Jean-Denis Laredo/ ISM / Science Photo Library
Summary
Biosimilar medicines are biological medicines that have been developed to be highly similar and clinically equivalent to an existing biological medicine. The introduction of these medicines provides additional patient choice and enables financial savings. These savings can be used within the NHS to help support the use of new treatments as they become available and further develop services for patients. The NHS already has a history of using biosimilar medicines for indications such as growth hormone deficiency, neutropenia associated with chemotherapy and anaemia related to renal disease. Biosimilar infliximab is now available for the management of a number of rheumatology conditions and, in the next few years, additional biosimilar medicines will become available for rheumatology patients. The introduction of biosimilars requires careful planning, the expertise of a multidisciplinary team and effective communication. Of utmost importance is the involvement of the patient in the decision to use a biosimilar. Current NHS policy states: “The decision to prescribe a biological medicine for an individual patient, whether an originator or biosimilar medicine, rests with the responsible clinician in consultation with the patient.”
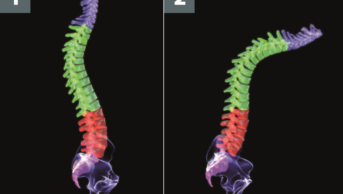
The introduction of biologic medicines, such as the tumour necrosis factor ά inhibitors (TNFi), has revolutionised the management of rheumatological diseases, including rheumatoid arthritis (RA) and the sero-negative spondyloarthropathies (ankylosing spondylitis [AS], psoriatic arthritis [PsA] and non-radiographic axial spondyloarthritis [axSpA]). These medicines block the actions of a number of inflammatory cytokines (e.g. TNFά, interleukin-1 [IL-1] and interleukin-6 [IL-6]) and immune mediators (T cells and B cells) within the body, identified as being causative factors in the joint and tissue damage associated with autoimmune and autoinflammatory diseases[1]
. The production of biologic medicines is highly complex, as they are derived from a living cell system[2]
. As a consequence, their original development was costly, resulting in high acquisition costs for commissioners. The clinical effectiveness of these medicines has been counterbalanced by the economic burden they have placed on the global health economy[3]
. The TNFi Enbrel (etanercept) alone was the world’s fifth biggest selling medicine in 2014 with sales of nearly US$9bn[4]
.
As patents for branded TNFi near their expiry, pharmaceutical manufacturers have taken steps to develop medicines with equivalent therapeutic effect to their branded counterparts, but with a considerably lower acquisition cost. These new medicines have been classified as ‘biosimilars’. NHS England defines biosimilar medicines as “a biological medicine which is highly similar to another biological medicine already licensed for use. It is a biological medicine which has been shown not to have any clinical meaningful differences from the originator biological medicine in terms of quality, safety and efficacy”[2]
. Biosimilar medicines have the potential to provide the NHS with considerable cost savings. The National Institute for Health and Care Excellence (NICE) recently proposed that the use of biosimilar infliximab could provide a 10% saving per cycle for each patient. It is important to note that biosimilars are not a generic copy of the original biological medicine (originator medicine or reference medicine) and the practice of automatic substitution is not permitted. The Medicines and Healthcare products Regulatory Authority (MHRA) recommends that all biological medicines, including biosimilars, are prescribed by brand name[2]
,[3]
.
European license approval
Biosimilar medicines have specific European Union (EU) regulatory pathways that differ from the authorisation process applied to generic medicines[2]
. The European Medicines Authority (EMA) analyses evidence provided from detailed head-to-head randomised controlled trials, which are designed to demonstrate that there are no significant differences in terms of efficacy and safety between the biosimilar product and the original reference drug. Biosimilar medicines are not required to have comparative phase III clinical trial data for all the indications of the original product. The information submitted to the EMA by the manufacturer of the biosimilar should be of sufficient quality and quantity to allow ‘extrapolation’ by the EMA to all the indications of the original reference product[2]
. All biologic medicines, whether they are the original reference product or the biosimilar, will exhibit batch-to-batch variability because of the way they are manufactured[3]
.
In the case of Remicade (infliximab), there have been 40 listed changes to the manufacturing process. For each of these changes, the same comparability process applied to the new biosimilars has also been applied to Remicade.
NICE and biosimilars
NICE is permitted to allow its recommendations, within multi-technology appraisals, to apply equally to the new marketed biosimilar medicine and the original reference drug[2]
. However, if NICE feels a review of the evidence of the new biosimilar product is required, it will produce an ‘evidence summary: new medicine’. In an evidence summary, the specific brand name of the product is stated because substitutability and interchangeability cannot be assumed. Evidence summaries do not make recommendations on which product to choose, this decision rests with the patient and the clinician caring for them. NICE recently published a final appraisal determination (FAD) on TNFi for ankylosing spondylitis and non-radiographic axial spondyloarthritis. The FAD only recommends starting infliximab if the least expensive product is used, and the biosimilar infliximab fulfils this criteria[5]
.
In July 2015, NICE produced a guidance document to assist both clinical and non-clinical staff in introducing biosimilar infliximab into NHS clinical practice[3]
. The document includes practical examples from hospitals that are already prescribing biosimilar infliximab and have successfully switched a large proportion of their inflammatory bowel disease (IBD) patients from the original reference drug to the biosimilar (see ‘Introducing biosimilar medicines into practice’).
Introducing biosimilar medicines into practice
The formation of a local project team, which includes a senior physician, pharmacist lead, management sponsor, commissioning leads and staff delivering the service, is recommended to support the safe introduction of biosimilar medicines. Communication and collaboration is essential and at the start of the process, it is important to define appropriate measures that provide assurance of safe and successful implementation of biosimilars into prescribing practice[3]
.
These measures should include consultation with all stakeholders (including patients) who will be involved and affected by the switch. Appropriate information should be sent out to both clinicians and patients, explaining what biosimilars are and the rationale for switching. Centres that have already switched patients to biosimilar infliximab developed patient information leaflets, which were sent out to patients in advance of the switch. In addition, a nurse specialist at these centres contacted patients by phone to explain the process and answer any questions. Clinical consensus on use and approval on the hospital formulary should be sought for each new biosimilar product. The formulary approval process should include recommendations on good prescribing practice of biosimilars to ensure the appropriate brand is prescribed for a patient. Hospitals that reconstitute a biosimilar product within their own preparative services will also need to ensure standard operating procedures are put in place to prevent the wrong brand of the medicine being aseptically prepared for a patient.
Considerable financial savings can be generated as a consequence of biosimilar prescribing. Prior to introduction of the biosimilar, information on the potential savings should be gathered and discussed with local commissioners in order to gain agreement on sharing financial rewards generated by the switch. Both University Hospital Southampton NHS Foundation Trust and University College London Hospitals NHS Foundation Trust have been able to develop and improve their services for IBD patients as a consequence of commissioners sharing the financial rewards generated by the switch[6]
. Both hospitals used a clinical data collection template and patient questionnaire to provide a longitudinal data set before and after switching. Patients were also registered on the IBD biologic registry.
Licensed biosimilars in rheumatology
Currently, there are two licensed biosimilar infliximab brands available in the UK; Inflectra (Hospira) and Remsima (Napp Pharmaceuticals). For a comparison of the current listed price of the two biosimilar infliximabs compared with the original reference product, see ‘Current marketed listed price for the three available brands of infliximab’. In the UK, there may be regional variations in the contract price of these products as a result of local procurement agreements with the manufacturers.
| Current marketed listed price for the three available brands of infliximab | |
|---|---|
| Product | MIMMS listed price (£) |
| Remicade 100mg (MSD) | 419.62 |
| Inflectra 100mg (Hospira) | 377.66 |
| Remsima 100mg vial (Napp Pharmaceuticals) | 377.66 |
Inflectra and Remsima are the same biosimilar product (CT-P13). CT-P13 is an IgG1 chimeric human-murine monoclonal antibody produced in the same type of recombant cell line (murine hybridoma cells produced by recombinant DNA technology) and with an identical amino acid sequence (30% murine variable amino acid sequence/70% human IgG1 heavy chain constant region and human kappa light chain). Both brands of biosimilar infliximab have the same therapeutic indications[6]
,[7]
,[8]
, pharmaceutical form and dosage regimes as the original branded Remicade. With regard to use of biosimilar infliximab in rheumatology patients, there have been two key studies: Program evaLuating the Autoimmune Disease iNvEstigational Drug cT-p13 in RA Patients (PLANETRA) and Program evaLuating the Autoimmune Disease iNvEstigational Drug cT-p13 in AS Patients (PLANETAS). Both studies used the standard dose infliximab regimes currently used in clinical practice for the management of these conditions.
The PLANETRA study was a 54-week, phase III randomised, double-blind, multicentre, multinational parallel group study designed to compare the efficacy and safety of biosimilar infliximab (CT-P13) with the original infliximab reference product (INX)[9]
. For the primary end point, CT-P13 was required to demonstrate equivalent efficacy to the reference product in terms of a 20% improvement in the American College of Rheumatology score (ACR20) at week 30. All patients entering the study had active disease and a diagnosis of RA for at least one year (1987 ACR classification criteria[5]
). All patients needed to be on a stable dose of methotrexate and must not have previously received a biologic medicine. A total of 606 patients were randomised (CT-P13 n= 302, INX n= 304) on a 1:1 basis to receive a two-hour infusion of 3mg/kg CT-P13 or INX at weeks zero, two and six, and then every eight weeks up to week 30. A total of 515 patients completed the 30-week study period and, of these, 16 patients were excluded from the patient population on account of protocol violations. The results were comparable across the two treatment groups for the ACR20 at week 30, in addition, similar results were seen for the ACR50 and ACR70 scores (see ‘PLANETRA study week 30 efficacy results in terms of ACR response’). Incidence of drug-related adverse events (35.2% versus 35.9%) and detection of anti-drug antibodies (48.4% versus 48.2%) were similar between CT-P13 and INX, respectively. Overall, no statistically significant differences in response or safety data were seen between CT-P13 and INX[9]
.
| PLANTERA study week 30 efficacy results in terms of American College of Rheumatology response | ||
|---|---|---|
| ACR = American College of Rheumatology Score (20%, 50%, 70%). | ||
| CT-P13 | INX | |
| ACR20 | ||
| Intention to treat population (n = 606) (95% CI: -6% to 10%) | 60.9% | 58.6% |
| Per protocol population (n=499) (95% CI: -4% to 12%) | 73.4% | 69.7% |
| ACR50 | ||
| Per protocol population (n=499) (95% CI: -7% to 10%) | 42.3% | 40.6% |
| ACR70 | ||
| Per protocol population (n=499) (95% CI: -5% to 9%) | 20.2% | 17.9% |
Patients who completed the PLANETRA study were eligible for entry into an open label extension phase covering an additional period of 48 weeks[6]
. Of the original study population, 302 patients entered the extension study. In this group, 158 patients were maintained on CT-P13 and 144 patients were switched from the originator reference drug (INX) to the biosimilar (CT-P13). Through to week 102, ACR20/50/70 response rates were maintained and were similar for each group: 72.2%, 48.3% and 24.5% (maintenance group) and 71.8%, 51.4% and 26.1% (switch group). Overall, the efficacy and safety profiles of the maintenance group and switch group were comparable[6]
.
The PLANETAS study was a 54-week, phase I randomised, double-blind, multicentre, multinational, parallel-group study designed to compare the pharmacokinetics, safety and efficacy of biosimilar infliximab (CT-P13) with the original reference compound (INX) in patients with AS[10]
. Eligible patients had a diagnosis of AS according to the 1984 modified New York classification criteria[11]
for at least three months prior to screening, were biologic naive and had active disease. The primary end points were area under the concentration time curve (AUC) at steady state and observed maximum steady state concentration (CMAX,SS) between weeks 22 and 30. Assessment according to the Ankylosing Spondylitis International Working Group criteria (ASAS20 and ASAS40) for improvement of 20% and 40% was performed in addition to required safety outcomes. Patients were randomly assigned on a 1:1 basis to receive either 5mg/kg of the biosimilar (CT-P13) or the original reference compound (INX) at weeks zero, two, six and then every eight weeks up to week 30. Of the 250 randomised patients, 229 completed the 30-week study period (CT-P13: n=125; INX: n=125). The pharmacokinetic parameters of AUC and Cmax were equivalent for CT-P13 (32765.8 µgh/ml and 147.0 µg/ml) and INX (31359.3 µgh/ml and 144.8 µg/ml). The ratio of geometric means was near a 100% for AUC and CMAX,SS. For the clinical response measures of ASAS20 and ASAS40, no statistically significant difference was seen between the two treatment groups at weeks 14 and 30 (see ‘Assessment according to the Ankylosing Spondylitis International Working Group criteria [ASAS20 and ASAS40] at week 30’)[7]
. Overall, at week 30 the efficacy and safety profile was similar between the two groups[10]
.
| Assessment accoriding to the Ankylosing Spondylitis International Working Group criteria (ASA20 and ASAS40) at week 30 | ||
|---|---|---|
| Week 30 | CT-P13 (n=125) | INX (n=125) |
| ASA20 (OR: 0.091; 95% CI: 0.51-1.62) | 70.5% | 72.4% |
| ASA40 (OR: 1.19; 95% CI: 0.70-2.00) | 51.8% | 47.4% |
Of the 210 patients who completed PLANETAS, 174 entered a one-year open label extension phase[12]
. Within the open label phase, 88 patients continued with CT-P13, while 86 patients were switched from INX to CT-P13. The comparable efficacy and tolerability profiles seen in the original 54-week study were maintained in the open label extension phase up to week 102[1]
.
Interchangeability
Infliximab is a monoclonal antibody that is not fully humanised and individuals exposed to this drug for a period of time will have had a specific anti-drug (B cell) response[13]
. Concerns have been raised that the immunogenic response to the biosimilar will differ from the original reference compound. Before market authorisation is granted for a biosimilar product, anti-drug B cell response must be evaluated. If the biosimilar contains the same amino acid sequence to the reference product, it should also have the same T-cell epitope. A strong immune response would require a new T-cell epitope. The level of aggregates and immunogenic impurities is also tightly controlled in biosimilar products, thus further controlling immunogenicity[13]
.
At present, there are no formal switch studies involving rheumatology patients. In both PLANETAS and PLANETRA, switching occurred in an open label extension phase in a small controlled patient population for a period of one year[6]
,[12]
. None of the patients in the controlled blinded studies had previously received a biologic medicine. Patients in ‘real life’ settings may have been on the reference product for a number of years, have additional extra-articular conditions (e.g. uveitis, psoriasis and IBD) and had exposure to multiple biologic medicines. It is not known what the potential complications could be of switching this population of patients. At the moment, there is a lack of knowledge about the long-term safety of biosimilar drugs[14]
. In February 2015, the British Society For Rheumatology (BSR) produced a position statement on biosimilar medicines[14]
. Within the statement it supported the incorporation of biosimilars into clinical practice, but the statement did not support switching patients who were currently responding and tolerating the reference product. The BSR recommends evaluating patients on an individual basis until additional safety data become available. Clinicians are encouraged to register all rheumatology patients commenced on a biosimilar product on the British Biologics Register.
A large Phase IV, randomised, double-blind, parallel group study is currently under way in Norway (NOR-SWITCH study) which aims to assess the safety and efficacy of switching from Remicade to the biosimilar treatment Remsima in patients with RA, AS, PsA, ulcerative colitis, Crohn’s disease and chronic plaque psoriasis (ClinicalTrials.gov identifier: NCT021486440). The primary outcome of the study is occurrence of disease worsening within a 52-week period. Patients entering the study must have been on stable treatment with innovator infliximab (Remicade) for the past six months. The estimated primary completion date of the study is April 2016 and it is hoped that data from this study will answer questions on the safety of switching patients who are established on the reference drug to the biosimilar.
Future biosimilars
In October 2015, the US Food and Drug Administration (FDA) accepted a biologic license application from Sandoz (a Novartis company) for a biosimilar etanercept product
[15]
. Sandoz is seeking approval for all the indications of the current reference product, Enbrel. An application to the EMA is planned for early 2016. For a summary of current biosimilars in phase III trials that are likely to become licensed for rheumatology conditions in the next few years, see ‘Biosimilar products for rheumatology indications currently in clinical development’. Licensing is prevented until the patent for the original reference drug expires.
| Biosimilar products for rheumatology indications currently in development | |||
|---|---|---|---|
| Source: New Drugs Online, UK MI information website *Launch dates are approximate RA= rheumatoid arthritis; PsA= psoriatic arthritis; AS= ankylosing spondylitis; axSpA= non-radiographic axial spondyloarthritis; JIA= juvenile idiopathic arthritis. | |||
| Biosimilar | Indication | Status | Pharmaceutical companies/manufacturer |
| Etanercept GP2015 | RA, PsA, AS, axSpA | US accepted licence application. UK launch 2017*. | Sandoz, Novartis |
| Etanercept SB4 | RA, JIA, PsA and AS | Pre-registration filed with EMA. UK launch Q1 2016*. | Biogen, Samsung Bioepsis |
| Etanercept CHS-0214 | RA | Phase III clinical trials. Estimated completion in May 2016*. | Baxter, Coherus Biosciences |
| Rituximab ABP 798 | RA | Phase III clinical trials. UK launch 2017*. | Amgen |
| Rituximab BI695500 | RA | Phase III clinical trials. UK launch 2017*. | Boehringer Ingelheim |
| Rituximab CTP10 | RA | Phase I, Phase III EU clinical trials. UK launch 2018*. | Sandoz, Celltrion |
| Rituximab MK8808 | RA | Phase I UK and EU. UK launch 2017*. | Merck Sharp & Dohme, Akebia |
| Adalimumab ABP 501 | RA | Phase III clinical trials. UK launch 2018*. | Amgen |
| Adalimumab BI-695501 | RA | Phase III US and Europe only. UK launch 2018*. | Boehringer Ingelheim |
| Adalimumab CHS-1420 | RA | Phase I. UK launch 2018*. | Coherus Biosciences |
| Adalimumab M923 | RA | Phase III clinical trials. UK launch 2018*. | Baxter |
| Adalimumab PF- 06410293 | RA | Phase III clinical trials. UK launch 2018*. | Pfizer |
| Adalimumab SB5 | RA | Phase III clinical trials. EU only. UK launch 2017*. | Samsung Bioepsis. |
Tina Hawkins
is an advanced clinical pharmacist in rheumatology at Leeds Teaching Hospital NHS Trust. Paul Emery is Arthritis Research UK professor of rheumatology and director of Leeds Institute of Rheumatic and Musculoskeletal Medicine at University of Leeds, and director of Leeds Musculoskeletal Biomedical Research Unit at Leeds Teaching Hospitals NHS Trust.
References
[1] McGonagle D & McDermott MF. A proposed classification of the immunological diseases. PLoS Medicine 2006;3(8):e297. doi:10.1371/journal.pmed.0030297
[2] NHS England. What is a Biosimilar Medicine? (Draft 8.3) Clinical and Scientific Policy and Strategy Team, NHS England, 24 September 2015. Publication Gateway Reference: 03923.
[3] National Institute for Health and Care Excellence. Health Technologies adoption programme. Introducing biosimilar versions of infliximab: inflectra and Remsima, 31 July 2015, Available at: https://www.nice.org.uk/guidance/htta329 (accessed November 2015).
[4] Medscape. Novartis Biosimilar Takes Aim At Amgen’s Enbrel. 2015.
[5] National Institute for Health and Care Excellence. Ankylosing spondylitis and axial spondyloarthritis (non-radiographic) — adalimumab, etanercept infliximab and golimumab (inc rev TA143 and TA233) ID694: final appraisal determination. 11 September 2015.
[6] Yang D-H, Prodanovic N, Jaworski J et al. Efficacy and safety of CT-P13 (infliximab biosimilar) over two years in patients with rheumatoid arthritis: Comparison between continued CT-P13 and switching from infliximab to CT-P13. Arthritis and Rheumatism 2013;65(12):3319. doi:10.1002/art.38257
[7] Electronic Datasheet Compendium. Inflectra 100mg powder for concentrate for solution for infusion. Last updated 11 June 2015. Hospira UK Limited. Available at: http://www.medicines.org.uk/emc/medicine/29980 (accessed November 2015).
[8] Electronic Datasheet Compendium. Remsima 100mg powder for concentrate for solution for infusion. Last updated 25 February 2015. Hospira UK Limited. Available at: http://www.medicines.org.uk/emc/medicine/29978 (accessed November 2015).
[9] Yoo DH, Hrycaj P, Miranda P et al. A randomised, double-blind, parallel group study to demonstrate equivalence in efficacy and safety of CT-P13 compared with the innovator infliximab when co-administered with methotrexate in patients with active rheumatoid arthritis: the PLANETRA study. Ann Rheum Dis 2013;72(10):1613–1620. doi:10.1136/annrheumdis-2012-203090
[10] Park W, Hrycaj P, Jeka S et al. A randomised, double-blind, multicentre, parallel-group, prospective study comparing the pharmacokinetics, safety, and efficacy of CT-P13 and innovator infliximab in patients with ankylosing spondylitis: the PLANETAS study. Annals of the Rheumatic Diseases 2013;72(10):1605–1612. doi:10.1136/annrheumdis-2012-203091
[11] Sieper J, Rudwaleit M, Baraliakos X et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 2009;68(2);ii1–ii44. doi:10.1136/ard.2008.104018
[12] Park W, Miranda P, Brzosko M et al. Efficacy and safety of CT-P13 (infliximab biosimilar) over two years in patients with ankylosing spondylitis: Comparison between continuing with CT-P13 and switching from infliximab to CT-P13. Arthritis and Rheumatism 2013;65(12):3326. doi:10.1002/art.38257
[13] Pekka K. Biosimilars for prescribers. Generics and Biosimilars Initiative Journal 2015:4(1):33–35. doi:10.5639/gabij.2015.0401.008
[14] British Society for Rheumatology Position statement on biosimilar medicines. February 2015. Available at: http://www.rheumatology.org.uk/about_bsr/press_releases/bsr_supports_the_use_of_biolsimilars_but_recommends_measures_to_monitor_safety.aspx (accessed November 2015).
[15] US Food and Drug Administration. US Department of Health and Human Services. Available at: www.fda.gov (accessed November 2015).