Shutterstock.com
In short:
Healthcare-associated infections (HCAIs) can develop as a direct consequence of treatment or from a healthcare environment. They most often affect patients, but healthcare workers, family members and carers are also at an increased risk of acquiring an infection when caring for a patient. Infection control and prevention is an essential part of patient safety and public health and a recognised indicator of quality of care.
Healthcare workers should be up to date with routine immunisations, both for their own protection and for the protection of others, and follow recommended protocols in relation to protective equipment and hand hygiene (e.g. ‘five moments’), when delivering direct patient care.
There is no evidence to support the use of one particular hand-washing agent over another, even though their microbiologic efficacy varies. National and international guidelines recommend the use of alcohol-based hand rubs because of their ease of use and availability at point of care; however, they should only be used when hands are not visibly soiled or potentially contaminated with body fluids, or when caring for patients with vomiting or diarrhoeal illness. In these instances, and in cases of Clostridium difficile infection, soap and water should be used instead.
Healthcare-associated infections (HCAIs) can develop either as a direct consequence of treatment or from a healthcare environment. In addition to patients, healthcare workers, family members and carers are also at increased risk of acquiring an infection when caring for patients.
High standards of clinical care, infection prevention and control practices, including provision of a clean environment for patients, can minimise the risk of HCAIs. The National Institute for Health and Care Excellence (NICE) recommends that everyone involved in providing healthcare should understand the standard principles of infection control, and should be trained in hand decontamination, the use of personal protective equipment, and the safe use of sharp disposal and waste[1]
. Other important elements of preventing infections include ensuring staff are up to date with immunisations, using good infection control practices, and promoting good antimicrobial stewardship.
The ‘English National Point Prevalence Survey of Healthcare Associated Infections and Antimicrobial Use, 2011’, published by the Health Protection Agency, showed that the prevalence of HCAIs in England was 6.4% in 2011[2]
. The six most common types of HCAI, which accounted for more than 80% of all HCAIs, were respiratory tract infections, including pneum
onia and other respiratory infections (22.8%), urinary tract infections (17.2%), surgical site infections (15.7%), clinical sepsis (10.5%), gastrointestinal infections (8.8%) and bloodstream infections (7.3%) (see ‘An overview of healthcare-associated infection’). In children, the most common HCAIs were clinical sepsis (40.2%), respiratory tract infections (15.9%) and bloodstream infections (15.1%). Prevalence of HCAI was highest in patients in intensive care units (23.4%), followed by surgical wards (8.0%). Independent sector hospitals had a significantly low prevalence of HCAI of 2.2%, compared with NHS organisations at 6.5%
[2]
(see ‘An overview of healthcare-associated infection’).
The same survey demonstrated an 18-fold decline in methicillin-resistant Staphylococcus aureus (MRSA) infections (1.3% to 0.1%) and a five-fold decline in Clostridium difficile infection (2.0% to 0.4%) between 2006 and 2011 in hospitals in England[2]
.
Over the past decade, a number of legislative, regulatory and organisational initiatives have helped establish infection control as an essential part of patient safety and public health and as a recognised indicator of quality of care. The code of practice on the prevention and control of HCAI in the Health Act 2008, and the strict criteria for infection control provisions in the mandatory Care Quality Commission inspections of healthcare facilities, exerted legislative and regulatory pressure on to healthcare providers, which resulted in changes in organisational behaviour[3]
. The introduction of benchmarking and performance improvement targets for MRSA bacteraemia in 2004 and C. difficile in 2007 served as organisational drives in the reduction of infection rates[3]
,
[4]
.
Immunisation and occupational health
Healthcare workers should be appropriately immunised against infectious diseases, both for their own protection and the protection of others. The Department of Health recommends that healthcare staff involved in direct patient care should be up to date with their routine immunisations (e.g. tetanus, diphtheria, pertussis, polio and measles, mumps and rubella) as well as BCG [Bacillus Calmette–Guérin], hepatitis B, influenza and varicella vaccines[5]
. Healthcare workers who are working on specialist wards, such as infectious diseases units, may require additional vaccines (e.g. diphtheria booster given five years after original vaccination and subsequently at ten-yearly intervals)[5]
.
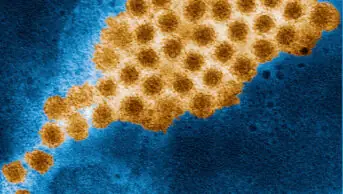
Infections such as meningococcal disease, pertussis, diphtheria and chickenpox can spread to non-immune or partially immune healthcare workers. Healthcare workers suffering from a known or suspected infectious disease should tell their occupational health department, who will advise on the management and exclusion from work, if required. Some hospital trusts may implement additional screening to control outbreaks or reduce risk of exposure to highly pathogenic organisms (e.g. MRSA, Panton-Valentine leukocidin-producing S. aureus).
Protective equipment
When delivering direct patient care, NICE recommends using disposable aprons if there is a risk that clothing may be exposed to blood, body fluid, secretions or excretions. It recommends the use of a long-sleeved fluid-repellent gown if there is a risk of extensive splashing of the body fluids on to skin or clothing. Disposable plastic gowns and gloves should be used once only and disposed of in medical waste bins for incineration. Face mask and eye protection must be worn when there is a risk of the body fluid splashing into the face or eyes[1]
.
Hand hygiene
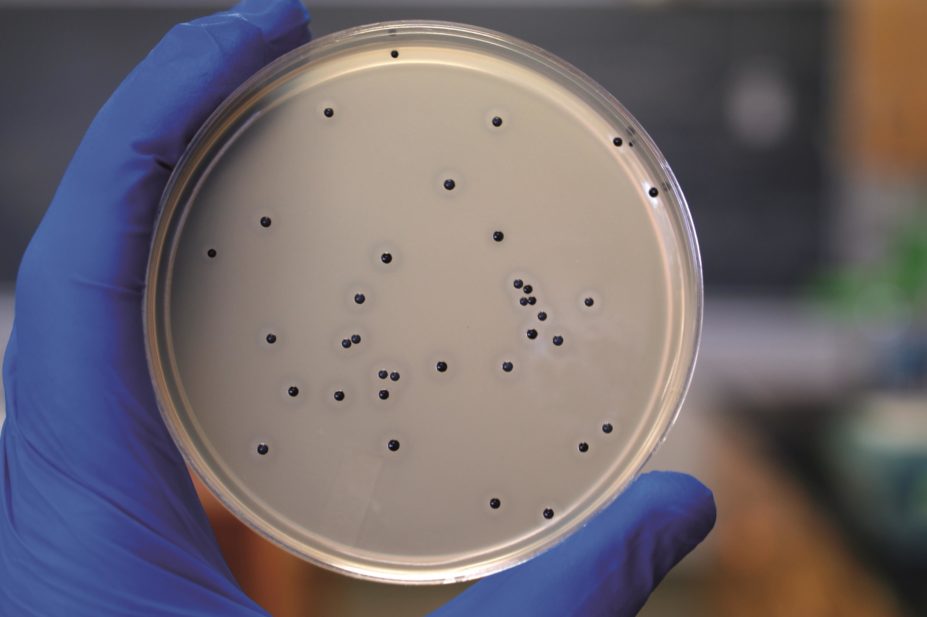
Transient flora are the most common cause of HCAIs, and are acquired and spread by direct contact with patients or environmental surfaces[6]
. These include organisms such as gram-negative bacilli, S. aureus, enterococci, C. difficile and respiratory syncytial virus[6]
. If transferred into susceptible sites, such as invasive devices (e.g. central venous and urinary catheter) or wounds, these organisms can cause life threatening infections.
In 2009, the World Health Organization produced guidelines on hand hygiene in healthcare, which outlines ‘five moments’ to perform hand hygiene[7]
:
- Before touching a patient;
- Before a clean or aseptic procedure;
- After body fluid exposure risk;
- After touching a patient;
- After touching a patient’s surroundings (e.g. changing bed linen).
Evidence is emerging that hand hygiene compliance after contact with patient surroundings is generally very poor in hospitals, and healthcare workers underestimate the role of environmental surfaces in transmission of HCAIs[8]
. Clinical notes, paper prescriptions and observation charts are part of the patient’s environment and any contact with these should be followed by appropriate hand hygiene.
There is no compelling evidence to favour a particular hand-washing agent (e.g. liquid soap, antiseptics) over others, even though their microbiological efficacy varies[6]
,
[9]
. Alcohol-based hand rubs are recommended by most national and international guidelines because of their ease of use and availability at the point of care[1],
[6],
[7],
[9]
. Alcohol hand rubs are suitable for use except when hands are visibly soiled or potentially contaminated with body fluids, or when caring for patients with vomiting or diarrhoeal illness. In these instances, soap and water should be used instead.
Soap and water is also recommended when washing hands following contact with a patient with C. difficile infection or their environment, as alcohol hand rubs and other disinfecting agents are not effective in reducing spore contamination[10]
.
To wash hands correctly, both the hands and wrists need to be fully exposed to the product, and therefore should be free from jewellery and long-sleeved clothing (bare below elbow). Non-analytical studies and case reports have demonstrated that ties, rings and false nails worn by healthcare workers can be colonised with potentially harmful microorganisms, and can impede performing effective hand hygiene[9]
.
When using alcohol gel, hands should be free of dirt and organic material and the gel solution must come into contact with all surfaces of the hand; the hand should be rubbed vigorously until the solution has evaporated.
When washing hands with a liquid soap, the solution should come into contact with all surfaces of the hand and the hands should be rubbed together for a minimum of 10–15 seconds. Particular attention should be paid to the tips of the fingers, the thumbs and the areas between the fingers. Hands should be thoroughly rinsed and then dried with a good-quality paper towel.
Mitul Patel is a consultant microbiologist at Birmingham Children’s Hospital NHS Foundation Trust.
References
[1] National Clinical Guideline Centre. Infection: prevention and control of healthcare-associated infections in primary and community care: partial update of NICE Clinical Guideline 2. NICE Clinical Guidelines, No. 139. London: Royal College of Physicians, 2012.
[2] Public Health England. The English national point prevalence survey on healthcare-associated infections and antimicrobial use, 2011.
[3] Department of Health. Health and Social Care Act 2008. Code of practice on the prevention and control of infections and related guidance. London: Department of Health 2008.
[4] Murray E & Holmes A. Addressing healthcare-associated infection and antimicrobial resistance from an organizational perspective: progress and challenges. Journal of Antimicrobial Chemotherapy 2012;67(1):i29–i36.
[5] Department of Health. Immunization of healthcare and laboratory staff: The Green Book: Chapter 12.
[6] Centre for Disease Control and Prevention. Guideline for hand hygiene in health-care settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA hand hygiene task force. Morbidity and Mortality Weekly Report. 2002;51:2–6.
[7] World Health Organization. Guidelines on hand hygiene in healthcare. 2009.
[8] FitzGerald G, Moore G & Wilson APR. Hand hygiene after touching a patient’s surrounding: the opportunities most commonly missed. Journal of Hospital Infection 2013;84(1):27–31.
[9] Loveday HP, Wilson JA, Pratt RJ et al. EPIC3: National evidence-based guidelines for prevention healthcare-associated infections in NHS hospitals in England. Journal of Hospital Infection 2014;86(S1):S1–S70.
[10] Public Health England and Department of Health. Clostridium difficile infection: How to deal with the problem. 2008.
You might also be interested in…

Everything you need to know about mpox
Norovirus and strategies for infection control
