount of clinical capacity,” says Chidlow.
The lack of opportunity to prescribe provides a disincentive for prescribers to qualify but also adds to issues with retaining staff who want to use those skills, he adds.
“It certainly doesn’t help in making community an attractive place to work if a significant part of your course and your foundation year has been dedicated to prescribing and then you come out and you can’t use it.”
No access to supervision
Another obstacle in community pharmacy is the availability of designated prescribing practitioners (DPPs) qualified to supervise those in training — either foundation pharmacists or experienced staff doing an independent prescribing course.
“With the recruitment for the 2025/2026 foundation year, because there are very few pharmacists working in prescribing roles in the community, we cannot find DPPs for our placements,” says Chidlow.
“We’re having to rely on GPs and hospital pharmacists.”
Community pharmacy employers would like a matching-type service at regional or integrated care board (ICB) level, he adds, as well as adequate funding to reimburse for the costs.
However, the lack of DPPs may be a temporary problem and securing them “will become easier as cross-sector rotational placements become mandatory from 2026/2027”, he says.
In Scotland, there is a ‘teach and treat’ model, where experienced and well-established pharmacist prescribers can offer support to trainees coming through. However, this is limited at the moment because there is only a small group of prescribers offering supervision, who could easily be overwhelmed by the demand.
Anyamene says she feels lucky that she found a GP who was willing to be her DPP but says it meant travelling ten miles once a week for months to be supervised. Knowing this is a barrier for others in her team, she is now training to become a DPP, which she says will also be useful for the foundation pharmacists they take on.
“I want to help my staff. You can see this is the future, especially with what we have done with Pharmacy First. Patients are already coming to us, knowing they can get a consultation.”
Capacity will be a short-term problem as more people come through
Brendon Jiang, vice-chair of the Royal Pharmaceutical Society’s English Pharmacy Board
Brendon Jiang, vice-chair of the Royal Pharmaceutical Society (RPS)’s English Pharmacy Board, highlights the RPS mentoring programme, through which people can find a DPP, but agrees that “there is a capacity issue” with those who can offer that service.
“This will be a short-term problem as more people come through,” he says.
Lack of interest
However, as evidenced by The Pharmaceutical Journal’s survey results, not everyone in the existing workforce wants to become an independent prescriber. Some feel that they are too close to retirement to return to academic study and others have family commitments that preclude the time investment needed.
Khalid Khan, head of training and professional standards at Imaan Healthcare, a chain of pharmacies across north west England and Yorkshire, says the company made a strategic decision to support its pharmacists to become independent prescribers, with the aim of having half of its pharmacists qualified across its 70 branches. However, he acknowledges that this target may not be achieved because not everyone is keen.
It does seem like it has been the tail wagging the dog in England
Khalid Khan, head of training and professional standards, Imaan Healthcare
“We wanted to try and engage those that were not independent prescribers because we need to future proof our business. The IP course itself is now funded but we put a programme together with a number of paid study days off,” explains Khan.
But, he adds, for those who qualified 10 to 20 years ago, it has been a bit of a cultural shift to go back to studying. The time commitment can be a burden, especially for those with young families, he adds. “Some of those who were relatively newly qualified have found it a bit easier.”
Imaan’s branch in Blackpool, Lancashire, was chosen as one of the pathfinder sites but it is not yet up and running. “It keeps getting pushed back even though [the staff are] raring to go. The IT seems to be the sticking point.”
He too believes there is a lot of learning that could be taken from Scotland and Wales. “It does seem like it has been the tail wagging the dog [in England]. We have decided we’re going to have prescribers and now we’re looking at what we’re going to do with them.”
Ongoing professional development
Ian Maidment, professor in clinical pharmacy at Aston University, points out that it has not yet been fully articulated how pharmacist prescribing will work in practice, despite the clear policy drive.
There are all sorts of complexities to sort out around how it will work on a large scale, for example, in separating dispensing and prescribing, and what sort of supervision is needed, he explains.
Just making every community pharmacist an independent prescriber without a clear implementation pathway may not solve much
Ian Maidment, professor in clinical pharmacy, Aston University
“Just making every community pharmacist an independent prescriber without a clear implementation pathway may not solve much. For example, if you’re an independent prescriber, then are you an independent prescriber for everything or just an independent prescriber for one defined area?”
Maidment has other practical concerns around scope, oversight and balancing commercial and clinical pressures. He has been funded by the National Institute for Health Research to do a detailed literature review of what does and does not work for IP in community pharmacy and what has been written about it in other settings. He hopes to produce recommendations on how best to develop services in the future by the end of 2025.
But this work should have all been carried out before ploughing ahead, he argues.
Ellen Schafheutle, professor of pharmacy policy and practice at the University of Manchester, will be evaluating the findings of the pathfinder programme in England. In all, 13 different models are being tested through ICB-commissioned projects, including minor ailments, hypertension, respiratory and dermatology.
There will need to be a structure for ongoing professional development within community pharmacy and there is learning from how this has been applied in general practice, she explains3. “No one expects the day one qualified doctor or nurse to be the finished piece.” There is a bit more of that culture in hospital pharmacy, she points out, but that relates to a clear career trajectory towards advanced practice.
“There is nothing like that in community pharmacy. There needs to be an understanding and support to help people grow into that role.”
Just ‘doing it’ doesn’t necessarily mean you are going to become more competent
William Swain, prescribing integration project manager, Lewisham and Greenwich NHS Trust
It is likely the only way you can develop a more competent prescriber is through effective supervision, says William Swain, prescribing integration project manager at Lewisham and Greenwich NHS Trust and lecturer at University College London.
“Just ‘doing it’ doesn’t necessarily mean you are going to become more competent,” he explains. “Prescribers need role modelling and regular feedback, working closely with someone more experienced. At the moment we are so far from that.”
Swain suggests that there should be some sort of decision support in place going forward, which could be a consultant, GP or senior colleague. Careful consideration is needed about the supervision model and how to make community pharmacists part of a multidisciplinary team to help support and build their skills.
“Just because you are allowed to do something from a statutory legal standpoint doesn’t mean you should do it straight away,” he adds.
The IP service that will develop in community pharmacy in England will likely be a “gateway”, with onward referral where needed, rather than prescribing across the board, says Schafheutle.
“How exactly that is going to run and what works will have to be worked through and the pathfinder programme is one way of finding that out. There are many important but moving parts.” Early and continuous engagement between those developing the service and employers will be vital, she adds.
Emjad Dubaissi is pharmacy director at Medihub Pharmacy, with two branches in Swansea, south Wales. He is also a partner in a GP surgery and as such has been one of those leading the way on prescribing in Wales, “seeing 10 to 15 patients a day through the prescribing service”. He says it is clear the future of community pharmacy lies in more services, including cancer screening, cholesterol testing, weight loss and dermatology.
But Dubaissi has seen trainees put off community pharmacy because they have developed all these clinical skills that are not being used. This is now starting to change as the sector expands, he says, having attracted two pharmacists back into the community — one from hospital and one from general practice — because of the variety of work they were able to offer. “I think we will see more of that.”
The newly qualified pharmacists coming through the system have excellent clinical skills but need to build up their confidence on communication and consultation skills, he says. “And risk management as well. It’s the application of those clinical skills and that is going to be interesting. Better collaboration with the wider primary care system could be helpful.”
Khan points out that sometimes the sector can get in its own way trying to “dot all the i’s and cross the t’s”, but he believes that it will sort itself out.
Wales and Scotland show that it is possible. “Community pharmacy is an untapped resource. I believe we can get there, none of this is insurmountable once the services are in place.”
- 1.Association of Independent Multiple Pharmacies, National Pharmacy Association, Company Chemists’ Association. Building an understanding of the community pharmacy workforce – reflections on the national workforce survey. Community Pharmacy Workforce Development Group. Published September 1, 2023. Accessed August 6, 2024. https://communitypharmacyworkforce.com/wp-content/uploads/2023/09/cpwdg-building-an-understanding-of-the-community-pharmacy-workforce-reflections-on-the-national-workforce-survey-.pdf
- 2.Change. Build an NHS fit for the future. Labour. Published June 13, 2024. Accessed August 6, 2024. https://labour.org.uk/change/build-an-nhs-fit-for-the-future/
- 3.Styles M, Middleton H, Schafheutle E, Shaw M. Educational supervision to support pharmacy professionals’ learning and practice of advanced roles. Int J Clin Pharm. 2022;44(3):781-786. doi:10.1007/s11096-022-01421-8