
Shutterstock.com
Pharmacists have had to cope with an extraordinary couple of years — and the cracks are beginning to show.
Results from The Pharmaceutical Journal’s annual salary and job satisfaction survey show a significant rise in the proportion of pharmacists reporting severe stress in 2021, and it is clear that this is having a damaging effect on morale.
In this infographic, we look at the depth of the problem and what has contributed to this trend. We also ask those in power what they are going to do about it (see Box 1).
A quarter of pharmacists (25%) report being “very stressed at work”, a significant increase on previous years
There has been an approximate doubling of pharmacists reporting feeling very stressed compared with previous years (see Figure 1). There are significant proportions of pharmacists with severe stress in most sectors, with community pharmacists appearing to be the most affected.
This matches trends observed in other parts of the health service. A study of almost 3,000 NHS workers published in The British Journal of Psychiatry in April 2021 revealed that severe stress jumped from 11% to 46% during the first wave of the pandemic. Then, in September 2021, the British Medical Association’s (BMA’s) survey on the impact of COVID-19 on doctors was published, which suggested that 67% of GPs and 52% of hospital doctors are suffering from depression, anxiety, stress, burnout or emotional distress relating to, or exacerbated by, their work.
Despite the higher stress levels within pharmacy, the proportion of pharmacists taking time off work because of stress has remained at a constant low of around 4% over the past four years.
So many times, I felt I needed to take time off during too much stress and exhaustion, but the workload is too much
Community pharmacist
I try to help all the time but there’s only one me. Feels like I’m a pharmacist, dispenser, customer adviser and floor staff in a day — just burnt out
Community pharmacist
Box 1: What can be done about pharmacist stress levels?
We asked pharmacy leaders what they are going to do to combat this problem.
Gareth Jones, head of corporate affairs, National Pharmacy Association (NPA): “We are continuously lobbying government for a better long-term environment for our members. The NPA also helped secure COVID-19 costs from the government. We held discussions with senior police representatives to address violence against pharmacy staff and have also provided resources about stress and mindfulness.”
Malcolm Harrison, chief executive, Company Chemists’ Association (CCA): “The CCA continues to advocate for long-term investment in the sector and solutions to address the workforce crisis. Through the Community Pharmacy Patient Safety Group, the CCA and others have produced resources to help individuals monitor their wellbeing, including tips on what to do if an individual or a colleague is feeling under pressure.”
Leyla Hannbeck, chief executive, Association of Independent Multiple Pharmacies: “The unplanned drive of pharmacists to PCNs by NHS England combined with a lack of adequate funding has exasperated the situation. As we lose experienced pharmacists it takes time to replace them, and it has a knock-on effect on stress levels within the teams. We will continue to write to NHS England asking for help with this acute workforce challenge.”
Ewan Maule, vice president, Guild of Healthcare Pharmacists: “Nationally, there needs to be investment in recruitment to meet the needs of patients, as well as reviewing pharmacists’ workload. Within organisations, management needs to be realistic in how they organise rotas and responsibilities. Pharmacists need to ensure they are comfortable in the conditions they are being asked to operate in and that they are not putting themselves at professional or personal risk.”
Paul Day, director, Pharmacists’ Defence Association: “Our trade union recognition at major employers provides the opportunity to influence practice and tackle health & safety concerns, including causes of stress. We are utilising the Health & Safety Executive’s stress and wellbeing survey to establish a baseline of the position at three of the largest multiples in community pharmacy as part of our longer-term strategy to highlight and improve stress levels.”
Staff shortages and demand for services during the pandemic have made workload unsustainable for some
Demand for services and staff absence are cited most often as sources of stress (see Figure 2).
Workforce issues are a recurring theme, with 78% of pharmacists saying that a “lack of staff” is creating a barrier to them doing their job effectively (n=991). There have been reports of shortages of pharmacists across all sectors and pharmacists were added to the Home Office’s shortage occupation list in March 2021.
Many pharmacists who responded to our survey say that supporting the rollout of the COVID-19 vaccine programme and changing the way they work, because of the pandemic, has put additional pressure on them.
Additional work created by the vaccine programme, which we had to accommodate over and above our day-to-day jobs, has caused stress. This was easier during the lockdown as a lot of other hospital activity, meetings etc. were stood down, but much more challenging now
Hospital pharmacist
Learning to work remotely and consulting patients remotely, especially if they have a language barrier
Primary care network pharmacist
The daily unpredictable workload, increased demand, shortage of staff, not enough GP appointments, lack of support and so many other reasons have left me doing many tasks at one time, while under pressure and stress and in a rush
Community pharmacist
Almost a quarter of pharmacists (22%) say they “always work outside of their contracted hours”
Taking time away from work is a recognised way of reducing stress levels, but our survey shows that working hours have increased over the past year for almost half (46%) of pharmacists (n=1,035).
Almost half of hospital pharmacists (46%) always or very often work outside of their contracted hours, followed by 36% of community pharmacists, 35% of GP pharmacists and 19% of primary care network (PCN) pharmacists (see Figure 3).
One in six (14%) pharmacists never take their contracted breaks, with a further 28% only taking them infrequently (up to a quarter of the time) (n=1,032). Community pharmacists are least likely to always take their breaks (see Figure 4).
Despite working outside of their contracted hours, 77% of pharmacists are not always paid for working overtime (n=1,035).
There is an inability to take breaks, even to eat or hydrate, due to workload and meetings
Hospital pharmacist
When at home there are constant out-of-hours phone calls and emails from work, so you can never have time to yourself to even relax and recover physically
Community pharmacist
Physical and verbal abuse has been a problem over the past year, with 42% of pharmacists saying it has increased
Community pharmacists appear to be bearing the brunt of the abuse, with almost three-quarters (74%) saying abuse has increased over the past year (see Figure 5). Reports of increased abuse in community pharmacy have grown by 17 percentage points since our 2020 survey. Only 7% of community pharmacist respondents said they have not experienced abuse within the past year.
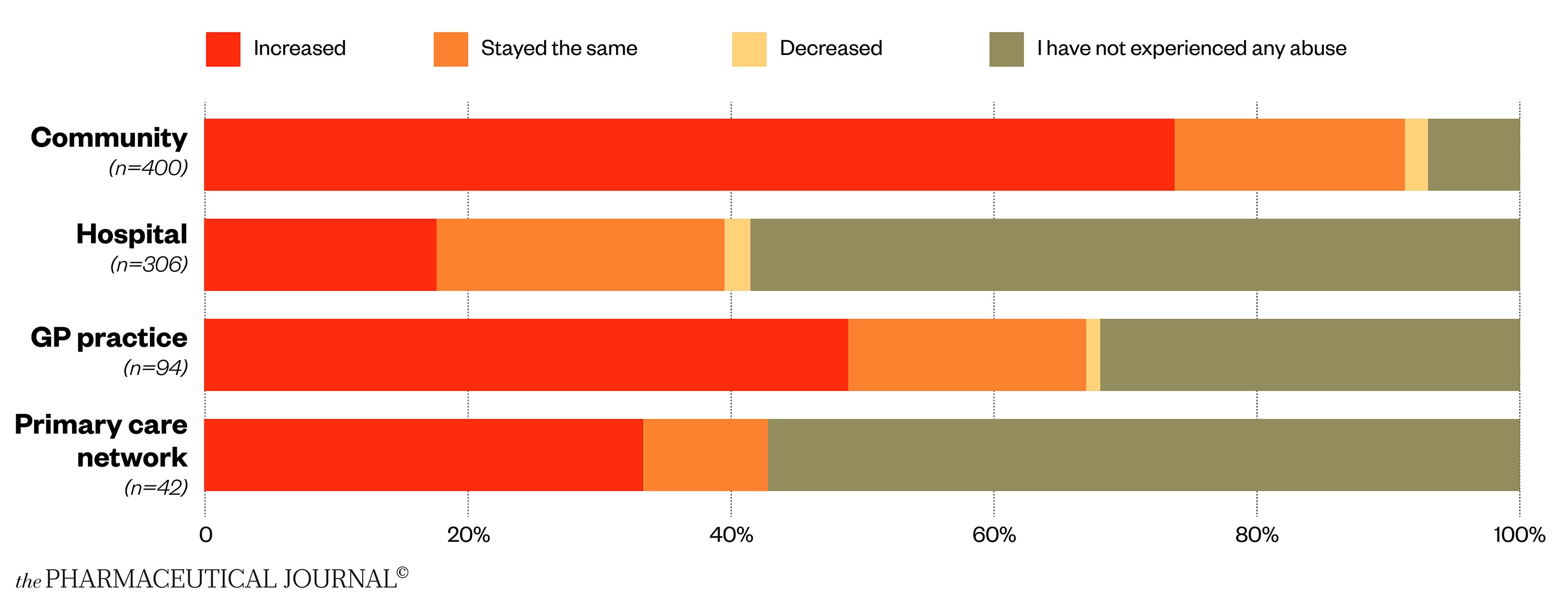
These reports of a rise in abusive behaviour towards pharmacists are supported by data from pharmacy employers and organisations. In April 2020, the Pharmacists’ Defence Association published survey results showing that more than 90% of 1,200 respondents had witnessed abusive or aggressive incidents in their pharmacies during the preceding month, and 80% of respondents thought abusive or aggressive incidents had increased compared with normal levels.
In early 2021, as a result of increased violence in its pharmacies, Boots began providing body cameras to its employees — including pharmacy staff — working in 60 stores.
GPs also feel they are under attack. A BMA survey of more than 2,400 doctors carried out in July 2021 found that 46% of GPs had experienced one to five incidents of verbal abuse, with roughly one in five (19%) receiving threats, in the previous month. Two-thirds (67%) of GPs had witnessed violence or abuse directed at other staff in their workplace in the past year, while 37% said these abusive instances had increased significantly on the same period 12 months ago.
Patients frustrated with their doctor’s practice take their anger out on us and our teams
Community pharmacist
Rudeness, verbal abuse and even threats of physical abuse
Community pharmacist
Rude, uncaring customers. No concept of infection avoidance. Pandemic denial
Community pharmacist
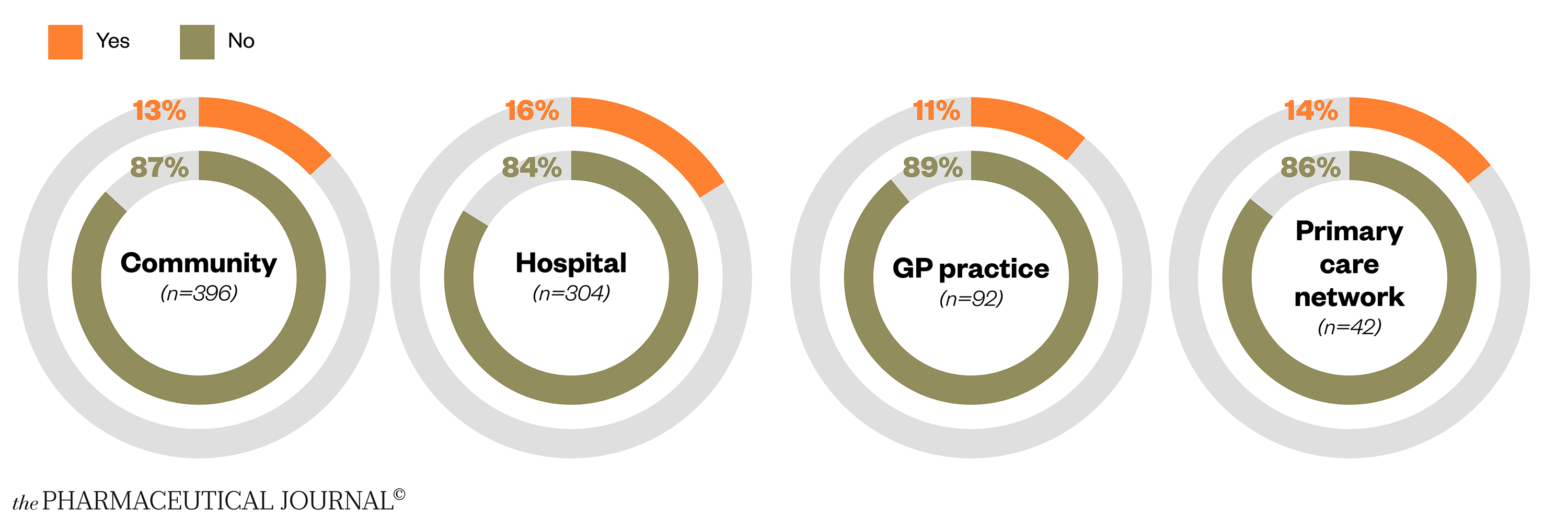
Mental health support is available, but some pharmacists struggle to access it
Most pharmacists (71%) say that mental health support is available from their employer (n=1,018), but this varies by sector. Hospitals are most likely to offer mental health support to pharmacists (85%), whereas only 54% of community pharmacists say support is available.
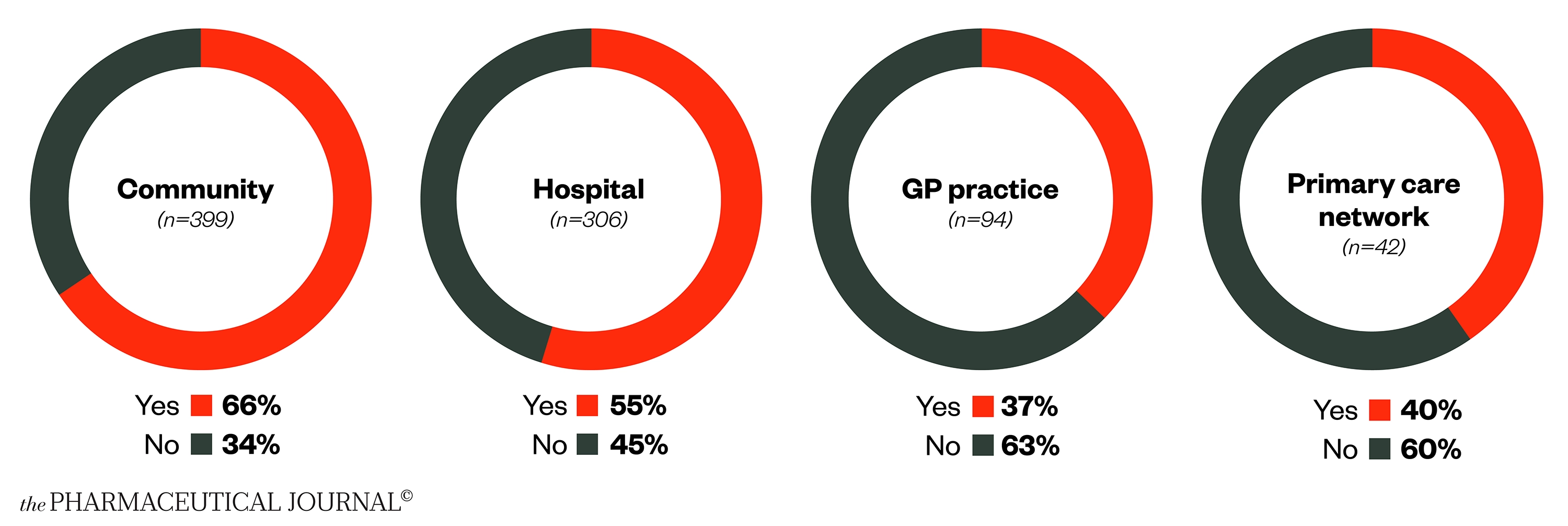
Indeed, one in five hospital pharmacists have accessed mental health support (not necessarily from their employer) during the past year, compared with around one in six of community pharmacists, and around one in ten GP practice and PCN pharmacists (see Figure 6).
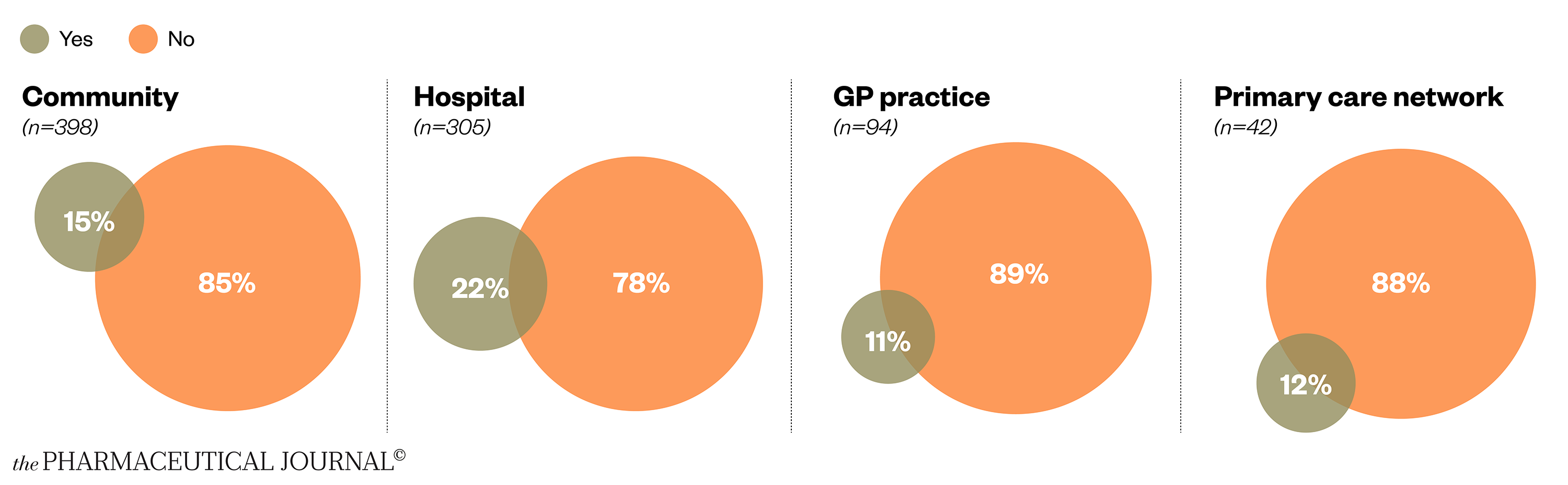
The NHS has introduced additional mental health and wellbeing support for NHS staff during the pandemic, including helplines and access to counselling (see Box 2).
However, one in six hospital pharmacists have wanted to access mental health support but not been able to, with lack of time a common reason (see Figure 7).
There is stigma associated with accessing mental health services and I feel guilty that it is exaggerating
Hospital pharmacist
I keep planning to access help, but I just don’t have time
Hospital pharmacist
When at work there is literally not a second free to even think about my own mental or physical wellbeing
Community pharmacist
Rising stress is having a corrosive effect on the morale of pharmacists
The most disturbing finding of the survey has to be the long-term effect of high stress levels on the morale of the profession. Overall, morale is low or very low for 45% of respondents (n=1,019), with a higher proportion of pharmacists in all sectors experiencing low morale compared with 2020. Community pharmacists have seen the biggest increase, from 35% in 2020 to 59% in 2021, followed by hospital pharmacists (from 32% to 47%), GP practice pharmacists and PCN pharmacists (up from a combined figure of 20% to 28% and 24%, respectively) (see Figure 8).
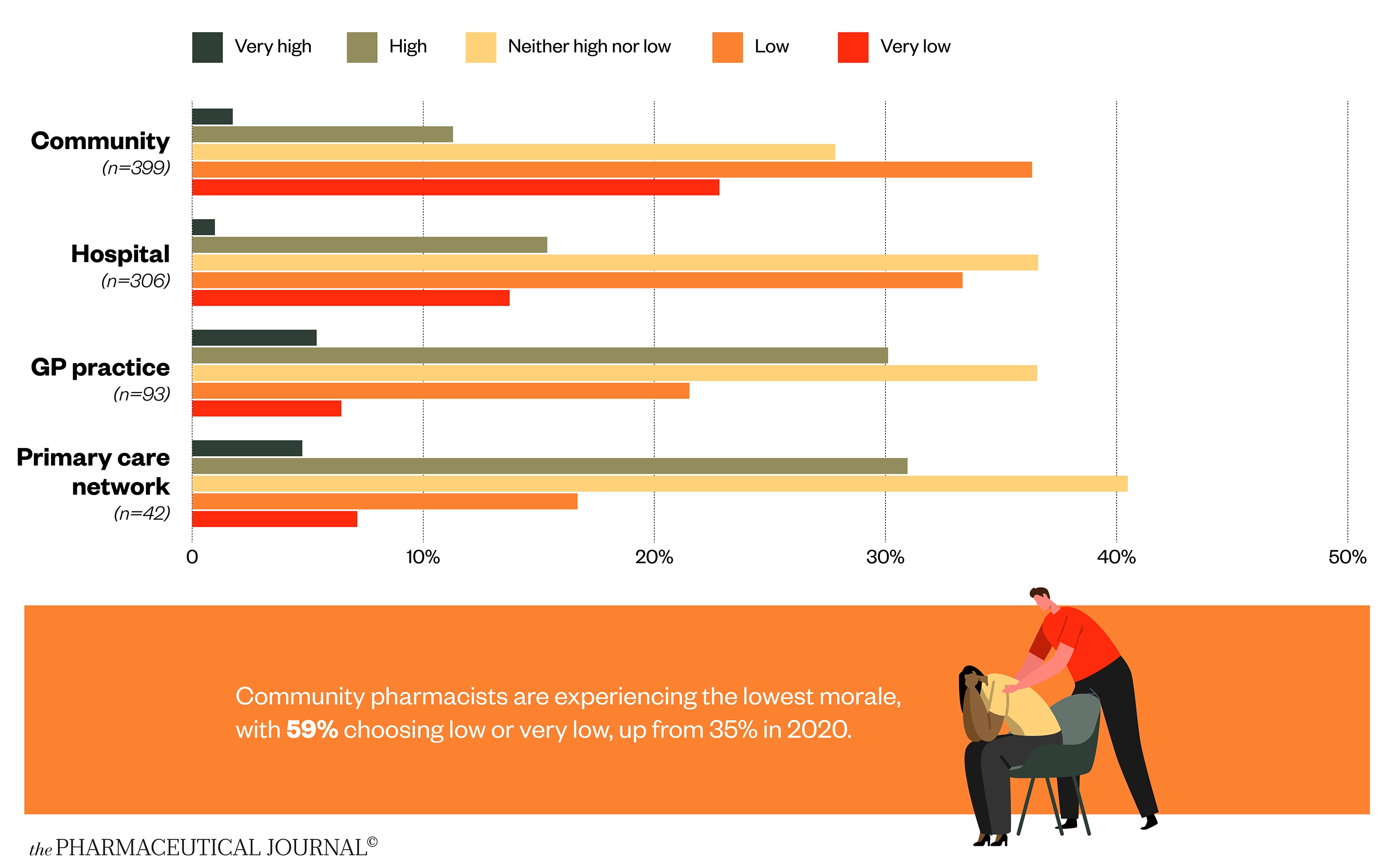
This low morale translates to many pharmacists feeling that the profession is no longer the career for them. Some two-thirds of community pharmacists have considered leaving the profession within the past 12 months (see Figure 9).
Poor management and poor communication of constant changes and poor communication of plans, lack of support from managers, low staffing levels in general, other staff being stressed leading to strain and poor morale
Hospital pharmacist
Morale is at its absolute lowest. We are constantly having to deal with inappropriate referrals from other healthcare staff
Community pharmacist
Box 2: Where to go if you are struggling
Pharmacist Support: A charity supporting pharmacists and their families, former pharmacists and pharmacy students. The charity now provides direct psychological support for those who are experiencing mental health issues, funding up to 12 counselling sessions.
NHS mental health and wellbeing support: All NHS health and care staff in England can access mental health support via 40 staff mental health and wellbeing hubs around the country. All regulated health and social care professionals can access support in Scotland via the Workforce Specialist Service. The Health for Health Professionals Wales is a free mental health support service for doctors that was expanded in April 2020 to provide support and advice for all frontline NHS Wales staff.
Helplines and free wellbeing apps: NHS England has introduced a confidential NHS staff support line, operated by the Samaritans, which is free to access from 07:00–23:00, seven days per week, on 0800 069 6222. Trained advisers can help with signposting and confidential listening. Support can also be accessed by texting FRONTLINE to 85258 for support 24/7. NHS staff have also been given free access to several wellbeing apps.
The National Wellbeing Helpline (0800 111 4191) in Scotland provides a compassionate listening service that is available 24/7 and can offer advice and signposting to local staff support services, when required. A National Wellbeing Hub also offers a broad range of advice and evidence-based digital resources to help staff with issues such as stress, anxiety, low mood, insomnia/poor sleep and resilience.
Box 3: Survey methodology
The Pharmaceutical Journal salary and job satisfaction survey was conducted on 1–29 September 2021. The analyses, carried out by independent statisticians at the University of Aberdeen, included 1,112 non-locum pharmacists practising in Great Britain. Community pharmacists were under-represented compared with the General Pharmaceutical Council (GPhC) register (37% vs. 63%) and hospital pharmacists were slightly over-represented (28% vs. 23%). The proportion of pharmacists working in primary care was roughly comparable with those on the GPhC register (13% vs. 12%). Female respondents were slightly over-represented (73% vs. 62%) and pharmacists of a black, Asian or ethnic minority (BAME) background were under-represented compared with the proportion of pharmacists who identify as BAME within the profession (28% vs. 45%).


