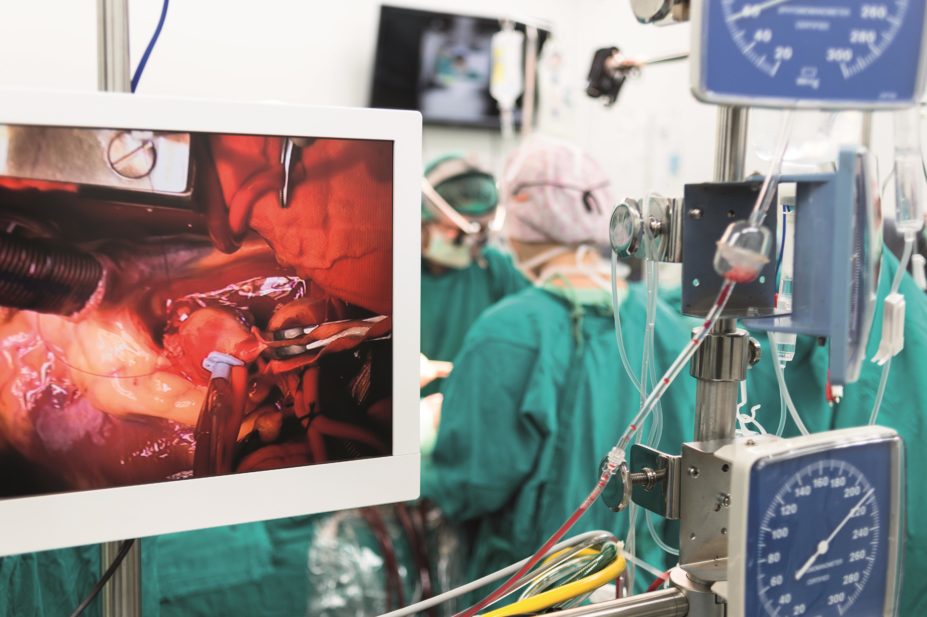
ChaNaWiT / Shutterstock.com
More than 34,000 cardiac operations are performed in the UK each year[1]
. Following heart surgery, patients typically stay in hospital for up to a week and require ongoing support from a cardiac rehabilitation team following discharge.
Patients are at risk of developing a range of complications and require a range of medicines in both the short and long term to ensure their operation is a success. This article focuses on aftercare following coronary artery bypass graft (CABG) or valve surgery.
Cardiac surgery
CABG is the most common cardiac operation in the UK, accounting for 16,000 operations in the UK in 2012[1]
. This involves isolating an artery from the patient’s arm or chest wall, or vein from the leg, and using it to bypass a narrowed or blocked coronary artery.
Valve repair and replacement is another common heart operation. Valve surgery typically involves either repair or replacement of a leaky (regurgitation) or narrowed (stenosis) mitral or aortic valve. Replacement valves can be either biological (for example, pig heart valves) or mechanical.
There are several techniques that can be used to perform the surgery. Open heart surgery involves the sternum being cut open (a median sternotomy) to allow access to the heart. Patients are usually placed on a cardiopulmonary bypass (CPB) machine, which temporarily takes over the functions of the heart and lungs while allowing the surgeon to work on a still heart. During the surgery, patients are mechanically ventilated and hypothermia is induced to prevent cerebral ischaemic injury. Cardiac surgery can also be performed without CPB, which is called ‘off-pump’ heart surgery.
An alternative approach is minimally invasive surgery. This involves creating a keyhole opening to access the heart, therefore avoiding the need to perform a medium sternotomy. This method is less invasive, allows faster recovery and causes less blood loss.
Early post-operative care
The initial management of patients following cardiac surgery focuses on ensuring adequate analgesia and ventilation and managing bleeding and hypothermia.
Maintaining cardiac output is important because it affects mean arterial pressure and tissue perfusion. Reduced tissue perfusion can lead to organ failure. Low cardiac output following cardiac surgery is managed by giving intravenous fluid therapy to increase and optimise preload, which increases the volume of each stroke and hence output. Inotropes, given by a central venous catheter, may be started when fluid therapy fails to provide an adequate effect.
Typically mechanical ventilation will be reduced and ended within 24 hours following surgery. Chest tubes, which are inserted during cardiac operations to drain fluid from the chest cavity, are removed when drainage volume is minimal (for example, several consecutive zero readings); this usually occurs the day after the operation. Central venous catheters, arterial lines and urinary catheters inserted during surgery are also removed during the initial recovery period.
Patients are given a course of antibiotics as prophylaxis for the first 24 hours after surgery. This is typically a combination of intravenous flucloxacillin and gentamicin to cover both Gram-positive and Gram-negative organisms[2]
. The choice and dose regimen of antibiotics can vary considerably between cardiac centres.
Aspirin 75mg daily is started following CABG for secondary prevention and to improve patency of vein grafts[3]
. Studies have shown that the earlier it is given after the operation, the better the benefit. Typically it is given within 24 hours after surgery[4]
. There is no strong evidence to support the use of aspirin following arterial grafts[5]
.
Clopidogrel is not usually used to improve vein graft patency, as the CASCADE (Clopidogrel after Surgery for Coronary Artery Disease) trial demonstrated that dual antiplatelet therapy with clopidogrel and aspirin did not significantly reduce vein graft hyperplasia following CABG compared with aspirin alone[6]
. However, clopidogrel can be used for patients who do not tolerate aspirin[3]
.
Patients who have had a mechanical valve implanted require lifelong anticoagulation to prevent valve thrombosis. Heparin will be started shortly after surgery and ‘bridged’ with an oral anticoagulant, usually warfarin, to protect the patient from valve thrombosis while the oral anticoagulant is reaching therapeutic levels. Therapeutic doses of low molecular weight heparins are used in practice as an alternative to unfractionated heparin, although they are unlicensed for this indication.
The target INR is dependent on patient risk factors, thrombogenicity of the prosthesis used[7]
and the position of the valve that was replaced; mitral valve replacement poses greater risk of thrombosis than aortic valve replacement.
Table 1. INR targets for mechanical valves[8]
| Prosthesis thrombogenicity | INR if no risk factors | INR with risk factors |
|---|---|---|
| Low | 2.5 | 3.0 |
| Medium | 3.0 | 3.5 |
| High | 3.5 | 3.5 |
Prosthesis thrombogenicity:
Low: Carbomedics (aortic position), Medtronic Hall, St Jude Medical (without silzone)
Medium: Bjork-Shiley, other bileaflet valves
High: Starr-Edwards, Omniscience, Lillehei-Kaster
Patient-related risk factors for thrombosis: Mitral, tricuspid or pulmonary position; previous arterial thromboembolism; atrial fibrillation; left atrium diameter >50 mm; mitral stenosis of any degree; left ventricular ejection fraction <35%; left atrial dense spontaneous echo contrast.
Complications of surgery
Atrial fibrillation (AF) is common after cardiac surgery, and typically occurs two to four days after the operation[9]
. The incidence is around 30% after CABG, and 40% after valve surgery; for combined CABG and valve procedures it is as high as 50%[9]
. Most patients will convert spontaneously back to sinus rhythm in 24 hours[9]
. Beta blockers (other than sotalol[10]
) are used to reduce the risk of AF [3],[11]
. Patients on pre-existing beta blockers should be advised to continue up to the day of surgery[9],[10]
, and beta blockers should be initiated soon after the procedure. Statins have also been shown to lower the risk of post-operative AF by between 22% and 34%[9]
, it has been postulated that this is due to their anti-inflammatory and anti-oxidative properties[11]
.
The European Society of Cardiology (ESC) guidelines recommend ventricular rate control for patients who develop AF following surgery, or direct current cardioversion for patients with AF and haemodynamic instability[9]
. Anticoagulants are started if AF persists for more than 48 hours[9]
.
Patients recovering from surgery may also have temporary epicardial pacing wires placed in-situ, which help detect and treat post-operative arrhythmias. The choice of whether to use a pacing wire depends on the surgeon.
Stroke occurs in up to 5% of patients following CABG and 16% of patients following valve surgery[12]
. Risk factors for stroke include a history of carotid artery stenosis or transient ischaemic attack (TIA)[3]
.
Surgical teams may request carotid duplex ultrasound scanning before a cardiac operation to assess stroke risk, and a carotid endarterectomy (a surgical operation to remove fatty deposits in the carotid artery) may be performed to reduce the risk of post-operative stroke[3],[13]
.
Mediastinitis, or infection of the sternal wound, occurs in up to 5% of patients[14]
. It is normally detected within two weeks of surgery, although it can occur more than a month later. Treatment includes surgical debridement, sternal rewiring, intravenous antibiotics, and vacuum assisted closure (VAC) therapy which uses negative pressure to promote wound healing.
Recovery
The average length of hospital stay for patients recovering from cardiac surgery ranges from five to seven days. During this time, physiotherapy will be provided to encourage early mobilisation. Patients will be taught deep breathing and coughing techniques to ensure adequate oxygenation and secretion of mucus to prevent respiratory tract infection. Patient-controlled analgesia with opioids via an infusion pump is gradually stopped and patients can be prescribed oral pain relief if required.
After discharge, patients are invited to attend their local cardiac rehabilitation centre. These centres provide exercise programmes and educational sessions.
Ongoing therapy
Aspirin has been shown to increase survival rates in atherosclerotic disease, which is common in patients requiring CABG surgery. Clopidogrel and aspirin are continued for 12 months as dual therapy following CABG for patients with acute coronary syndrome[4],[5]
.
Statins have also been shown to reduce mortality and cardiovascular events when started soon after CABG surgery[15]
. Pharmacists should advise patients on the benefits of statins after cardiac surgery because atherosclerosis can continue to develop after revascularisation.
Furosemide is commonly prescribed for fluid retention, which often occurs due to the large volumes of fluid used during CPB surgery[16]
. A patient’s weight will be monitored regularly before and after surgery, and once the patient’s pre-operative weight is reached the diuretic is stopped.
Prophylactic antibiotics are no longer recommended before dental procedures to prevent infective endocarditis[17]
. This also applies to procedures of the upper and lower gastrointestinal tract, genitourinary tract (including urological, gynaecological and obstetric procedures), upper and lower respiratory tract (including ear, nose, throat procedures, and bronchoscopy)[17]
.
In cases where antibiotics are prescribed because there is a suspected infection at the site of gastrointestinal or genitourinary surgery, an antibiotic that covers infective endocarditis organisms should be chosen[17]
, such as eamoxicillin or vancomycin to cover enterococci[18]
.
Patients with valve replacements are at increased risk of endocarditis. These patients should be informed of the risk, counselled on the importance of maintaining good oral hygiene and advised to seek medical attention promptly if symptoms suggestive of infective endocarditis occur (for example, fever with loss of appetite and weight loss)[18]
.
Community pharmacy
Community pharmacists can support patients following cardiac surgery by reviewing their medicines and providing advice on the signs and symptoms that may require medical attention.
Pharmacies that provide INR monitoring should ensure patients are aware of the importance of regular INR monitoring, particularly in the first month following a mechanical valve implant, when the risk of thrombosis is highest[7]
. Patients will have their INR checked daily in hospital, and patients are only discharged when the INR is in or close to the target range. The frequency of INR monitoring depends on the patient’s INR and other factors, such as interacting medicines.
Pharmacists should also ask any patient changing from warfarin to a new oral anticoagulant whether they have a prosthetic valve. Dabigatran is contraindicated in patients with a prosthetic heart valve[19]
, while apixaban and rivaroxaban are unlicensed as there are no data to support their use[20]
[21]
.
Anna Man MPharm, MRPharmS, PGDipGPP, MSc Pharmacy Practice is a cardiothoracic critical care pharmacist at Essex Cardiothoracic Centre, Basildon & Thurrock University Hospitals NHS Foundation Trust.
References
[1] The Society for Cardiothoracic Surgery in Great Britain & Ireland. Blue Book Online. www.bluebook.scts.org/#ActivityRates (accessed 2 October 2014).
[2] Kappeler R, Gillham M & Brown N. Antibiotic prophylaxis for cardiac surgery. Journal of Antimicrobial Chemotherapy 2012;67:521–522.
[3] Wijns W, Kolh P, Danchin N et al. Guidelines on myocardial revascularization. European Heart Journal 2010;31:2501–2555.
[4] Dunning J, Versteegh M, Fabbri A et al. Guideline on antiplatelet and anticoagulation management in cardiac surgery. European Journal of Cardio-thoracic Surgery 2008;34:73–92.
[5] Ferraris VA, Saha SP, Oestreich JHet al. 2012 Update to the Society of Thoracic Surgeons Guideline on use of antiplatelet drugs in patients having cardiac and noncardiac operations. Annals Thoracic Surgery 2012;94:1761–1781.
[6] Kulik A, May M, Voisine P et al. Aspirin plus clopidogrel versus aspirin alone after coronary artery bypass grafting. The Clopidogrel after Surgery for Coronary Artery Disease (CASCADE) trial. Circulation 2010;122:2680–2687.
[7] Vahanian A, Alfieri O, Andreotti F et al. Guidelines on the management of valvular heart disease (version 2012). European Heart Journal 2012;33:2451–2496.
[8] Keeling D, Baglin T, Tait C et al. Guidelines on oral anticoagulation with warfarin — Fourth edition. British Journal of Haematology 2011;154:311–324.
[9] Camm JA. Kirchhof P, Lip GYH et al. Guidelines for the management of atrial fibrillation. ESC Guidelines. European Heart Journal 2010;31:2369–2429.
[10] National Institute for Health and Care Excellence. Atrial fibrillation: the management of atrial fibrillation. London: NICE 2014.
[11] Rho RW. The management of atrial fibrillation after cardiac surgery. Heart 2009;95:422–429.
[12] Hogue CW, Murphy SF, Schechtman KB et al. Risk factors for early or delayed stroke after cardiac surgery. Circulation 1999;100:642–647.
[13] Stamou SC, Hill PC, Dangas G et al. Stroke after coronary artery bypass: incidence, predictors, and clinical outcome. Stroke Journal of the American Heart Association 2001;32:1508–1513.
[14] Diez C, Koch D, Kuss O et al. Risk factors for mediastinitis after cardiac surgery — a retrospective analysis of 1700 patients. Journal of Cardiothoracic Surgery 2007;2:23.
[15] Kulik A, Brookhart A, Levin R et al. Impact of statin use on outcomes after coronary artery bypass graft surgery. Circulation 2008;118:1758–1792.
[16] Bellomo R, Raman J & Ronco C. Intensive care unit management of the critically ill patient with fluid overload after open heart surgery. Cardiology 2001;96:169–176.
[17] National Institute for Health and Care Excellence. Prophylaxis against infective endocarditis: Antimicrobial prophylaxis against infective endocarditis in adults and children undergoing interventional procedures. London: NICE 2008.
[18] Habib G, Hoen B, Tornos Pet al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009). European Heart Journal 2009;30:2369–2413.
[19] Summary of Product Characteristics for Pradaxa 150mg hard capsules. Boehringer Ingelheim Limited. Accessed via www.medicines.org.uk. Last updated 10 July 2014 (accessed 30 August 2014).
[20] Summary of Product Characteristics for Eliquis 5mg film-coated tablets. Bristol-Myers Sqibb-Pifzer. Accessed via www.medicines.org.uk. Last updated 30 July 2014 (accessed 30 August 2014).
[21] Summary of Product Characteristics for Xarelto 20mg film-coated tablets. Bayer plc. Accessed via www.medicines.org.uk. Last updated 15 August 2014 (accessed 30 August 2014).



