For a moment, in October 2023, virtual wards — where patients who would usually be treated in hospital for an acute condition receive care at home (see Box) — became a trending topic.
NHS England announced on 12 October 2023 that it had met its target of delivering 10,000 virtual ward ‘beds’ across the country by the end of September 2023, and subsequently asked integrated care services to expand their offering to include more patients with heart failure on virtual wards, which have historically housed patients with frailty and acute respiratory infections[1,2]. Acknowledging this rapid growth of virtual wards, the Royal Pharmaceutical Society (RPS) launched interim professional standards for ‘hospital at home’ pharmacy services on 17 October 2023[3].
However, the Care Quality Commission (CQC) issued a warning on 20 October 2023 in its annual ‘State of care’ report that “policy, practice, and governance of medicines [is] being overlooked” in virtual wards because pharmacy teams are often not involved in setting them up from the outset and there is not always budget allocated for pharmacy staffing[4].
NHS England’s longer-term ambition, set out in its ‘Delivery plan for recovering urgent and emergency care services’, published in January 2023, is to further increase capacity in virtual wards to more than 50,000 admissions per month[5]. Hospital at home and virtual ward services have also been established in Scotland, where the Scottish government has announced further investment to expand support in 2023/2024, and in Wales and Northern Ireland.
As use of virtual wards expands, it is becoming increasingly apparent that the virtual ward pharmacy team has an essential role in ensuring safe use of medicines in this non-traditional acute care setting.
Box: What are virtual wards?
The concept of virtual wards has been provided in some local healthcare systems in the UK for many years — in some places, for decades. ‘Virtual ward’ is a term that covers various types of service, including the traditional face-to-face ‘hospital at home’ model, but the common theme is that it is acute care for a specific group of patients who would otherwise be in hospital. Patients are managed by a clearly defined and consistent multidisciplinary team that works together, through the use of daily ‘ward routines’.
Virtual wards have been set up in different ways throughout the country. Depending on local protocols, consultants, GPs, paramedics, community matrons and emergency call handlers are among those who may refer patients to a virtual ward.
Patients eligible for treatment on virtual wards may have been admitted to prevent them from being admitted to hospital or to enable them to be discharged from hospital sooner. Patients with frailty may require repeated home visits, whereas others — including on virtual respiratory wards — may be monitored remotely by clinical staff using technology, such as apps, wearables and other medical devices.
According to NHS England, evidence from long-standing hospital at home programmes suggests several benefits of this approach, including patients being five times less likely to acquire an infection on a virtual ward compared with admission to hospital and eight times less likely to experience functional decline[6].
In practice
When a ‘home ward’ service was first planned by Leeds Teaching Hospital NHS Trust in 2019 — carefully named because patients did not understand the term ‘virtual ward’ at the time — pharmacy was not considered, explains Heather Smith, now a consultant pharmacist in older people at Leeds Health and Care Partnership. However, then at the hospital trust, she quickly recognised the need for a proactive virtual ward pharmacy service, so set up a team led by advanced pharmacist Amy Vigar, comprising two other pharmacists and two pharmacy technicians.
Most patients on the home ward are aged over 65 years with frailty and are there to prevent an acute hospital admission. Each day, the pharmacy team carries out structured medication reviews, remotely or by home visit, followed by a multidisciplinary team (MDT) meeting with the consultant and community matrons.
“We work on a fairly autonomous basis, so if we identify a medicine that could be causing a fall, we can remove that medication from the house at that point and then liaise with the consultant in the MDT,” explains Vigar.
The pharmacy team also advises on potential interactions, adverse effects that might be contributing to the acute illness and the best medicines to prescribe, while liaising with community pharmacy, the patients and their carers about the best way to deliver the medicines to them. Around the country, each virtual ward does things slightly differently, explains Vigar, who is part of a national network of 50 virtual ward pharmacists.
Without a pharmacy team in place and clear governance structures, Smith adds that there would be significant potential for medication errors.
“There is also a lot of deprescribing in our role,” adds Vigar. “We’re focused on the acute illness, but you do pick up chronic issues, so it’s about referring, which could be to the hospital, primary care network or GP pharmacist, and making sure [patients] are safety netted,” she explains.
I don’t know how a service could run without a pharmacist
Graham Sutton, a consultant in elderly medicine and lead clinician, Leeds virtual ward team
Graham Sutton, a consultant in elderly medicine and lead clinician on the Leeds virtual ward team, says pharmacist input has been crucial to the success of the service, particularly around medication reviews, day-to-day advice and prescribing for others who are not yet independent prescribers. “I don’t know how a service could run without a pharmacist,” he notes.
Professional standards
Through its interim standards, the RPS has identified areas where pharmacist teams should have input into virtual wards, says Ravijyot Saggu, medicines optimisation lead at Central London Community Healthcare NHS Trust.
Saggu was involved in drawing up the standards, which, she says, set out what “good” looks like, enabling services to audit what they are doing and identify where there may be a skills gap.
There’s a lot of activity; this is an emerging role and there’s really a place for pharmacist teams to make a difference
Ravijyot Saggu, medicines optimisation lead, Central London Community Healthcare NHS Trust
The RPS is one of many organisations establishing standards in this area. The National Institute for Health and Care Excellence has also published a suite of guidance and resources to help manage acute respiratory infection patients safely in their homes.
The CQC is working on its own standards, says Saggu. “There’s a lot of activity; this is an emerging role and there’s really a place for pharmacist teams to make a difference.”
Saggu believes the most important role for pharmacy in virtual wards is medicines reconciliation because, whenever someone’s care is transferred to a different setting, there is a risk of errors.
“Pharmacists are involved in the MDTs, taking part in regular meetings, doing structured medication reviews, and they might also have a technician with them,” she says. The lead clinician is often a consultant but it can also be a GP, depending on how the virtual ward has been set up. “There is a lot to coordinate and there are issues around governance and information flow.”
Technology
According to the RPS standards, digital technology and data sharing have a crucial role to play in optimising care for patients.
Beth Harries, principal clinical pharmacist for Sussex Virtual Wards, was involved at the outset of the plans for 600 virtual ward beds in the region, which have been in place since December 2022. “It meant we could really think through the practical aspects, like where do you get the medicines from and who prescribes. We could design it from scratch.”
In Sussex, patients in virtual ward beds are under the care of the hospital consultant team, supported by pharmacist independent prescribers. The Sussex team opted for community pharmacies to supply and deliver medicines for virtual ward patients because it covers a large geographical area. As a result of the large area, about 60% of virtual ward patients also have remote monitoring, meaning the virtual ward team can view observations, such as a patient’s pulse or temperature, on a web-based dashboard. A secure text messaging platform is used to ask patients if they have received medicines.
However, use of technology on the home ward in Leeds is still being considered.
“We don’t know what that will look like. It might be an Apple Watch or a patch that you wear, but we’re not there yet,” says Vigar. Mobile electrocardiogram and chest X-rays are also options.
Smith adds that Leeds already has a virtual respiratory ward and there is a workstream looking at how remote monitoring technology can be better used there. In the future, there may be similar set ups for heart failure and post-surgery discharge.
The CQC’s annual report notes that a lack of integration and compatibility of digital systems in secondary, primary and community care can be problematic when transferring information.
But one advantage for the virtual ward pharmacy team in Leeds is its access to all secondary and primary care IT systems across the city, says Vigar. “That’s why we’re relied upon for a lot of this communication because we can see all of it,” she says.
Skills and training
Vigar also notes that pharmacists must have good clinical and communication skills to work on a virtual ward, but also be practical and pragmatic. “You do also have to be working towards advance-level practice, it’s definitely high-level use of clinical skills.”
Saggu adds that an understanding of long-term conditions, and probably secondary care experience, as well as good consultation skills are needed. “You have got to be able to challenge decisions because you’re reviewing patients and thinking about polypharmacy and deprescribing but also have an understanding of the wider NHS landscape.”
I now do clinical examinations to bring back to the MDT or start the initial care plan
Chris Jones, advanced clinical practitioner and pharmacist, Bradford Virtual Ward
Some pharmacists are going a step further and undertaking training to gain more practical skills. Chris Jones began working on what was then a hospital at home service for frail and older patients in Bradford in 2016, after the team wanted more help with medicines management. At first he conducted medicines use reviews but, over time, he became more hands-on than most pharmacists generally would, he says.
“It started to make sense for me to do basic observations, taking blood pressure, keeping an eye on patients as you would on a hospital ward.” He went on to train in phlebotomy so he could take blood before doing an advanced clinical practitioner course. “I now do clinical examinations to bring back to the MDT or start the initial care plan. I’ve been slowly building my skills over time.”
Jones is one of two full-time pharmacists on the team. There is also a separate team running a virtual respiratory ward that makes use of more remote monitoring. “The trust as a whole is now starting new virtual wards in various areas,” explains Jones.
Similar practical skills are also being actively developed within the pharmacy team at Oxford University Hospitals NHS Foundation Trust. Sophie McGlen, a highly advanced pharmacist, works within a team of five pharmacists and a technician across the virtual ward programme, mostly working remotely but doing home visits where needed.
Every person that comes through our service has some need for a pharmacist
Sophie McGlen, highly advanced pharmacist, Oxford University Hospitals NHS Foundation Trust
The team is being trained in phlebotomy, point-of-care ultrasound and canulation, which will mean that only one person needs to visit the patient. “There’s a lot more blurring of roles within the virtual space,” says McGlen.
“If you’re treating someone at home, the most likely intervention you will make is to stop or start a medicine because you’re not doing surgery or putting in a drain. Every person that comes through our service has some need for a pharmacist.”
Workforce
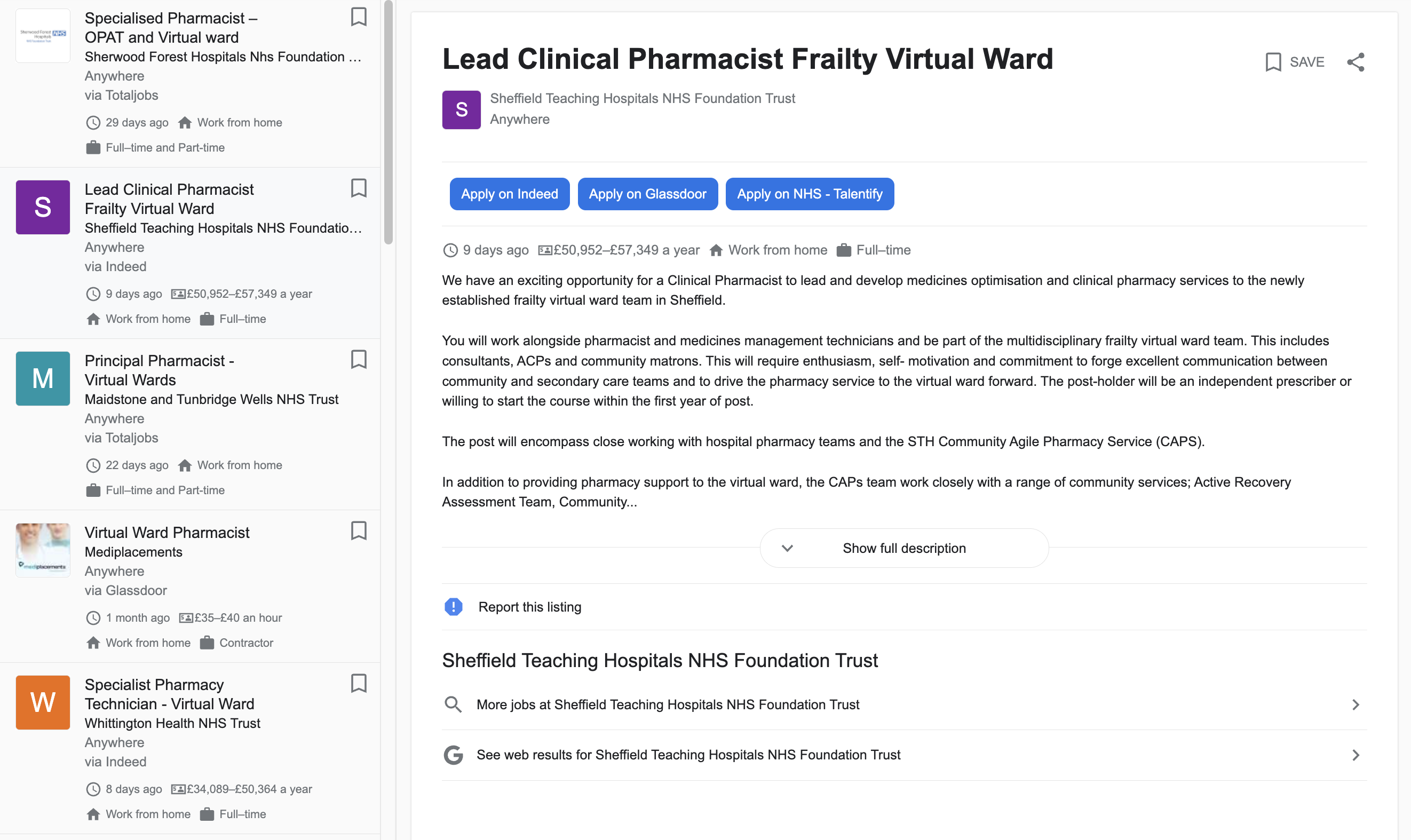
Despite the high level of skills required, McGlen says that when job advertisements for virtual ward pharmacists first started coming out, they were banded as quite low on the NHS Agenda for Change pay scale (see Figure).
“Things like the RPS professional standards highlight that this isn’t [a role] for a newly qualified pharmacist. There’s an enormous amount of problem solving,” she says.
“It is slightly uncharted territory so there’s a lot of opportunity to develop as a team, and professionally, but the pathway on what that looks like is not yet clear.”
As virtual ward teams grow, Harries predicts there will be more interest in hiring pharmacist prescribers. “Prescribing is one of the real barriers [to providing care on virtual wards] and pharmacists are really well placed to fill that gap,” she says.
But it will take time for this new breed of virtual ward pharmacists to become established in a consistent way across the country. “I have heard people say our pharmacy team doesn’t do very much and I’m thinking, well that’s either because they’re not enabled to do much or there’s not enough of them,” says Harries.
More needs to be done at the commissioning level to ensure that virtual ward services are investing in developing their own pharmacy teams
Desmond Gourley, pharmacy lead for hospital at home, Southern Health and Social Care Trust
Desmond Gourley, pharmacy lead for hospital at home at the Southern Health and Social Care Trust in Northern Ireland, agrees that there is significant variation in pharmacy staffing levels in virtual ward services across the UK. “Investment in pharmacy staffing must be a vital component in the successful delivery of virtual wards or hospital at home services.
“More needs to be done at the commissioning level to ensure that virtual ward services are investing in developing their own pharmacy teams.”
Gourley says that hospital at home guidance in Northern Ireland recommends that, for an average caseload of 25 patients (2,000 patients per annum), there should be 1 Agenda for Change band 8a pharmacist, 7.6 band 7 pharmacists and 2 band 5 pharmacy technicians.
“Those services that do not invest in pharmacists and pharmacy technicians cannot meet the challenges around medicines governance essential for effective virtual ward or hospital at home services,” warns Gourley.
- 1NHS delivers 10,000 virtual ward beds target with hundreds of thousands of patients treated at home. NHS England. 2023. https://www.england.nhs.uk/2023/10/nhs-delivers-10000-virtual-ward-beds-target-with-hundreds-of-thousands-of-patients-treated-at-home/ (accessed 14 November 2023)
- 2Guidance note: virtual ward care for people with heart failure. NHS England. 2023. https://www.england.nhs.uk/long-read/guidance-note-virtual-ward-care-for-people-with-heart-failure/ (accessed 14 November 2023)
- 3New RPS interim professional standards for virtual wards. Royal Pharmaceutical Society. 2023. https://www.rpharms.com/about-us/news/details/new-rps-interim-professional-standards-for-virtual-wards (accessed 14 November 2023)
- 4Quality of care. Care Quality Commission. 2023. https://www.cqc.org.uk/publications/major-report/state-care/2022-2023/quality-of-care#medicines (accessed 14 November 2023)
- 5Delivery plan for recovering urgent and emergency care services. NHS England. 2023. https://www.england.nhs.uk/wp-content/uploads/2023/01/B2034-delivery-plan-for-recovering-urgent-and-emergency-care-services.pdf#page=37 (accessed 14 November 2023)
- 6Guidance and resources to support implementation of virtual wards. NHS England: Getting It Right First Time. https://gettingitrightfirsttime.co.uk/cross_cutting_theme/virtual-wards/ (accessed 14 November 2023)



