
Alison Young
This content was published in 2010. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
In 2008, the British Society for Parenteral and Enteral Nutrition (BAPEN) reported that a quarter of patients admitted to NHS hospitals and a third of residents admitted to care homes were malnourished or at a high risk of becoming so.1 According to a later report,2 about three million people in the UK are malnourished or are at risk of becoming so, at an estimated cost of £13 billion from increased medical and social services. For these people, nutritional support is essential and, in some cases, will take the form of parenteral or enteral nutrition.
Parenteral nutrition can meet all the needs of adults unable to be fed by the oral or enteral route over prolonged periods and was discussed in a previous CPD article (PJ, 12 September 2009, pp275–8). However, most malnourished people have a functioning gastrointestinal tract capable of absorbing nutrients and it is desirable for them to be fed orally or, where needed, enterally (through a tube placed into the stomach or jejunum).
Pharmacists will come across enterally fed patients in hospitals but also, increasingly, in the community, particularly in care homes. They may be required to dispense feeds (although many are delivered direct to homes by manufacturers) or they might be asked about the administration of medicines via feeding tubes.
Indications for enteral feeding
Nutritional support is of most benefit in adults who are malnourished (or at risk of this) and who are unable to obtain sufficient nutrition from food or drink. Typically this may be caused by or associated with:
- Anorexia
- Dysphagia (often due to diseases of the oesophagus or neuromuscular disorders, or following stroke, upper gastrointestinal tract surgery or radiotherapy)
- Malabsorption states (these are common in patients with inflammatory bowel disease or following some gastrointestinal surgery)
- Chronic vomiting or diarrhoea
- Excessive nutrient losses or high demands for nutrients, such as in cachexia (severe muscle wasting, which is seen in several medical conditions) or in patients with pressure sores or open wounds
Malnutrition increases morbidity and mortality from disease, surgery and trauma, and in 2006 the National Institute for Health and Clinical Excellence published guidance recommending that all patients admitted to hospital or seen in outpatient departments be screened for malnutrition.3 This guidance also defined malnutrition and being at risk of malnutrition (see Panel 1).
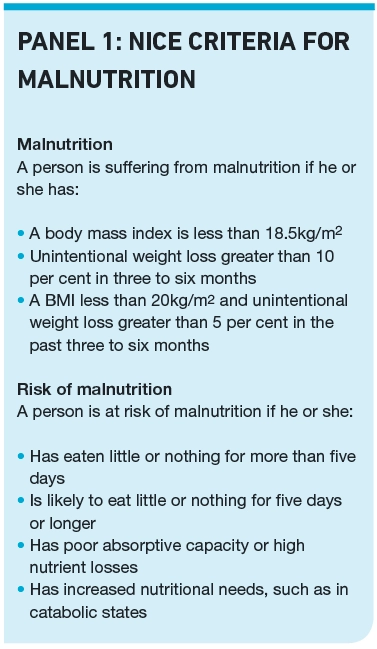
Patients with malnutrition or at high risk of it can be identified by using a screening tool such as the BAPEN malnutrition universal screening tool (MUST; available at www.bapen.org.uk), which is usually adapted locally. This tool is not only based on the patient’s body mass index but also on any recent weight loss and medical conditions. Once a risk is identified, nutritional help and advice should be given. Oral supplementation, enteral tube feeding or parenteral nutrition can be considered.
Enteral tube feeding is safer and cheaper than parenteral feeding. It is preferred if the patient has adequate gastrointestinal absorptive capacity because it more closely mimics normal feeding, and healthy gut function is more likely to be maintained. Enteral tubes can either be placed through the nose (nasogastric or nasojejunal tube) or through the abdominal wall (gastrostomy or jejunostomy tubes). Tubes are usually made of polyurethane or silicone, which are not affected by gastric acid.
Reflect
- How is malnutrition defined by the National Institute for Health and Clinical Excellence?
- What factors affect the type of nutrition administered through enteral feeding tubes?
- How should medicines be administered through feeding tubes?
Before reading on, think about how this article may help you to do your job better.
Nasogastric and nasojejunal tubes
In hospitals, gastrointestinal access for up to six weeks is usually achieved using fine-bore (ie, less than 9 French gauge) nasogastric or nasojejunal tubes. These cause less irritation to the nose and oesophagus (and so present fewer gastric reflux risks) than the wider-bore PVC tubes (sometimes called Ryles tubes) that are typically used for aspirating gastric contents, and which are sometimes used for feeding after aspiration.
Nasogastric tubes administer feed directly into the stomach. Surgery or swallowing problems can lead to reflux or delays in gastric emptying. If gastric feeding is difficult or unsafe (due to a risk of aspiration of gastric contents) and nasojejunal tubes are used, administering feed past the pyloric sphincter of the stomach.
Higher feeding rates are usually better tolerated and the use of more concentrated feeds (eg, over 1.5kcal/ml) is possible using nasogastric tubes.
The insertion of a nasogastric tube involves passing the tube (with the end lubricated with water or KY jelly) through the nostril, pharynx and oesophagus, into the stomach. (The patient is instructed to swallow and the tube is advanced as he or she does so.) The positioning of the tube in the stomach is confirmed by testing the pH of aspirate (usually indicated by a pH less than 5.5, unless the patient is on acid suppressants or antacids). The tube is secured in position with tape and usually goes over the ear. Nasojejunal tubes are inserted with the aid of endoscopy. Metoclopramide has been used to aid insertion.
PEG and JEJ tubes
Where feeding is required for longer than six weeks (for example, because the patient is unlikely to recover his or her ability to feed orally in the short term), gastrostomy or jejunostomy tubes are used (usually following a patient compatibility trial with a nasogastric or nasojejunal tube). Gastrostomy or jejunostomy tubes are inserted endoscopically or surgically. They are more discreet and, if cared for properly, are more comfortable for the patient than nasogastric or nasojejunal tubes.
Typically, a percutaneous endoscopically placed gastrostomy (PEG) tube is inserted through the abdominal wall into the patient’s stomach (radiologically inserted gastrostomy tubs [RIG] are an alternative). Where postpyloric feeding is indicated, a jejunostomy (JEJ) tube can be placed into the small intestine. Like nasojejunal tubes, JEJ tubes are useful in patients at risk of reflux.
Overall, mortality within a few weeks of PEG tube placement is high but this is usually due to the patient’s condition rather than the tube — PEG tubes are sometimes placed (inappropriately) in patients with poor prognoses (eg, following severe stroke).
Feed administration
Feeds can be given intermittently, continuously or as a bolus. Intermittent infusion (cycled feeding by gravity or via a pump system) over 16 to 20 hours has its proponents but overnight feeding is also possible if the patient is not at risk of aspiration (a complication of tube feeding where feed is inhaled into the lungs, with associated risks of aspiration pneumonia). Continuous infusion can also be considered but, generally, regimens that more closely mimic normal feeding are preferred. There is conflicting evidence that continuous feeding leads to higher gastric pH levels and bacterial overgrowth.
In nasogastric or gastrostomic feeding intermittent or continuous infusion are not essential but they can prevent “dumping” in some patients, where stomach contents are transported (dumped) into the small intestine too quickly. Common symptoms include abdominal cramps and nausea but dumping can also lead to sudden surges of dextrose in the blood. Continuous infusion or cycled feeding is also preferred in patients with insulin-dependent diabetes, who require a steady availability of carbohydrate.
Bolus feeding involves the administration of 200–400ml of feed down a PEG tube over 15–60 minutes at regular intervals. If a patient has a fine bore nasogastric tube, an enteral syringe (these are purple) can be used for bolus feeding but this regimen is timeconsuming.
In jejunal feeding, the absence of the stomach to act as a reservoir means that continuous or cycled infusions are essential to avoid dumping syndrome.
As mentioned above, continuous or overnight nasogastric or gastrostomy feeds should not be given to patients at risk of aspiration (eg, bed-bound patients). The risk of aspiration of feed in bed-bound patients can be minimised if the patient is propped up at an angle of 30 degrees or more during and for 30 minutes after feeding.
Tubes should be flushed before and after feeds. Normal water can be used for gastric feeding but for jejunal feeding, where no stomach acid is involved, some clinicians recommend sterile bottled or freshly boiled and cooled water.
In general, tube feeds should not be diluted and nothing should be added to them because bacterial contamination of the feed increases the risk of infection and can give rise to sepsis, pneumonia and gastrointestinal problems. Closed systems are preferred. Feeds should not be decanted and any feed containers should be discarded after 24 hours.
Nutrient requirements
The 2006 NICE guidance3 recommends that healthy people should be provided with 25– 35kcal/kg/day, including calories from protein. More specifically, protein intake should be between 0.8–1.5g/kg per day (ie, 0.13–0.24g nitrogen per kg per day, where 6.25g protein = 1g nitrogen).3
In seriously ill or injured people feeding should be started at no more than 50 per cent of their estimated energy and protein needs and be built up to meet full needs over 24 to 48 hours. Over-feeding can be risky after major surgery, in septic patients and in multiorgan failure because it can lead to complications, such as deranged lipid profile, hyperglycaemia and increased carbon dioxide production — these types of patient should be reviewed regularly and underfed until their condition improves and they become anabolic. This is termed “permissive underfeeding”.
Reduced nutrients (and volumes) are initially required in patients who have not eaten for over five days, but special starter regimens are unnecessary in patients who have had a reasonable nutritional intake in the previous week. Dietitians will assess a patient’s nutritional status and history and recommend a regimen taking into account the recipient’s needs and preferences. Where prolonged malnutrition has led to a risk of refeeding syndrome (see below), a maximum of 10kcal/kg/day should be used initially and only increased slowly to full needs over four to seven days.
Fluid needs can usually be met by giving 30–35ml/kg of body weight per day, but patients’ needs will vary. For example those with an ileostomy will require more fluids because of increased losses via the stoma.
Most feeds contain enough electrolytes to meet typical daily requirements for sodium, potassium, calcium, magnesium, and phosphate. However, patients with malnourishment or metabolic stress are often salt and water overloaded and normal feeds may not be appropriate. Too much sodium can also be a problem in patients with renal or liver problems, or cardiac failure. On the other hand, where intestinal losses are excessive, additional sodium may be needed.
More potassium, magnesium and phosphate than normal is needed after starvation to restore and maintain stores and plasma levels, and to allow protein synthesis to proceed optimally. More potassium is also required in patients receiving diuretics or insulin. Hypomagnesaemia due to diureticinduced excretion, stoma losses, fistulae or diarrhoea can worsen hypokalaemia. Correcting potassium, magnesium and phosphate deficiencies while feeding can reduce or prevent refeeding problems.
Essential vitamins, minerals and trace elements are required for the prevention or correction of deficiency states and maintenance of normal metabolism and antioxidant status. Standard enteral feeds providing total daily energy needs contain daily recommended micronutrient requirements but these may not suffice if there are increased demands due to illness, preexisting micronutrient deficits, poor absorption or when full enteral tube feeding is not tolerated in the initial period of feeding.
Refeeding syndrome, a set of metabolic complications seen when feeding is started after prolonged malnutrition due to a depletion of certain electrolytes (especially phosphates) and water soluble vitamins, can be life threatening, resulting in cardiac or respiratory failure or other problems. NICE recommends the prescription of B vitamins, especially thiamine, when starting feeding in the very malnourished, along with a gentle start to nutrition.

Monitoring
Enteral tube feeding is effective and safe but carries a number of risks that close monitoring can prevent. Metabolic complications of enteral tube feeding, in addition to refeeding syndrome, include hyperglycaemia, electrolyte disturbances, clotting disturbances and oedema due to fluid overload. (In hospital fluid balance records and regular body weight are useful when assessing fluid status.) Initially, electrolytes and blood glucose need to be checked daily, and weekly full blood counts and liver function tests are required until the patient is stable.
Nasogastric and nasojejunal tubes are easily displaced so their position should be checked before each feed (testing tube aspirate with litmus paper). Gastrostomy and jejunostomy sites should be checked daily, both for tube positioning and infection. The patency of tubes should also be checked.
Patients should also be monitored for adverse effects. Gastrointestinal problems, such as bloating and diarrhoea, are common in enterally fed patients, especially initially, due to dumping or the osmotic load of the feed, gut atrophy or abnormal motility. In addition, the absence of normal eating mechanisms (eg, chewing) can affect gut motility and absorption.
Once infective causes are excluded changing the feed from a standard feed, such as Jevity, to a semi digested peptide feed, such as Perative, can help, as can a switch to continuous infusion, although this should be changed to intermittent infusion as soon as possible.
Sometimes diarrhoea can be helped by having breaks of four to eight hours in feeding, or changing to a fibre-containing feed. Many medicines can cause or aggravate diarrhoea, including H2 blockers, proton pump inhibitors, antibiotics, magnesiumcontaining antacids, antiarrhythmics, antihypertensives and non-steroidal antiinflammatory drugs. Antibiotics can affect colonic flora and reduce short-chain fatty acid production from insoluble carbohydrates and fibre. Some liquid medicines contain sorbitol, which has laxative properties, while others have a high osmolality and can cause osmotic diarrhoea, especially with jejunal administration. Pharmacists can advise on alternative products and formulations if diarrhoea persists.
A motility agent, such as metoclopramide, may be considered for patients with slow gastric emptying.
Choice of feed
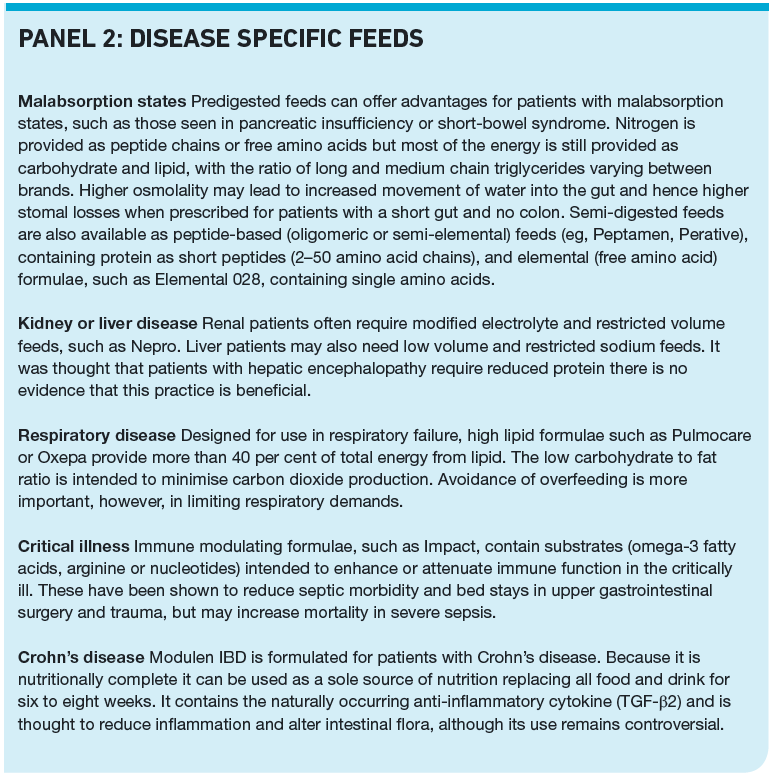
Choice of feed is influenced by gastrointestinal absorption or motility problems and other co-morbidities, such as renal or liver disease.
Feeds are prescribable (on FP10, GP10 and WP10) for disease-related malnutrition, malabsorption states and dysphagia. Allowed feeds are listed in appendix 7 of the British National Formulary and prescriptions should be endorsed “ACBS” (ie, Advisory Committee on Borderline Substances approved for specific indications). Although oral sip feeds (eg, Ensure Plus) do not fit into the narrow definition of enteral feeding some can be given through feeding tubes so will also be considered in this section.
Enteral and sip feeds provide varying amounts of nutrients and fluid from differing combinations of fat, carbohydrate and protein. The variety of feeds available include those that are nutritionally complete when given in the recommended amount, and which be used as a sole source of nutrition, and those that provide calories but lack other essential components of a complete diet so are intended to be used as supplements.
Nutritionally complete feeds commonly seen include Ensure Plus and Fortisip and these are suitable for sip feeding or bolus administration into the stomach via a PEG tube but are not suitable for jejunal feeding. Jevity and Nutrison are examples of complete feeds used in tube feeding only.
Not all patients who are tube fed are unable to eat. Some may be able to eat small amounts but need enteral feeding to ensure their full nutritional requirements are met (ie, these people may be prescribed enteral feeds in addition to dietary and other oral supplements). Well known feeds that should not be used as a sole source of nutrition and are intended for use as supplements include Ensure Plus Juce, Fortijuce, Scandishake and Vitasavoury Soups. Calogen is a popular fat emulsion that provides high levels of calories but little else.
Most feeds contain a partially hydrolysed starch as the carbohydrate source, whole protein for nitrogen, and long-chain triglycerides (LCT) to supply lipid. Energy supply can vary from less than 0.9kcal/ml (low) to more than 1.2kcal/ml (high). Very calorie dense formulae have recently been marketed, providing 2kcal/ml or above and these benefit patients with fluid restriction, such as in chronic kidney disease or cardiac failure and for adults with early satiety.
Most feeds are available as fibrecontaining or fibre-free, and are generally gluten free. Traditionally, enteral feeds were fibre-free because fibre was thought to cause tube obstruction, but the normal recommended fibre intake of 15 to 30g per day can be provided by the enteral feed. In fact, fermentable (soluble) fibre from guar gum, pectin and soy polysaccharides, and non-fermentable fibre (non-soluble), such as oat fibre, are beneficial to maintain gut physiology, prevent diarrhoea and constipation, and for glycaemic and lipid control. Fermentable fibre is broken down to short-chain fatty acids in the colon.
More recently, oligosaccharides, such as inulin, and fructo/galacto-oligosaccharides, are being introduced to feed formulations because they are also metabolised by gut bacteria, resulting in improved gastrointestinal function.
Many feeds are described as “clinically lactose free”, containing less than 1g lactose per 100ml of formula. These are suitable for patients with primary or secondary lactase deficiency (caused by gut damage due to inflammation, infection, short bowel or rapid small bowel transit time) where malabsorption of lactose would cause diarrhoea.
Soya protein formulae are available for patients with intolerance to dairy products.
The long-chain omega-3 fatty acids DHA (docosahexaenoic acid) and EPA (eicosapentanoic acid) present in oily fish have been linked with health — particularly cardiovascular — benefits. Increasing omega-3 intake may also have a role in the prevention of dementia. Feeds that include fish oils in their formulation are now available. Panel 2 describes some disease specific feeds.
There is an increasing range of nutritional products available. These impose a significant acquisition cost implication on purchasers and for this and clinical reasons patients should be assessed by a dietitian or experienced health professional before and while receiving enteral nutrition in order that only appropriate products and quantities are prescribed. For patients requiring a vegan or religious diet, the suitability of individual products should be confirmed with manufacturers.
When patients are discharged from hospital on continuing enteral tube feeding, care must be taken to ensure that the arrangements for the supply of feeds and equipment is in place and that all carers are fully informed. Whether the feeds are intended for bolus or infusion administration needs to be specified. Although enteral feeding is usually started in secondary care, GPs can also refer patients for placement of feeding tubes. Patients are managed by a community dietitians and may be followed up by hospital nutrition teams as outpatients. Health care professionals should also be aware of the potential impact of tube feeding on the eating habits of carers, who may not bother preparing proper meals, if they are just cooking for themselves.
Medicines
Pharmacists may be asked to advise on the administration of medicines via feeding tubes as well as possible interactions between drugs and feeds.
Most medicines are not licensed for administration through enteral tubes. In general, medicines administered via an enteral feed tube should be given separate from the feed, flushing the tube with water before and after each medicine and only used after establishing compatibility with the feed.
The much-reduced bioavailability of phenytoin is the best known example among many drug-feed interactions and feed should be stopped for two hours before phenytoin is given. Some advice is based on recommendations given with products dispensed for oral use so, for example, tetracycline should not be given with milky feeds and if penicillin is given, feeds should be stopped for an hour before and after dosing (see Resources for further details).
Dispersible tablets, elixirs or suspensions are preferable to syrups because of the effects of high osmolality (eg, diarrhoea).
Blockage of tubes is common if adequate flushing is not performed after each administration of both feed and each medicine. Crushed tablets, potassium, iron supplements and sucralfate are particularly likely to cause blockage problems. Unblocking can be attempted (usually by nursing staff) by flushing with warm water or an alkaline solution of pancreatic enzymes, but sometimes tubes will need to be replaced.
Summary
With an increasing awareness of the potential morbidity, mortality, and financial burdens associated with malnutrition, enteral and oral sip feeds are being increasingly used based on a strong evidence and NICE recommendations. A general knowledge of enteral feeding is, therefore, of value to pharmacists.
Practice points
Reading is only one way to undertake CPD and the regulator will expect to see various approaches in a pharmacist’s CPD portfolio.
- Familiarise yourself with sections 7.1 to 7.4 of appendix 7 in the British National Formulary. Consider typical indications for patients to be receiving enteral or oral nutrition.
- Discuss with a colleague what you would consider if asked to recommend a medicine for administration via an enteral feeding tube.
- Make sure you can describe the differences between the various enteral and oral feeds and supplements available.
Consider making this activity one of your nine CPD entries this year.
Resources
- “The handbook of drug administration via enteral feeding tubes” (R White et al, Pharmaceutical Press) is a practical guide to the safe administration of medicines via enteral feeding tubes. It includes information on drug therapy review, medication formulation choice and unlicensed medication use as well as guidance on the safe administration of specific drugs and formulations.
References
- Russell CA, Elia M. Nutrition screening survey in the UK in 2008. British Association for Parenteral and Enteral Nutrition (BAPEN), 2008.
- Combating Malnutrition: Recommendations for Action BAPEN 2009.
- Nutrition support in adults. NICE Clinical Guideline 32, 2006.
CPD articles are commissioned by The Pharmaceutical Journal and are not peer reviewed.

