
Oliver Dixon / Alamy
Summary
In this article you will learn:
The current rules about driving after taking medicines
How the new drug driving offence will affect patients
The common conditions that impair a patient’s fitness to drive
How to advise patients driving after surgery
There are an estimated 200 drug driving-related deaths in the UK each year[1]
. In an attempt to reduce these deaths, a new offence for driving under the influence of 16 specified controlled drugs is due to come into force in March 2015. The main targets of this new legislation are those whose driving is impaired following the recreational use of drugs that are taken illegally or abused[2]
.
Medicines and driving
Section 4 of the Road Traffic Act 1988 already makes it illegal to drive if your driving is impaired through the use of drugs, regardless of whether or not the drugs are being used legally. This means that if a patient’s driving is found to be impaired by medicines, even when taking them as prescribed by a healthcare professional or in accordance with the product information, he or she may still be prosecuted.
If convicted of drug driving, the possible penalties include a minimum of one year’s driving ban, a fine of up to £5,000 and a criminal record. The individual’s driving licence will show the conviction of drug driving for 11 years and there may be additional consequences, such as increased car insurance costs and difficulties travelling to countries such as the United States[3]
. This existing offence will remain in place alongside the new drug driving offence[4]
[5]
.
Patients should not drive if they feel drowsy or dizzy, are unable to concentrate or make decisions, or have vision problems. When a patient starts a medicine that could affect their driving ability, such as sedatives, pharmacists should advise them not to drive until they know how the medicine affects them[6]
.
An untreated medical condition may itself impair a patient’s ability to drive, and it is important to advise patients not to stop taking their medicines.
Drug driving
The new offence of ‘driving, attempting to drive, or being in charge of a vehicle with a specified controlled drug in the body in excess of specified levels’ is set to come into force on 2 March 2015. Roadside drug screening devices will use saliva to identify the prohibited drugs[4] (see Roadside drug testing). Those found guilty will face up to six months imprisonment and a fine of up to £5,000, as well as being disqualified from driving for at least 12 months.
The first group of controlled drugs are commonly abused drugs or their metabolites, for which low blood concentration limits have been set (see New drug driving limits). These are cannabis, methylenedioxymethamphetamine (MDMA; ecstasy), ketamine, methylamphetamine (crystal meth), cocaine, lysergic acid diethylamide (LSD) and diamorphine (heroin)[4]
. Amphetamine is expected to be included later in 2015, once a limit has been agreed[4]
.
The second group consists mainly of licensed medicines that have a significant liability to be abused. The specified limits have been set higher than those in the first group. These are clonazepam, diazepam, lorazepam, oxazepam, temazepam, flunitrazepam, methadone and morphine[4]
.
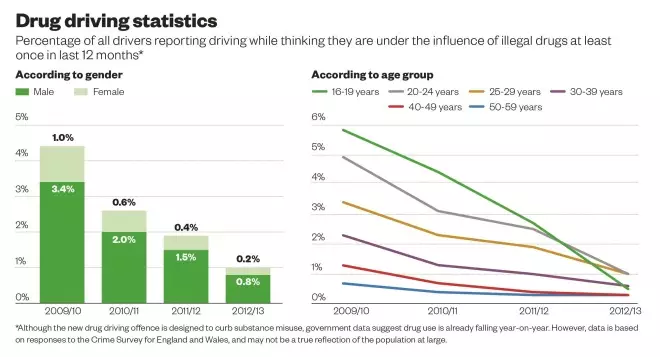
Source: National Crime Survey
New drug driving limits
- Benzoylecgonine (cocaine metabolite), 50 µg/L
- Cocaine, 10 µg/L
- Tetrahydrocannabinol (cannabis), 2 µg/L
- Lysergic acid diethylamide (LSD), 1 µg/L
- Methylamphetamine, 10 µg/L
- Methylenedioxymethamphetamine (MDMA; ecstasy), 10 µg/L
- 6-Monoacetylmorphine (diamorphine metabolite), 5 µg/L
- Clonazepam, 50 µg/L
- Diazepam, 550 µg/L
- Flunitrazepam, 300 µg/L
- Ketamine, 20 µg/L
- Lorazepam, 100 µg/L
- Methadone, 500 µg/L
- Morphine, 80 µg/L
- Oxazepam, 300 µg/L
- Temazepam, 1,000 µg/L
Source: Department for Transport
To protect patients who may test positive for certain specified drugs, the new offence has a statutory medical defence. This may be raised at any point, providing that the drug was:
- lawfully prescribed and supplied for medical or dental purposes; and
- taken in accordance with advice given by the prescriber or supplier, and in accordance with any accompanying written instructions (provided these are consistent with any advice given by the prescriber)[4]
.
Patient-specific advice provided by a healthcare professional may sometimes differ from the general information given in the patient information leaflet of a medicine. In these cases, the advice provided by the healthcare professional may be used as a basis for the patient’s statutory medical defence[4]
.
It is important to note that if the individual’s driving is impaired they can still be prosecuted under the existing offence of driving while impaired through drugs, for which there is no statutory medical defence.
Roadside drug testing

Source: 67photo / Alamy
Lateral flow drug detection devices, which require a saliva sample, will be used to test for drug driving
Police already have the power, introduced in the Railways and Transport Safety Act 2003, to conduct roadside drug tests. Currently, these impairment tests include asking the suspect to walk in a straight line or touch the tip of their nose. The police also assess whether the suspect has dilated pupils or slurred speech. Suspects are then taken to the police station for a blood test.
From March 2015, police will use lateral flow drug detection devices to test for the new offence, which require a saliva sample.
The test takes around 12 minutes in total and can test for up to eight substances. Suspects are asked to swab the test kit inside their cheeks for up to four minutes, before the sample is taken into the device and tested.
The test uses antibodies to detect the controlled substances in a similar way to a pregnancy test. The devices give only a positive or negative reading, and do not state the amount of drug detected. Current roadside testing equipment can detect as little as 10ng/L for some substances. If the test is positive, the suspect will be taken for a blood test.
The equipment used by police forces throughout the UK will vary depending on their individual budgets, priorities and equipment contracts.
Patient advice
The Medicines and Healthcare products Regulatory Agency (MHRA) requires all affected medicines to carry a warning that it may be an offence to drive after taking the medicine. A range of other medicines, including some OTC products, will also include the new warning. This includes codeine, fentanyl, tramadol and pethidine.
Although the new legislation is not due to come into force until next year, it is likely that medicines with the new information on their packaging and patient information leaflets will start to appear in pharmacies from September 2014[2]
.
Pharmacists should advise patients to keep some suitable evidence with them when driving to show that they are taking their medicine as prescribed (e.g. a repeat prescription slip, the patient information leaflet, or in accordance with the manufacturer’s instructions if purchased over the counter).
If a patient taking one of the specified controlled drugs starts any new medicine, pharmacists should consider whether the new medicine will cause an interaction that could affect the controlled drug’s blood levels. Patients should also be reminded that alcohol taken in combination with any of the specified controlled drugs, even in small amounts, can greatly increase the risk of accidents[4]
.
Medical conditions
The two drug driving offences are in addition to the existing rules on fitness to drive requirements for patients with various medical conditions.
People with a driving licence must already inform the Driving and Vehicle Licensing Agency (DVLA), or Driver and Vehicle Agency (DVA) in Northern Ireland, if they develop a condition or disability that may affect their ability to drive, or if they have a condition or disability that gets worse. If they fail to notify the DVLA or DVA, they may be fined up to £1,000 and could be prosecuted if they are involved in an accident[7]
. Notifiable medical conditions include: diabetes; epilepsy; neurological and mental health conditions; visual impairments; and alcohol and substance misuse[7]
.
The requirement to report a condition may depend on whether the person holds a group 1 licence (for a car or motorcycle), or a group 2 licence (for a bus, coach or lorry), as well as the condition itself and how it is managed.
Diabetes is a notifiable medical condition for those treated with insulin, unless: they are a group 1 licence holder only; their treatment is temporary for a condition such as gestational diabetes; and they are under medical supervision and have not been advised that they are at risk of hypoglycaemia[8]
.
Epilepsy is the most frequent cause of loss of consciousness while driving, and all drivers with epilepsy must notify the DVLA of their condition[8]
. The decision as to whether a patient with a history of seizures is allowed to drive depends on a number of factors, including the time since the last seizure, any patterns as to when seizures occur, and whether a seizure was provoked[9]
.
Stopping antiepileptic medicines may cause seizures to recur, and pharmacists should ask patients with epilepsy if they drive when there is a change to their medicines. Patients should be counselled on the risk of having a seizure, and warned that they could lose their driving licence and potentially cause a road traffic accident if they are driving at the time[9]
.
Alcohol misuse, if confirmed and persistent, will result in the DVLA or DVA revoking a patient’s group 1 licence, or refusing their application until a minimum of six months of controlled drinking or abstinence has been attained. A group 2 licence will be revoked or refused until control or abstinence has been attained for one year[10]
.
Substance misuse patients who are fully compliant with a consultant-supervised oral methadone or buprenorphine maintenance programme may obtain a group 1 licence, subject to “favourable assessment” and, usually, an annual medical review. A group 2 licence may be granted on a case-by-case basis once a three-year period of stability on a maintenance programme has been established, along with negative random urine tests and favourable assessments[11]
.
Patients recovering from surgery should be free from any distracting pain, and any sedative or other effects of medicines before driving. They should also be comfortable when sat in a driving position and able to control the car safely, including performing an emergency stop[12]
.
Update: Since this article was published, the regulations have been updated to also include amphetamine in the list of drugs with a set driving limit.
Further information
- Medicines and Healthcare products Regulatory Agency (MHRA) information for patients
- Department for Transport guidance for health professionals on drug driving
- Driver and Vehicle Licensing Agency (DVLA) guide for medical professionals on driving rules
- Royal College of Surgeons guidance on driving following common surgical procedures
- Royal Pharmaceutical Society members requiring further information on this topic can contact the RPS Support Team on 0333 733 2570 or email support@rpharms.com
About the author
Katie Perkins MPharm CertPharmPract MRPharmS is a professional support pharmacist with the Royal Pharmaceutical Society’s support team.
References
[1] Department for Transport. Regulations to specify the drugs and corresponding limits for the new offence of driving with a specified controlled drug in the body above the specified limit - A Consultation Document [Online].
[2] Medicines and Healthcare Products Regulatory Agency. Letter to all holders of Marketing Authorisations of medicines controlled by the Misuse of Drugs Act September 2013. New drug driving offence—Implications for medicines packaging [Online].
[3] GOV.UK. Drugs and driving: the law [Online]. [accessed on 5 September 2014].
[4] Department for Transport. Guidance for healthcare professionals on drug driving July 2014 [Online].
[5] Road Traffic Act 1988 Chapter 52 Part 1 Section 4 [Online].
[6] Medicines and Healthcare Products Regulatory Agency. Drug Safety Update July 2014. Drugs and driving: blood concentration limits to be set for certain controlled drugs in a new legal offence [Online].
[7] GOV.UK. Medical conditions, disabilities and driving [Online].
[8] Driver and Vehicle Licensing Agency. DVLA’s current medical guidelines for professionals—conditions D to F [Online].
[9] Driver and Vehicle Licensing Agency. Current medical guidelines: DVLA guidance for professionals—Neurological appendix [Online].
[10] Driver and Vehicle Licensing Agency. DVLA’s current medical guidelines for professionals—conditions A to C [Online].
[11] Driver and Vehicle Licensing Agency. DVLA’s current medical guidelines for professionals—conditions M to O [Online].
[12] The Royal College of Surgeons. Get Well Soon [Online].


