This content was published in 2013. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
How do you feel when you hear the terms “adherence”, “concordance” or “compliance”? You could be forgiven for feeling somewhat cynical since, in recent years, we pharmacists have been urged constantly to improve medication adherence while the demands placed on us seem evermore intense. Some of us may even feel guilty because although we would like to do more to help patients get the best out of their medicines, the reality is that the barriers to developing our practice in this area have not changed much. And yet we know that non-adherence increases medicines waste and adversely affects patient outcomes.
REFLECT
- What sort of consultation style do you use?
2 What are the benefits of a patient-centric approach?
3 What four elements should patient consultations include?
Before reading on, think about how this article may help you to do your job better.
It has been reported that one adherence-related initiative, the new medicine service in England, has resulted in a third of patients starting to taking their medicines correctly [1]. However, there is still a significant journey ahead if we are to achieve the paradigm shift [2] to the point where the whole profession prioritises taking responsibility for continued improvement in medication adherence for both clinical and economic benefit.
Meeting this challenge requires application by pharmacists of not only their clinical skills but communication skills as well. The recent Modernising Pharmacy Careers proposals make it clear that we really must up our game in the area of patient consultation skills to improve the safety, value and effectiveness of medicines [3]. (A task and finish group has been set up to make recommendations for a national model for enhancing the consultation and communication skills of pharmacists and pharmacy technicians [4].)
Many GPs are receiving health coaching skills development inorder to incorporate thisapproach into their shortconsultations [5]. It is our contention that the use of coaching skills during consultations could also provide pharmacists with the greater flexibility required to respond to patients needs and support the delivery of medicines optimisation. This will help to ensure the rightful place of pharmacists in the provision of healthcare services.
Product versus patient
The National Institute for Health and Care Excellence defines adherence as “the extent to which the patient’s behaviour matches agreed recommendations from the prescriber” [1]. It is thought that improved adherence can result from concordant consultations.
And emerging evidence suggests new ways of interacting with the patient can improve patient outcomes and reduce costs and waste [6,7]. It can be argued that pharmacists traditionally favour a product-centric approach to patient consultations, providing information on the safe and effective use of medicines. And when advice on choosing options for medicines use is required, what appears to be the right advice may not be if the pharmacist makes assumptions about the patient’s needs. We believe that a patient-centric approach provides greater opportunity for adherence support, where product knowledge can be used to support the patient’s agenda in medicines taking.
The benefits of a patient-centric approach include:
- Providing targeted support according to the needs of the patient
- Understanding the patient perspective around medicines use
- Supporting patients with decision-making
Consultation styles
To maximise the benefit of every consultation, pharmacists need to be able to use a range of consultation styles, which can be described as located along a continuum that ranges from a product-centric approach at one end to a patient-centric approach at the other (see Figure 1).
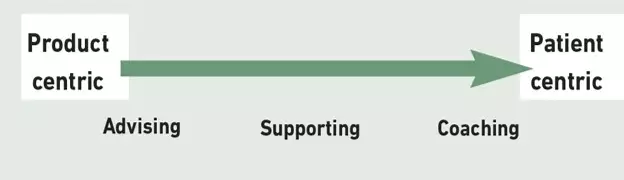
We do not advocate that one style is better than another, rather it is the choice of style appropriate to the patient and situation that optimises the benefit of the consultation.
Although it is likely that every consultation will contain elements of a number of different styles, one or two will predominate. Often, the style used is influenced by the skills and preferences of the pharmacist, rather than the needs of the patient but, by increasing familiarity with a wider range of styles, a more patient-centric focus is possible.
Descriptions of three consultation styles are given below, with suggestions for how and when to use them.
Advising
Advising patients about products represents the traditional consultation most pharmacists are familiar with: telling the patient facts about the medicine. Although information transfer has its place, its limitation is that there is no indication of what patients think about what they are hearing, what they already know and whether they are even registering the information you are giving. Advising can be patient centric, however, if a patient receives information that is highly pertinent to his or her individual situation. For example, if a patient tells you he or she knows little or nothing about a medicine, or is unsure of what he or she knows, it is useful to ask “What would you like to know?”, and to base your advice on this. By exploring the patient’s needs at the beginning of each consultation, the pharmacist can provide tailored advice. The pharmacist can still give the patient essential information to ensure he or she can use the medicine safely and effectively (eg, “Rinse your mouth with water after using your [steroid] inhaler to remove any traces and reduce the risk of oral thrush”). However, framing it in the context of information the patient has asked for, makes it likely for the patient to be more receptive. Advising is useful for educating patients in response to information they have asked for, particularly when patients know little or nothing about their medicines or condition and need the pharmacists’s expertise and guidance to manage their medicines. If the patient has some knowledge, the pharmacist can determine whether it is sufficient for the patient’s needs by asking “What else would you like to know?”.
This consultation style can also be used to provide evidence to correct any misunderstandings or misconceptions patients have about their medicines or condition or to provide specific information after finding out what patients know, what they perceive the benefits of a medicine to be, or what concerns they have. When advising, it is helpful to use the teachback technique to ensure that the patient has understood the information and to support the pharmacist’s understanding of the patient’s perspective [8].
This can commonlybe addressed through thestatement: “To be sure that I have explained things clearly, let’s review what we discussed. Please tell me how you are going to take/what you understand about this medicine.”
It is helpful for the patients to summarise what has been discussed so far because this allows pharmacists to check understanding and patients to consolidate what they have understood. Patients can be asked what they want to do now about their medicines taking.
If the patient decides not to take a medicine, the pharmacist must be ready to manage this positively, encouraging consideration of alternative health improvement strategies and obtaining permission to liaise with or refer to other relevant health care professionals.
Key points
- Consider the patient benefit of exploring, educating, empowering and enabling in each consultation.
- To maximise the benefits of every consultation pharmacists need to be able to use a range of consultation styles.
- Giving advice is patient-centric if a patient receives information relevant to his or her individual situation.
- A supportive style is appropriate for patients who want to optimise their adherence but have not yet made the necessary changes.
- Coaching promotes patients as their own problem solvers. Patients are more likely to act on suggestions they make themselves.
Supporting
A supportive style is appropriate for patients who want to optimise their adherence but have not yet made the necessary changes.
Pharmacists can help patients weigh up the benefits of the medicine and the impact of not adhering against the barriers to adherence. The pharmacist’s intention should be ensure patients have all the facts they need to evaluate the benefits and risks, consider the impact of non-adherence and explore methods to overcome barriers in order to maximise their desired health outcome. For example, if a patient says: “I would like to take my glibenclamide but I’m worried about putting on weight”, possible responses from the pharmacist could include:
- How do you think this medicine will benefit or has benefited you?
- How important are these benefits to you?
- How well have you felt since taking this medicine?
- What do you think might happen to you if you don’t take the medicine as intended?
- If your condition does not improve, what do you think could happen? How might this affect you and how might this make you feel?
- What else could you do to manage weight gain [ie, side effects]?
The pharmacist may need to provide factual information and advice in response to answers to these questions from the patient. This method allows the pharmacist to bring patients’ expertise and experience of their medicine and condition into the discussion and use their own expertise in medicines to work together with the patient to empower positive change.
Again, to ensure patients own their decision to take a medicine following the discussion, it is useful again to ask them what they would like to do about medicines taking.
Coaching
There are many definitions and types of coaching. A health coaching approach (see Panel 1) has much to offer in support of medication adherence. In the context of pharmacy consultations, health coaching skills can be used to raise patients’ awareness of medicines issues and increase their personal responsibility for managing medicines optimally to improve their health.
Panel 1: Health coaching
“Health coaching is a behavioural intervention that facilitates participants in establishing and attaining health promoting goals in order to change lifestyle-related behaviours, with the intent of reducing health risks, improving self-management of chronic conditions and increasing health-related quality of life.” [9]
Coaching to support adherence promotes patients as their own problem solvers, whereas the more traditional approach focuses on pharmacists trying to solve the problem for patients or directly instructing them. The principle is that if patients decide the approach they will take to medicines taking with our support, they are more likely to act on their own suggestions.
So health coaching is a style that involves approaching the consultation from the patient’s perspective. For pharmacists this approach is the least intuitive because traditional pharmacy teaching considers the pharmacist to be the medicines expert with a responsibility for providing instruction and advice. A coaching approach takes into account not only pharmacists as medicines experts but also patients as experts on their lives, so that a consultation is about the meeting of two expert equals.
Key features of coaching include:
- Belief that patients have the potential to solve their own adherence issues
- Holding yourself back and letting the patient do the thinking
- Asking open questions to solicit ideas rather than telling or suggesting options
- Being non-judgemental
- Encouraging patients to choose their preferred option rather than suggesting your preferred option, opinions or solutions
- Accepting a patient’s solution even if it is not one you would choose yourself
Health coaching for medication adherence encourages patients to develop their expertise and learning about their medicines continually. It helps them to manage their condition and resolve problems, thereby facilitating patient self-care. Coaching is a patient-centric approach in which patients are empowered to generate their own options, supported by provision of factual information by pharmacists where appropriate. For example, “There is a soluble version of this tablet available. Would that be useful?” or “Would it help to know that you can ask for ordinary caps on your medicine instead of child-proof ones?” Panel 2 lists some useful questions for health coaching, either during a medicines use review or over the counter.
Panel 2: Useful questions
- What would you like to know about your condition and your medicine(s)?
- What benefit do you feel your medicine gives you?
- How important are the benefits of this medicine to you?
- What, if anything, are your worries about your medicine?
- What would you like your medicine to allow you to do? (eg, feel well enough to walk the dog)
- How well have you felt since taking this medicine?
- What do you think might happen if you don’t take this medicine as intended?
- If your condition doesn’t improve, what do you think could happen? How might this affect you?
- What would you like to do about taking your medicine (following discussion of benefits and risks)?
- How would you like to manage your condition/medicines?
- How will you fit your medicines into your day?
- How will you know if this is working for you?
- What will you do to find out if the medicine is working for you?
- What would you like to do now about your medicines taking
Change
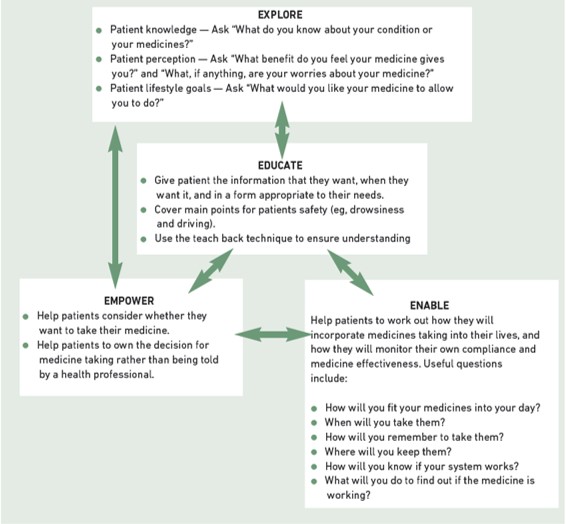
We suggest that the framework of the four Es [10] (see Figure 2) can help support the use of a wider variety of consultation skills — we recommend beginning the consultation by exploring the patient’s needs and then using the consultation style most appropriate to those needs.
We cannot ignore the need for change. The role of pharmacists as information providers is both necessary and highly valued by patients. However, improving medicines adherence requires the use of a range of consultation styles tailored to patient need and which effectively bridge the gap between the pharmacist and patient perspectives. A coaching approach expands the pharmacist’s range of communication skills in a way that facilitates working smarter not harder to deliver continued improvements in medicines adherence.
Further reading
Hibbard J, Tusler G. Improving the outcomes of disease management by tailoring care to the patient’s level of activation. American Journal of Managed Care June 2009;6:353–360 discusses the use of health coaching within patient consultations.
The citation information is currently available. For more information please contact pharmpress-support@rpharms.com
Practice points
Reading is only one way to undertake CPD and the regulator will expect to see various approaches in a pharmacist’s CPD portfolio.
1. Adopt the teachback technique into your consultations. Does it make a difference?
2. Ask a colleague to observe your consultations and suggest how you could be more patient-enabling in your approach.
3. Use open questions wherever possible.
Consider making this activity one of your nine CPD entries this year.
Further learning
We recommend the e-learning introduction at http://mentoring.londondeanery.ac.uk/coaching-for-health/e-learning-module
Health coaching training is available from various sources. Information about NHS health coaching programmes is available at www.eoe.nhs.uk/page.php?page_id=2179 and www.londondeanery.ac.uk/global-news/coaching-for-health-programme.

