
Shutterstock
After reading this article, you should be able to:
- Describe the use of entrustable professional activities (EPAs) within a pharmacy context;
- Define a decreasing level of supervision in an EPA structure within a pharmacy context;
- Reflect on personal practices around supervising trainee pharmacists.
Introduction
In 2021, the General Pharmaceutical Council (GPhC) changed its standards for the education and training of pharmacists[1]. All pharmacists qualifying from 2026 will be qualified independent prescribers and will take on the associated additional roles and responsibilities. To facilitate this transition, the profession’s approach to education and training must also adapt and change.
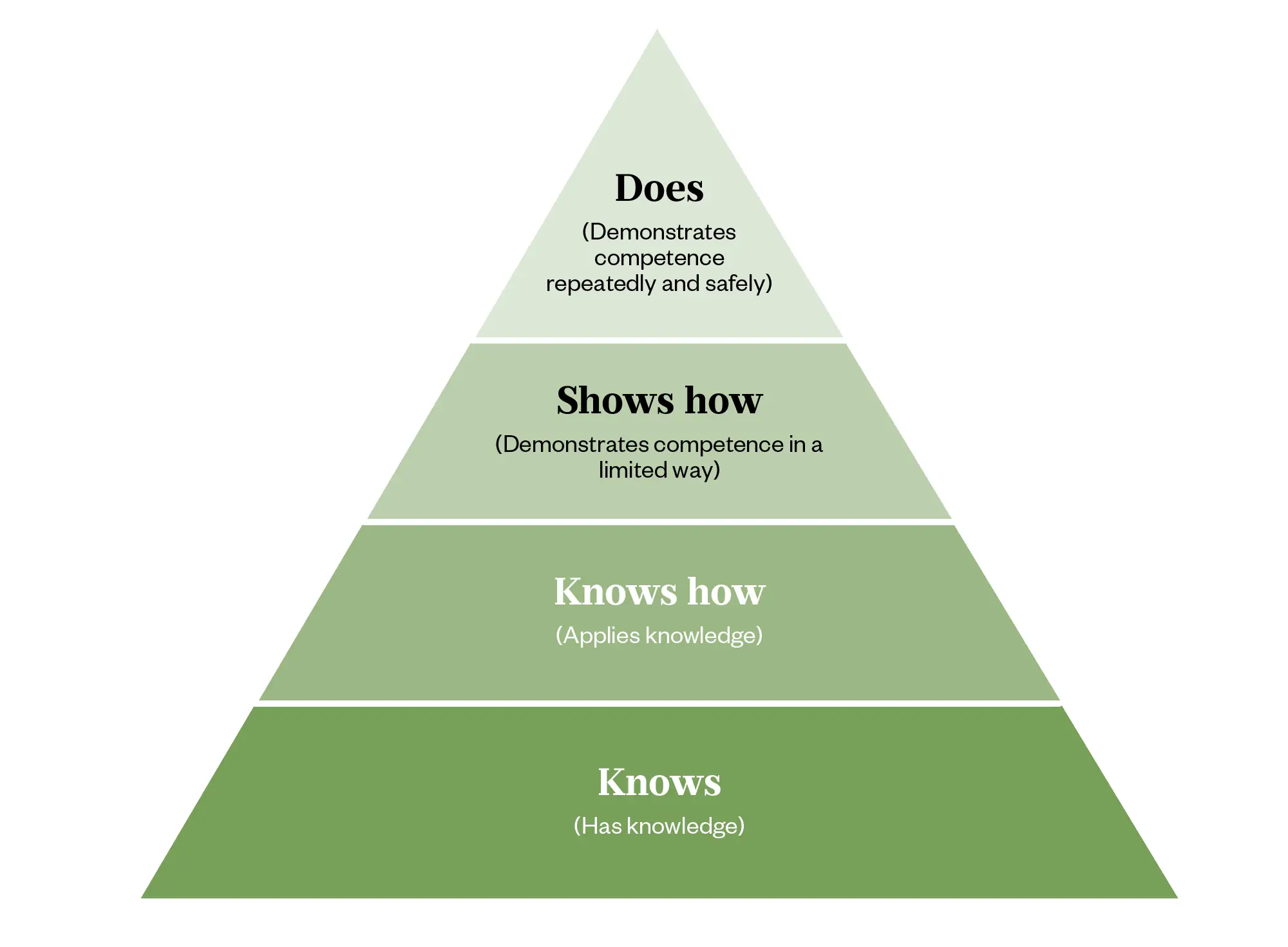
Education and training are provided by higher education institutions at an undergraduate level and foundation training providers at the foundation training level. The required changes are significant, not least because of pressures on placement provisions, clinical settings and increasing trainee numbers[2–4]. Many of the learning outcomes stipulated by the GPhC that underpin prescribing must be demonstrated at the ‘shows how’ or ‘does’ level of Miller’s triangle, to allow trainees to develop and evidence the necessary knowledge, skills and behaviours for safe and effective prescribing (see Figure 1)[1].
The Pharmaceutical Journal
The increased emphasis on prescribing and clinical experience means there is a greater need for meaningful placement experiences within all stages of training, where trainees can practise their skills and demonstrate their competence at the required level to be workforce ready (i.e. active participation rather than observation). The existing pharmacy workforce has a major role to play in facilitating this expansion of practice learning and it is important that pharmacy teams are suitably prepared and able to provide appropriate support and education to trainees. The concept of entrustable professional activities (EPAs) can provide a scaffold to the profession’s approach to work-based placements by offering a safe and evidence-based approach to facilitating trainee development of skills and knowledge for prescribing.
This article will explain the concept of EPAs, show the value they offer for training towards prescribing practice and how pharmacists can make use of EPAs when supporting trainees on placements.
Entrustable professional activities
EPAs are units of professional activity that can be fully entrusted to an individual trainee, once they have demonstrated the necessary skill to execute them unsupervised[5,6]. EPAs support active participation and trainee development as supervision generally decreases over time as trainees develop their skills and competence and become entrusted to work more independently[7,8]. One of the benefits of EPAs is that they provide a structured approach to entrustment that balances risk and patient safety with the need for trainees to access learning opportunities[9].
EPAs were originally developed within medicine and have an established evidence-base supporting their use[10]. More recently, EPAs have been adopted by a range of healthcare professions, including pharmacy[7]. The American Association of Colleges of Pharmacy published a national list of 15 EPAs for pharmacy graduates in 2017[10]. In 2023, NHS England and the Pharmacy Schools Council (PhSC) published a joint report on establishing national EPAs for use in the UK to meet GPhC standards[11].
The joint report suggests that the use of EPAs can be flexible and determined by the curricula of the higher education institution or provider, but acknowledged that not all EPAs will be suitable for a particular placement given they may not always be achievable in a given setting[12]. For example, if an EPA relates to the dispensing and supply of medicines, it will not be suitable for a trainee working in a setting where medicines are not dispensed[12]. Examples of EPAs within pharmacy are ‘advise a patient on an issue associated with the use of a medicine’ and ‘discuss with patient and/or carer ideas, concerns and expectations about the management of their condition’[12].
In the UK, EPAs have mainly been used in undergraduate education and training; however, EPAs have been used internationally in the equivalent of foundation training and/or graduate training[13]. The same EPAs can be used throughout different levels of training, but changing the level of entrustment and supervision to reflect the progression and more advanced level of practice of the trainee[8].
Approaches to supervision and entrustment decisions
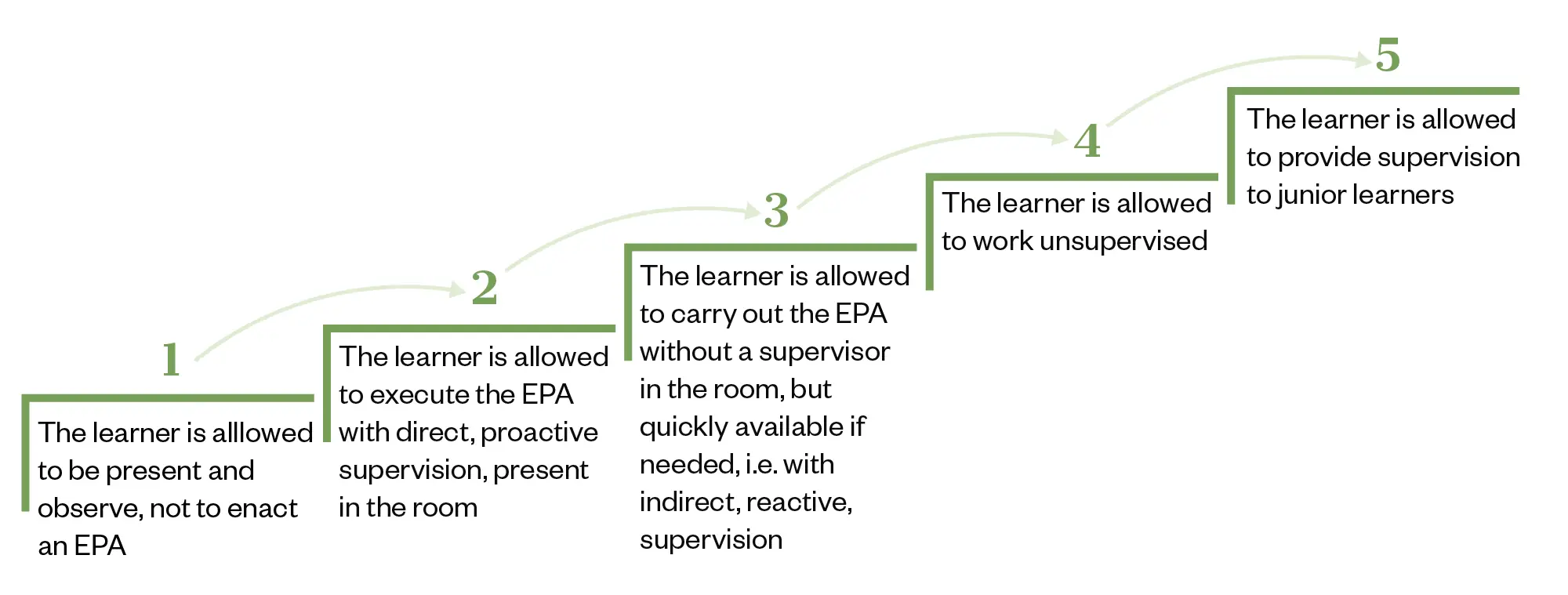
EPAs encourage the active participation of students and trainees in professional activities (with appropriate supervision determined by the level of entrustment)[8]. The level of entrustment is decided by a supervisor or collection of supervisors and reflects that a trainee has met specific, defined expectations for a given level of supervision (see Figure 2)[8,14]. Over time, a trainee will progress within an EPA and their level of required supervision will decrease (in other words, the level of entrustment will increase)[7,14].
The Pharmaceutical Journal
A trainee’s progression within an EPA is usually mirrored by[14]:
- Decreasing supervision with development of skills; and
- A transition from rigid adherence to the EPA procedures to a more intuitive mode of operation where the trainee is able to increasingly draw from their own clinical judgement.
Entrustment decisions should consider the ‘trustworthiness’ of the trainee in applying knowledge, skills and attitudes in performance of an EPA[14]. Trustworthy behaviours include truthfulness, conscientiousness and discernment (knowledge of one’s own limits and help-seeking behaviour)[14,15].
While working within an EPA, trainees may display different levels of behaviours, which can aid in entrustment decisions[16]:
- Behaviours requiring corrective response (e.g. is disrespectful in interactions with patients);
- Developing behaviours (e.g. communicates unidirectionally);
- Expected behaviours for an entrustable trainee (e.g. responds effectively to patient’s verbal and nonverbal cues and emotions).
Thinking in terms of behaviours and not necessarily competency can provide a useful scaffold when making entrustment decisions. When making entrustment decisions, practice supervisors might find it useful to ask themselves reflective questions, such as[14]:
- Will I let the trainee go in the room without me?
- How much will I let the trainee do versus observe?
- Because I wasn’t present to observe, how much do I need to double-check?
This can be done in such a way that patient safety is central and maintained, but balancing this with space for the trainee to develop.
The relationship between entrustable professional activities and competencies
It is important to understand that EPAs are not competencies[17]. As we have already established, an EPA is a unit of professional activity that a trainee can work within with a varying level of supervision. A competency, on the other hand, is the ability to do something successfully or efficiently. A trainee’s ability to perform an activity is the actual skill (demonstrating competence), and the EPA is simply the activity itself[17].
Assessment of students within entrustable professional activities for entrustment
Any given EPA may be made up of multiple competencies, skills or attitudes (see Table[16]) leading to the question of how they should be assessed[17]. One of the cornerstones of understanding and applying EPAs is that they are not intended as a form of assessment in and of themselves. Assessment should focus on the underlying attributes, competencies, skills and attitudes of trainees when working within an EPA[6,8].
Box 1: Entrustable professional activities at a pharmacy clinic
At Newcastle University, pharmacy students run a student-led clinic focused around cardiovascular screening[18]. The clinic uses several EPAs to structure student tasks, such as taking a blood pressure (BP) measurement. In this example, initial entrustment comes based on the previous academic year’s objective structured clinical examination, pre-placement simulation and in session supervision where it is likely trainees will start at supervision level two, possibly progressing to three through the year as skill develops (see Figure 1). The assessment is not necessarily focusing on the individual’s ability to take a blood pressure as the EPA, but of the developing and expected behaviours underpinning the EPA.
It is essential to assess trainees performing EPAs, not only for their development and progress but also to facilitate entrustment decisions and judging the required level of supervision. The generally adopted method for this is work-based assessment (WBA). Examples of WBAs include mini clinical evaluation exercises, direct observation of procedural skills and recording case-based discussions. NHS England already provides templates for the use of these across the profession[19].
Low levels of entrustment are to be expected initially and reflect the expectation that early learners need closer supervision[18]. With the EPA approach, a learner on day one of a placement may only be entrusted to be present and observe. With time, WBAs will accumulate providing evidence of the trainee’s competency of the attributes needed in the EPA which can then support entrustment decisions that reduce the level of supervision required. In this way, individual WBAs are not used as ‘sign off’ points or as a summative or progression decision, but rather as part of a whole portfolio of evidence that can be considered at regular touch points[5,20].
Entrustment decisions can also be ad hoc; for example, it can be quickly decided on the day that a trainee has demonstrated enough competency to complete an activity with less supervision[6,13]. Many designated practice supervisors will be doing this already within their clinical setting. When supervisors do this, the decision is often implicit (i.e., not clearly communicated as an entrustment decision)[6]. Ad hoc decisions allow the trainee slightly more entrustment to gather evidence (via WBAs) of working under less supervision, which then could be used to make a more formal entrustment decision (described in the literature as ‘structural decisions’), after which the trainee formally moves to the next level of supervision (Figure 2)[13]. Entrustment decisions can also go the other way, depending on the evidence and clinical context in which the trainee is working. That is, supervision can be reactively increased if the trainee demonstrates they are not yet ready for more independent practice[5].
At the end of a placement or rotation, summative entrustment decisions should be made by a trained group based on longitudinal performance assessments from multiple supervisors and documented day-to-day entrustment judgements by workplace supervisors[21]. Evidence of entrustment should capture that the trainee knows their limits (discernment), can be relied on to follow through (conscientiousness), and are forthcoming regarding their performance and development (truthfulness)[13,14,21].
Box 2: Assessment of trainees after EPAs
At the Newcastle University student-led clinic, all trainees complete a work-based portfolio as part of their study programme. Through this assessment (in addition to WBAs, which record their performance and the level of supervision they have required for various EPAs over an academic year), they record action plans and reflections. It is these entries that are assessed for the underlying skills and behaviours of EPAs and ‘trustworthy’ attributes described above. The overall portfolio contributes to future entrustment decisions in the next stage of study.
Summary
EPAs are a useful framework for considering the level of independence and supervision that a trainee can safely work within.
Ad hoc entrustment decisions are not dissimilar to the day-to-day decisions currently made by clinical supervisors; however, these can be coupled with structured entrustment decisions based on a portfolio of WBAs. The framework provided by EPAs can help trainee pharmacists to develop the skills, knowledge and attributes needed for prescribing and demonstrate progressive independent practice and decreased supervision requirements.
Adopting an EPA-based approach will represent a culture change for some practice learning providers. Traditional observational approaches to pharmacy supervision and entrustment may need to be unpicked and refocused. The aim of EPAs to allow trainees to work within environments more independently but within a carefully judged level of entrustment that encourages them to develop the attributes required for practice as prescribers while preserving patient safety.
- 1Standards for the education and training of pharmacist independent prescribers. General Pharmaceutical Council. 2021. https://www.pharmacyregulation.org/sites/default/files/document/standards_for_the_initial_education_and_training_of_pharmacists_january_2021_final_v1.4.pdf (accessed March 2024)
- 2Attenborough J, Abbott S, Brook J, et al. Everywhere and nowhere: Work-based learning in healthcare education. Nurse Education in Practice. 2019;36:132–8. https://doi.org/10.1016/j.nepr.2019.03.004
- 3Arja SB, Arja SB, M. Venkata R, et al. Integrated curriculum and the change process in undergraduate medical education. Medical Teacher. 2018;40:437–42. https://doi.org/10.1080/0142159x.2018.1441988
- 4Webb D, Cattell R, Fidler L. Open Letter to Pharmacy Professionals: NHS Long Term Workforce Plan. NHS England. 2023. https://www.rpharms.com/Portals/0/Documents/David%20Webb%20letter%20NHS%20LTWP%20300623.pdf?ver=_Ak0vLpYFgbgyF_lpyFh4A%3d%3d (accessed March 2024)
- 5Cate O ten. A primer on entrustable professional activities. Korean J Med Educ. 2018;30:1–10. https://doi.org/10.3946/kjme.2018.76
- 6ten Cate O. Entrustability of professional activities and competency-based training. Med Educ. 2005;39:1176–7. https://doi.org/10.1111/j.1365-2929.2005.02341.x
- 7Jarrett JB, Berenbrok LA, Goliak KL, et al. Entrustable Professional Activities as a Novel Framework for Pharmacy Education. American Journal of Pharmaceutical Education. 2018;82:6256. https://doi.org/10.5688/ajpe6256
- 8ten Cate O. Nuts and Bolts of Entrustable Professional Activities. Journal of Graduate Medical Education. 2013;5:157–8. https://doi.org/10.4300/jgme-d-12-00380.1
- 9El‐Haddad C, Damodaran A, McNeil HP, et al. The ABCs of entrustable professional activities: an overview of ‘entrustable professional activities’ in medical education. Internal Medicine Journal. 2016;46:1006–10. https://doi.org/10.1111/imj.12914
- 10Shorey S, Lau TC, Lau ST, et al. Entrustable professional activities in health care education: a scoping review. Medical Education. 2019;53:766–77. https://doi.org/10.1111/medu.13879
- 11Haines ST, Pittenger AL, Stolte SK, et al. Core Entrustable Professional Activities for New Pharmacy Graduates. American Journal of Pharmaceutical Education. 2017;81:S2. https://doi.org/10.5688/ajpe811s2
- 12NHS England & Pharmacy Schools Council proposed list of Entrustable Professional Activities. NHS England and Pharmacy Schools Council. https://www.hee.nhs.uk/sites/default/files/documents/List%20of%20EPAs%20Final.pdf (accessed March 2024)
- 13Eudaley ST, Brooks SP, Jones MJ, et al. Evaluation of student-perceived growth in entrustable professional activities after involvement in a transitions-of-care process within an adult medicine advanced pharmacy practice experience. Currents in Pharmacy Teaching and Learning. 2022;14:193–9. https://doi.org/10.1016/j.cptl.2021.11.032
- 14Obeso V, Brown D, Aiyer M. Core EPAs for Entering Residency Pilot Program. Association of American Medical Colleges. 2017. https://www.aamc.org/media/20196/download (accessed March 2024)
- 15Kennedy TJT, Regehr G, Baker GR, et al. Point-of-Care Assessment of Medical Trainee Competence for Independent Clinical Work. Academic Medicine. 2008;83:S89–92. https://doi.org/10.1097/acm.0b013e318183c8b7
- 16Barron B, Orlander P, Schwartz M. Core Entrustable Professional Activities for Entering Residency. Association of American Medical Colleges. 2017. https://www.aamc.org/media/20141/download (accessed March 2024)
- 17ten Cate O, Schumacher DJ. Entrustable professional activities versus competencies and skills: Exploring why different concepts are often conflated. Adv in Health Sci Educ. 2022;27:491–9. https://doi.org/10.1007/s10459-022-10098-7
- 18Nazar H, Rathbone AP, Richardson C, et al. Young@Heart clinic: a feasibility study of an undergraduate pharmacy student-led blood pressure and healthy lifestyle clinic. International Journal of Pharmacy Practice. 2021;29:277–84. https://doi.org/10.1093/ijpp/riab008
- 19E-portfolio and downloadable resources. NHS England. 2023. https://www.hee.nhs.uk/our-work/pharmacy/transforming-pharmacy-education-training/initial-education-training-pharmacists-reform-programme/foundation-trainee-pharmacist-1 (accessed April 2024)
- 20ten Cate O, Chen HC, Hoff RG, et al. Curriculum development for the workplace using Entrustable Professional Activities (EPAs): AMEE Guide No. 99. Medical Teacher. 2015;37:983–1002. https://doi.org/10.3109/0142159x.2015.1060308
- 21Brown DR, Warren JB, Hyderi A, et al. Finding a Path to Entrustment in Undergraduate Medical Education: A Progress Report From the AAMC Core Entrustable Professional Activities for Entering Residency Entrustment Concept Group. Academic Medicine. 2017;92:774–9. https://doi.org/10.1097/acm.0000000000001544


