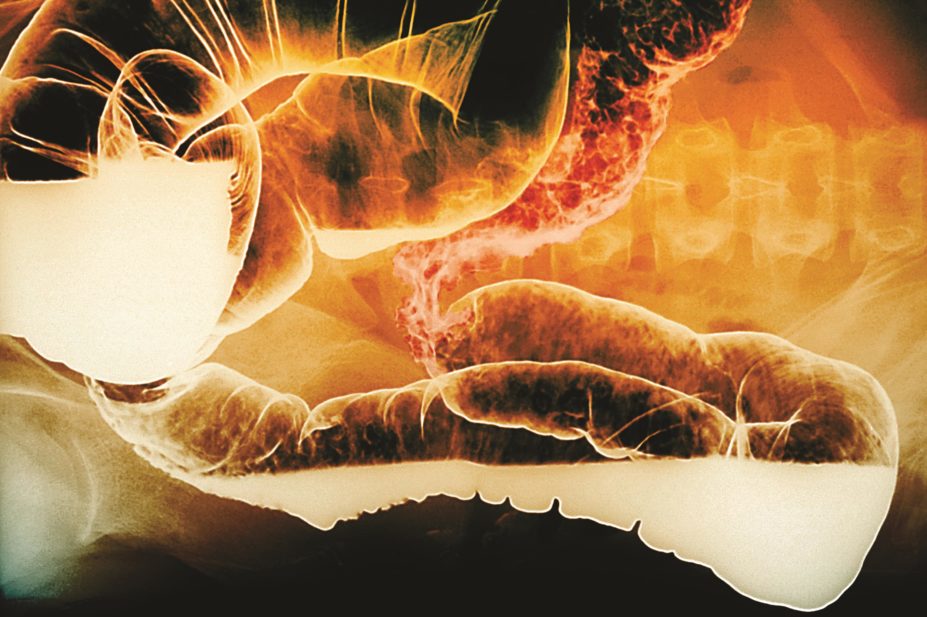
Zephyr / Science Photo Library
Biological medicines are large, complex proteins comprised, or derived from, living cells or organisms[1]
. The biologic infliximab is a chimeric human–murine monoclonal antibody that is produced using recombinant DNA technology[2]
. It acts against tumour necrosis factor alpha (TNF-α), a pro-inflammatory cytokine, and is used for the management of several autoimmune diseases (e.g. inflammatory bowel disease [IBD]). Infliximab was the first biologic to be used in the management of IBD in 1999 and is now key in the management of both Crohn’s disease (CD) and ulcerative colitis (UC).
When the patents for biologic medicines expire, many biotechnology companies develop and manufacture biosimilars of the original biologic medicines. However, biologic molecules have a complex structure and the process to produce them from living cells is unique to the manufacturer[3]
. Any changes in the production site or manufacturing process can affect the structure of a biologic[1]
. Therefore, the new biologic molecule will be highly similar to the original biologic but not identical, hence the name biosimilar.
Biosimilars introduced into the UK market are authorised by the European Medicines Agency (EMA). The development of biosimilar medicines improves patient and clinician choice and increases commercial competition[3]
. However, the development of biosimilars is not to establish patient benefit per se (which has already been shown for the reference product)[3]
, but to demonstrate high similarity to the reference product so that the efficacy and safety experience gained with its use can be extrapolated to the biosimilar version.
In June 2013, the first biosimilar monoclonal antibody (biosimilar infliximab, CT-P13) was approved by the EMA and marketed under the trade names Remsima[4]
and Inflectra[5]
.
The regulation of biosimilars
A biosimilar medicine is one that is highly similar to a biologic that is already authorised for use in the European Economic Area (EEA)[6]
. Although the active substance of a biosimilar and its reference medicine is essentially the same in physiochemical and biological terms, there will be a degree of natural variability in molecular structure between the biosimilar and the original biologic. Minor levels of variation are also found between batches of the original biologic product following a manufacturing change[3]
. Any variability between batches of originator biologic or between the originator biologic and its biosimilar is controlled and maintained within predefined and EMA-approved equivalence limits, and must be shown not to affect safety or effectiveness[3]
.
Biosimilars undergo a comprehensive regulatory process with extensive head-to-head comparability studies to demonstrate similarity to the reference medicine[3]
. The EMA requires the biosimilar to have a highly similar quality profile, as well as comparability data from both non-clinical studies (e.g. pharmacological and toxicological assessment) and clinical studies (e.g. pharmacokinetic and pharmacodynamic studies, and clinical efficacy and safety trials)[6]
. CT-P13, for example, had physiochemical tests to compare its molecular structure to originator infliximab and functional assays to compare biological characteristics[7]
. The purpose of clinical data is to provide complementary information, for example, the clinical relevance of any observed differences and data on immunogenicity. Any observed differences have to be justified with regard to their potential impact on safety and efficacy[6]
. For example, there have been 40 listed changes made to the manufacturing process for Remicade (originator infliximab) since 1999 and the same comparability exercise is carried out to ensure that the new Remicade is similar to the previous one. All major physiochemical characteristics and biological activities of CT-P13 have been shown to be comparable to those of Remicade.
Extrapolation of evidence for CT-P13
CT-P13 has been approved for the same indications as the originator infliximab (Remicade) using data from two randomised, controlled, double-blind clinical trials in rheumatoid arthritis (RA, the Programme evaLuating the Autoimmune disease iNvEstigational drug cT-p13 in RA patients [PLANETRA] study)[8]
and ankylosing spondylitis (AS, the Programme evaLuating the Autoimmune disease iNvEstigational drug cT-p13 in AS patients [PLANETAS] study)[9]
, which demonstrated equivalent outcomes between CT-P13 and Remicade. Controlled trials of CT-P13 were not undertaken in CD or UC. The EMA licence for the use of CT-P13 in IBD was granted on the basis of extrapolation from the rheumatology data. The working party on similar biologic medicinal products of the EMA stress that a biosimilar cannot automatically claim all indications of the reference product and that extrapolation will only be approved on the basis of sound scientific justification[7]
.
Immunogenicity is related to multiple factors including, among others, the route of administration, dose regimen, and patient and disease-related factors. Thus, immunogenicity could differ among indications. Extrapolation of immunogenicity from the studied indication/route of administration to other uses of the reference product should be justified[6]
.
Pharmacovigilance
There are no specific efficacy or safety concerns identified for biosimilar medicines, however, as new medicines, biosimilars have ‘black triangle’ status and any suspected adverse reactions should be reported through the Medicines and Healthcare products Regulatory Agency (MHRA) Yellow Card Scheme in order to further characterise immunogenic potential and adverse reactions[10]
.
In the UK, the MHRA recommends that all biological medicines and biosimilars are prescribed by brand and generic name[11]
, to ensure that the intended product is received by the patient. This can be supported by electronic prescribing systems. The MHRA also supports the recording of brand names and batch numbers in patient records, for traceability when reporting suspected adverse reactions[12]
. Every biosimilar medicine authorised in the EU will have a risk management plan and information on this is included in the European Public Assessment Report (EPAR)[13]
. Robust pharmacovigilance is essential for any new biologic, and patients on a biologic or the biosimilar should be followed up for safety in a registry[14]
(e.g. the UK national IBD registry) to support the gathering of intelligence and experience.
Managing the introduction of biosimilars: insight from the NHS
The National Institute for Health and Care Excellence (NICE), England’s health technology assessment body, has worked with two NHS organisations to share their learning and experiences of planning for and managing the introduction of biosimilar medicines. The knowledge gained is presented as technology appraisal adoption support for introducing biosimilar versions of infliximab, Inflectra and Remsima[15]
. Box 1 presents the University of Southampton experience, and while it is not presented as best practice, it does provide a real-life clinical example, including the planning and management of the introduction of biosimilars.
Box 1: The University Hospital Southampton NHS Foundation Trust experience of switching inflammatory bowel disease patients from Remicade to the biosimilar Inflectra
Background
The British Society of Gastroenterology (BSG) recommends that for patients starting infliximab, Remicade, Remsima or Inflectra can be prescribed. The choice of preparation should take into account the cost of the drug and its administration. In addition, the BSG states that there is sufficient evidence to recommend that patients who are in a stable clinical response or remission on Remicade therapy can be switched to Remsima or Inflectra at the same dose and dose interval[14]
.
The clinicians within the gastroenterology team at University Hospital Southampton (UHS) discussed the use of biosimilars and agreed to the switching of their inflammatory bowel disease (IBD) patients on Remicade to CT-P13. The formulary approval of CT-P13 was then obtained.
Methodology
With the support of the Trust’s assistant director of finance, a gain share with the two local clinical commissioning groups (CCGs) was agreed for the managed switch to CT-P13. Through the gain share, a proportion of the substantial drug acquisition savings have been reinvested into the IBD service, including the funding of a specialist biologic pharmacist.
The proposed switching programme from Remicade to CT-P13 was discussed with the IBD patient panel. Many of the patients on the panel were on infliximab or other biologics and were able to offer insight from the patient perspective. The patient panel were reassured by the additional clinical monitoring and surveillance to be included within the programme and they were pleased that some of the savings were being reinvested to improve their care.
During clinic appointments the switch to biosimilar infliximab was discussed with those IBD patients on Remicade. In addition, the IBD nurse spoke to all (n=143) of the Remicade IBD patients (more than 80% of whom had CD) during one of their routine Remicade infusions. Patients were also given a letter that explained the proposed switch to CT-P13 (Inflectra); a copy letter was also sent to patients’ GPs. All patients received a follow-up phone call before their next infusion date to ensure they understood the process. Patients were informed that they could call the hospital IBD helpline at any time if they had concerns. They were also reassured that their infliximab would be changed back to Remicade in the unlikely event that it became clinically necessary (e.g. if they experienced adverse effects or loss of disease control).
All patients on Remicade were asked to complete a questionnaire at the two infusions before their planned switch. This included a patient-recorded outcome measure (PROM) for IBD control[28]
, disease activity scoring (IBD-Control-VAS score) and a questionnaire on side effects experienced. Routine blood tests for biochemical markers of disease activity were also done. Adverse events were reported using the Yellow Card Scheme. Patient serum was collected prior to the switch for the measurement of infliximab trough levels and antidrug antibody levels. The serum infliximab trough levels and antidrug antibodies are an important predictor of loss of response and immunogenicity and were measured using the Immundiagnostik IDK monitor ELISA assay.
The switch programme started in April 2015 and required close collaboration between the clinical speciality staff, the biologics pharmacist, the day unit staff and the patients.
As an independent prescriber, the pharmacist prescribed the majority of CT-P13 prescriptions for the first three months of the programme. As part of the risk management strategy, a robust drug traceability system was put in place in the day infusion unit, as well as on the wards where in-patients may receive infliximab. The pharmacist worked with the IT team to amend the hospital electronic prescribing system so that all biologics could only be prescribed by brand name. Additionally, the protocol required the brand name and batch number of the infliximab vials used to be recorded in patient records and for all patients to be given the brand-specific biologic alert card.
Results
After two months, all 143 patients had been switched from Remicade to CT-P13, at the same dose and with the same frequency. The median number of Remicade infusions administered prior to switching was 10 (range 1–67). Some patients had only recently started Remicade prior to the switch, however, the majority of patients were in remission and had been on stable maintenance Remicade therapy. During the switch programme any new patients requiring infliximab were initiated on CT-P13. After 12 months, patients had received a median of seven Inflectra infusions (range 1–9). Two patients had requested a review of the switch; one patient was on concomitant mercaptopurine and had abnormal liver enzymes with high 6-thioguanine and 6-methylmercaptopurine levels and the second patient had non-specific flu-like symptoms. All patients continued to have their routine six-monthly clinical reviews in line with the protocol and in addition to the switch programme evaluations.
Patient reported outcomes, disease activity scores, laboratory results and side effects were collected prospectively at each subsequent infusion following the switch and reviewed by the team as part of a risk management strategy. Additionally, drug and antidrug antibody levels were measured once patients had received three infusions of CT-P13.
The evaluation outcomes of the switch programme include drug persistence, change in drug spend, patient reported side effects, adverse events and patient outcomes assessed using the IBD control-8 PROM and blood tests including CRP, platelet count, haemoglobin and albumin.
In order to assess drug persistence, the treatment outcomes of IBD patients on Remicade during the period April 2014 to March 2015 were compared with the outcomes of patients treated with CT-P13 during the period April 2015 to March 2016. If a patient stopped treatment, the reason for stopping was obtained from the patients’ records. The gain share incentivised us to switch all patients to CT-P13 in one go. However, maintaining a control group of IBD patients on Remicade during the switch programme would have enabled a more robust evaluation of switching to CT-P13 to continued use of Remicade.
All patients treated with at least one dose of CT-P13 were included in the safety analysis. Outcomes were analysed in patients who provided relevant data at the time of the switch from originator to CT-P13 and after at least three infusions of CT-P13.
At one year (April 2015 to March 2016), there were no clinically significant differences in terms of drug persistence, side effects, adverse reactions, disease activity (IBD-Control-VAS score) or blood test results between the two infliximab products. It is worth noting that patients were more closely monitored following the switch and, therefore, had greater opportunity to report side effects. There was an improvement in the mean IBD control-8 score following the switch to CT-P13. This improvement may have been influenced by the increased IBD specialist nursing support. There were no significant differences in the infliximab trough levels before and after the switch, and anti-drug antibody positivity was unchanged at 40% before and after the switch.
The potential effect of concomitant immunomodulator therapy (70.7% of patients in the switch programme) versus infliximab monotherapy on patient outcome, when switching from Remicade to CT-P13, was not evaluated.
The financial impact of the switch was a reduction in infliximab acquisition costs of around £60,000 per month.
Considering the relative short clinical experience of using CT-P13 in IBD and the extrapolation of data by the EMA, close monitoring and follow-up of this group of patients is recommended. All of the IBD patients receiving a biologic or biosimilar are entered onto the local gastroenterology database and the UK IBD Registry. The registry contributes to the body of evidence on biosimilars.
Conclusion
In this study, IBD patients were successfully switched from Remicade to CT-P13 in a real life NHS environment. The gain share enabled a proportion of the savings to be reinvested into the clinical service for IBD patients.
The current evidence base
There is a growing body of real-world evidence showing the comparable safety, clinical efficacy and immunogenicity of CT-P13 in both treatment-naïve patients and patients who have been switched from Remicade to CT-P13[12]
.
Studies by Keil et al.
[16]
, Jahnsen et al.[17]
and Farkas et al.[18]
all showed that induction therapy with CT-P13 in CD and UC is safe and effective. A prospective, multicentre cohort (210 patients) showed that CT-P13 was safe and effective in the induction of clinical remission and response in both CD and UC[19]
.
Two reports from Korea provide data of patients with IBD switching to CT-P13. The first included 173 patients (CD=95, UC=78)[20]
, while the second reported 59 CD patients (27 switching from Remicade) and 51 UC patients (nine switching from Remicade)[21]
. Both demonstrated high response and remission rates.
In 2015, Kang and colleagues reported effective induction with CT-P13 in 17 IBD patients[22]
. Nine patients in maintenance with the originator were interchanged with CT-P13 (UC=4 and CD=5). One UC patient experienced arthralgia and one patient experienced loss of response. However, a study by Smits and colleagues in 83 IBD patients demonstrated that switching from Remicade to CT-P13 did not have significant impact on short-term clinical outcomes[23]
. Furthermore, a study by Kolar et al. that included 74 IBD patients found comparable efficacy, safety and immunogenicity after switching patients from reference infliximab to CT-P13[24]
.
Data from the PRospective Observational cohort Study with Inflammatory bowel disease receiving Therapy with BIOsimilars (PROSIT-BIO; n=397), showed that patients who were switched from reference infliximab to biosimilar infliximab (n=93) demonstrated comparable efficacy and safety to patients receiving a biosimilar who had previously been naive to anti-TNF (n=217), and to patients receiving a biosimilar who had previously been exposed to one or more biologics (n=87)[25]
.
A poster presentation on this PROSIT-BIO cohort reported no difference in safety, however, after the switch, an increase in loss of response and a trend towards more frequent primary failure was observed in UC compared with CD patients. However, the results should be interpreted with caution due to the short follow-up.*
Furthermore, the extension studies of PLANETAS and PLANETRA have investigated the efficacy and safety of maintenance treatment with CT-P13 over two years, as well as the efficacy and safety of switching to CT-P13 from Remicade for one year. Clinical efficacy, immunogenicity and safety were highly comparable between the maintenance and switch group in both extension studies.
Ongoing and future research
Ongoing studies include a randomised, double-blind, parallel group, Phase III study (NCT 02096861), sponsored by Celltrion, that plans to demonstrate non-inferiority in efficacy and safety of CT-P13 compared with Remicade in patients with active CD up to week 54. The study is due to complete in February 2017. The Personalized Anti-TNF Therapy in Crohn’s Disease (PANTS) study will report UK experience of CT-P13 in CD, providing important post-authorisation data on efficacy, safety and pharmacokinetics in both anti-TNF naive patients and patients switched from Remicade.
The Nor-Switch study, is a Phase IV study evaluating the clinical safety and efficacy of switching from Remicade to CT-P13 compared with continued treatment with Remicade in patients who have been on stable infliximab treatment for at least six months. Patients with RA, psoriatic arthritis, plaque psoriasis, spondyloarthritis, UC and CD have been recruited from multiple centres in Norway[26]
. The primary study outcome is disease worsening over 52 weeks of follow-up. This study is expected to complete in January 2017.
A recent study in patients with RA and spondyloarthritis showed that when antibodies develop to Remicade they also cross-react with CT-P13[27]
. This suggests that where infliximab is ineffective owing to the presence of circulating antibodies, switching to its biosimilar is not appropriate. It is also worth noting that multiple biosimilars of the same reference product are in development. Regulatory approval processes are not expected to assess their comparability to each other. Therefore, at present, there is no evidence to support the use of biosimilars interchangeably.
Further observational studies, randomised trials and pharmacovigilance data are required within the area of immunogenicity and interchangeability for biosimilars in IBD.
Financial and conflicts of interest disclosure:
The author has worked on advisory boards for Pfizer, Abbvie, Chugai, Napp and Novartis. The author has no other relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilised in the production of this manuscript.
Acknowledgements:
The author would like to mention the team involved in the University Hospital Southampton Switch Programme Evaluation: F Cummings, I Ahmed, J Callaghan, S Whiteoak, V Razanskaite, M Rush, M Bettey and L Downey.
*As this is a rapidly developing field, the details of the poster presentation referred to in the section. ‘The current evidence base’ are: Florino G, Manetti N, Variola A et al. (March 2016) Prospective observational study on inflammatory bowel disease patients treated with infliximab biosimilars: preliminary results of the PROSIT-BIO cohort of the IG-IBD. Poster presented at European Crohn’s and Colitis Organisation Congress, Amsterdam 16–19 March 2016. Available at: https://www.ecco-ibd.eu/index.php/publications/congress-abstract-s/abstracts-2016/item/p544-prospective-observational-study-on-inflammatory-bowel-disease-patients-treated-with-infliximab-biosimilars-preliminary-results-of-the-prosit-bio-cohort-of-thex00a0ig-ibd.html
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Weise M, Bielsky M-C, De Smet K et al. Biosimilars: what clinicians should know. Blood 2012;120(26):5111–5117. doi: 10.1182/blood-2012-04-425744
[2] Electronic Medicines Compendium. Available at: http://www.medicines.org.uk/emc (accessed August 2016)
[3] National Institute for Health and Care Excellence: Biosimilar Medicines. 26 Feb 2016. Available at: https://www.nice.org.uk/guidance/ktt15/resources/biosimilar-medicines-58757954414533 (accessed August 2016)
[4] European Medicines Agency. Committee for Medicinal Products for Human Use (CHMP). Assessment report, Remsima. 27 June 2013. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002576/WC500151486.pdf (accessed August 2016)
[5] European Medicines Agency. Committee for Medicinal Products for Human Use (CHMP). Assessment report, Inflectra. 27 June 2013. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002778/WC500151490.pdf (accessed August 2016)
[6] European Medicines Agency. Committee for Medicinal Products for Human Use (CHMP). Guideline on similar biological medicinal products containing biotechnology-derived proteins as active substance: non clinical and clinical issues. 18 December 2014. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2015/01/WC500180219.pdf (accessed August 2016)
[7] European Medicines Agency. Committee for Medicinal Products for Human Use (CHMP). Guideline on similar biological medicinal products. 23 October 2014. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/10/WC500176768.pdf (accessed August 2016)
[8] Yoo DH, Hrycaj P, Miranda P et al. A randomised, double-blind, parallel-group study to demonstrate equivalence in efficacy and safety of CT-P13 compared with innovator infliximab when coadministered with methotrexate in patients with active rheumatoid arthritis: the PLANETRA study. Ann Rheum Dis 2013;72(10):1613–1620. doi: 10.1136/annrheumdis-2012-203090
[9] Park W, Hrycaj P, Jeka S et al. A randomised, double-blind, multicentre, parallel-group, prospective study, comparing the pharmacokinetics, safety, and efficacy of CT-P13 and innovator infliximab in patients with ankylosing spondylitis: the PLANETAS study. Ann Rheum Dis 2013;72(10):1605–1612. doi: 10.1136/annrheumdis-2012-203091
[10] Drug Safety Update. The black triangle scheme. June 2009. Available at: https://www.gov.uk/drug-safety-update/the-black-triangle-scheme-or (accessed August 2016)
[11] Drug Safety Update. Biosimilar products. Feb 2008;1(7):8. Available at: http://www.bsg.org.uk/clinical/news/bsg-guidance-on-the-use-of-biosimilar-infliximab-ct-p13-in-ibd.html (accessed August 2016)
[12] Drug Safety Update. Reporting suspected adverse drug reactions to vaccines and biological medicines. November 2012. Available at: https://www.gov.uk/drug-safety-update/reporting-suspected-adverse-drug-reactions-to-vaccines-and-biological-medicines (accessed August 2016)
[13] European Medicines Agency. European Public Assessment report (EPAR) Inflectra (Infliximab). Available at: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002778/human_med_001677.jsp&mid=WC0b01ac058001d124 (accessed August 2016)
[14] British Society of Gastroenterology Guidance on the use of biosimilar iInfliximab CT-P13 in inflammatory bowel disease. February 2016. Available at: http://www.bsg.org.uk/clinical/news/bsg-guidance-on-the-use-of-biosimilar-infliximab-ct-p13-in-ibd.html (accessed August 2016)
[15] National Institute for Health and Care Excellence. Infliximab, adalimumab and golimumab for treating moderately to severely active ulcerative colitis after the failure of conventional therapy. Available at: https://www.nice.org.uk/guidance/ta329/resources/nice-technology-appraisal-adoption-support-for-introducing-biosimilar-versions-of-infliximab-inflectra-and-remsima-493818736/chapter/4-insights-from-the-nhs-managing-the-introduction-of-biosimilar-medicines (accessed August 2016)
[16] Keil R, Wasserbauer M, Zadorova Z et al. Clinical monitoring: infliximab biosimilar CT-P13 in the treatment of Crohn’s disease and ulcerative colitis. Scand J Gastroenterol. 2016;51(9):1062–1068. doi: 10.3109/00365521.2016.1149883
[17] Jahnsen J, Detlie TE, Vatn S et al. Biosimilar infliximab (CT-P13) in the treatment of inflammatory bowel disease: a Norwegian observational study. Expert Rev Gastroenterol Hepatol. 2015;9 Suppl 1:45–52. doi: 10.1586/17474124.2015.1091308
[18] Farkas K, Rutka M, Balint A et al. Efficacy of the new infliximab biosimilar CT-P13 induction therapy in Crohn’s disease and ulcerative colitis – experiences from a single center. Expert Opin Bio Ther 2015;15(9):1257–1262. doi: 10.1517/14712598.2015.1064893
[19] Gecse KB, Lovasz BD, Farkas K et al. Efficacy and safety of the biosimilar infliximab CT-P13 treatment in inflammatory bowel disease: a prospective, multicentre nationwide cohort. J Crohns Colitis 2016;10(2):133–140. doi: 10.1093/ecco-jcc/jjv220
[20] Park SH, Kim YH, Lee JH et al. Post-marketing study of biosimilar infliximab (CT-P13) to evaluate its safety and efficacy in Korea. Expert Rev Gastroenterol Hepatol 2015;9 Suppl 1:35–44. doi: 10.1586/17474124.2015.1091309
[21] Jung YS, Park DI, Kim YH et al. Efficacy and safety of CT-P13, a biosimilar of infliximab, in patients with inflammatory bowel disease: a retrospective multicenter study. J. Gastroenterol Hepatol 2015;30(12):1705–1712. doi: 10.1111/jgh.12997
[22] Kang YS, Moon HH, Lee SE et al. Clinical experience of the use of CT-P13, a biosimilar to infliximab in patients with inflammatory bowel disease: a case series. Dig Dis Sci. 2015;60(4):951–956. doi: 10.1007/s10620-014-3392-z
[23] Smits LJ, Derikx LA, de Jong DJ et al. Clinical outcomes following a switch from Remicade to the biosimilar CT-P13 in inflammatory bowel disease patients: a prospective observational cohort study. Abstract. J Crohns Colitis. 2016; April 19 2016. doi: 10.1093/ecco-jcc/jjw087
[24] Kolar M, Duricova D, Brotlik M et al. (2016) ‘DOP032 Switching of patients with inflammatory bowel disease from originator infliximab (Remicade) to biosimilar infliximab (Remsima) is effective and safe.’ Abstract presented at 11th Congress of ECCO, 16–19 March, Amsterdam, Netherlands.
[25] Fiorino G et al. Prospective observational study on safety and efficacy of infliximab biosimilar in patients with inflammatory bowel disease: preliminary results of the PROSIT-BIO cohort. Presented at the Italian Group for the Study of IBD (IG-IBD), VII National Congress, Palermo, Italy. Available at: http://www.biosimilardevelopment.com/doc/newly-presented-largest-real-world-effectiveness-reference-0001 (accessed August 2016)
[26] The NOR-SWITCH study. ClinicalTrials.gov. Identifier NCT02148640. Available at: https://clinicaltrials.gov/ct2/show/NCT02148640 (accessed August 2016)
[27] ‘Biosimilar switching not suitable for all patients.’ Reported at the European League against Rheumatism Annual Congress (EULAR 2016). Available at: https://www.sciencedaily.com/releases/2016/06/160609115433.htm (accessed August 2016)
[28] Bodger K, Ormerod C, Shackcloth D, Harrison M; IBD Control Collaborative. Development and validation of a rapid, generic measure of disease control from the patient’s perspective: the IBD-control questionnaire. Gut. 2014;63(7):1092–1102. doi: 10.1136/gutjnl-2013-305600


