Shutterstock.com
After reading this article, you should be able to:
- Describe the physiological effects of heat;
- Identify patients at risk of heat-related illnesses;
- Define the different types of heat-related illnesses and their management.
Introduction
Climate change and rising global temperatures pose an increasing threat to human health[1–3]. Hot days are expected to continue to increase in frequency and severity across the globe, and heatwaves and extended periods of hot weather are considered a natural hazard[1,3].
A heatwave is classified as a prolonged period of hot weather during which the daily maximum temperature reaches or exceeds a temperature threshold. As local climates differ both within the UK and globally, the definition of a heatwave and the heatwave temperature threshold can vary[2]. In the UK, there are heatwave day and night temperature thresholds for each county and a heatwave is confirmed by the Met Office when a temperature threshold is reached for at least three consecutive days[2,3].
Heatwaves are associated with excess morbidity and mortality[1,3]. Excess mortality during heat periods is evaluated by the Office for National Statistics and the UK Health Security Agency. A heat period is a day or days during which a level 3 heat-health alert is issued in England and/or when the mean temperature of central England is above 20°C.
During the 2022 UK heat periods, there were an estimated 3,271 excess deaths (compared with the five-year average), with 2,803 of these occurring in those aged over 65 years[4]. Heat vulnerability is also increasing with an ageing population and the related increasing incidence of health conditions that can be amplified by excessive heat, such as cardiovascular disease[1,3,5].
Exposure to heat drives the body to thermoregulate to prevent body heat gain, and these adaptive processes can cause physiological stress[1,5]. But heat also has other broader, indirect negative effects on health through changes in human behaviour, disease transmission, environmental pollution, wildfires, transport infrastructure, water shortages, crop failure and pressures on health and fire services[1,5,6]. Figure 1 shows the direct and indirect health impacts of exposure to extreme heat[1].
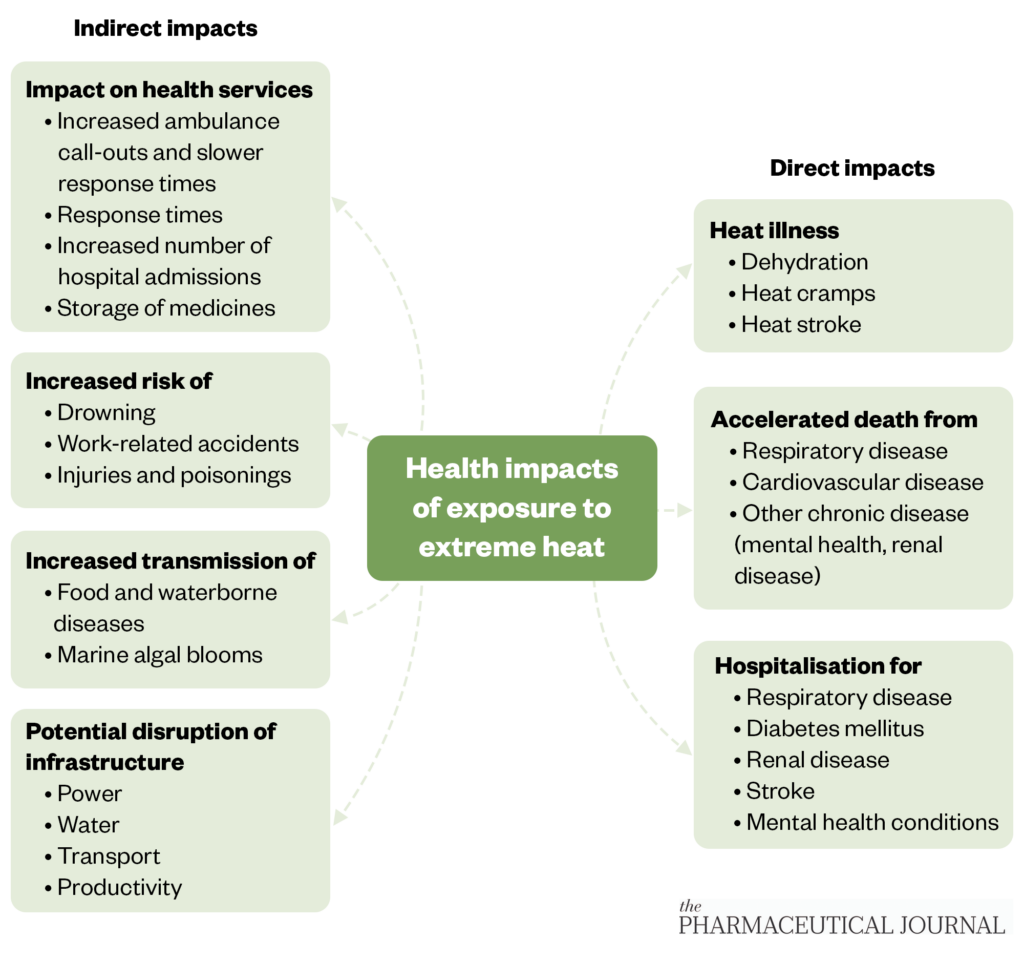
The Pharmaceutical Journal
Physiological effects of heat and impact on fluid balance
A consistent core body temperature of 37°C is needed for optimal cellular function and, ultimately, survival[1,5,6]. Multiple effector mechanisms are involved in this temperature regulation. Heat stress triggers the body’s main heat-loss responses of vasodilation and sweat secretion; however, prolonged or extreme exposure to heat, however, can impair thermoregulation, causing an inability to control body temperature and cumulative physiological stress[5,6]. This stress largely results from vasodilation-related blood redistribution, and fluid and electrolyte imbalance secondary to sweat loss. As seen in Figure 2[5], these thermoregulatory mechanisms can strain multiple organ systems[5]. Significantly, increased cardiovascular workload increases the risk of cardiovascular mortality, and hypovolaemia and renal hypoperfusion increase the risk of acute kidney injury.
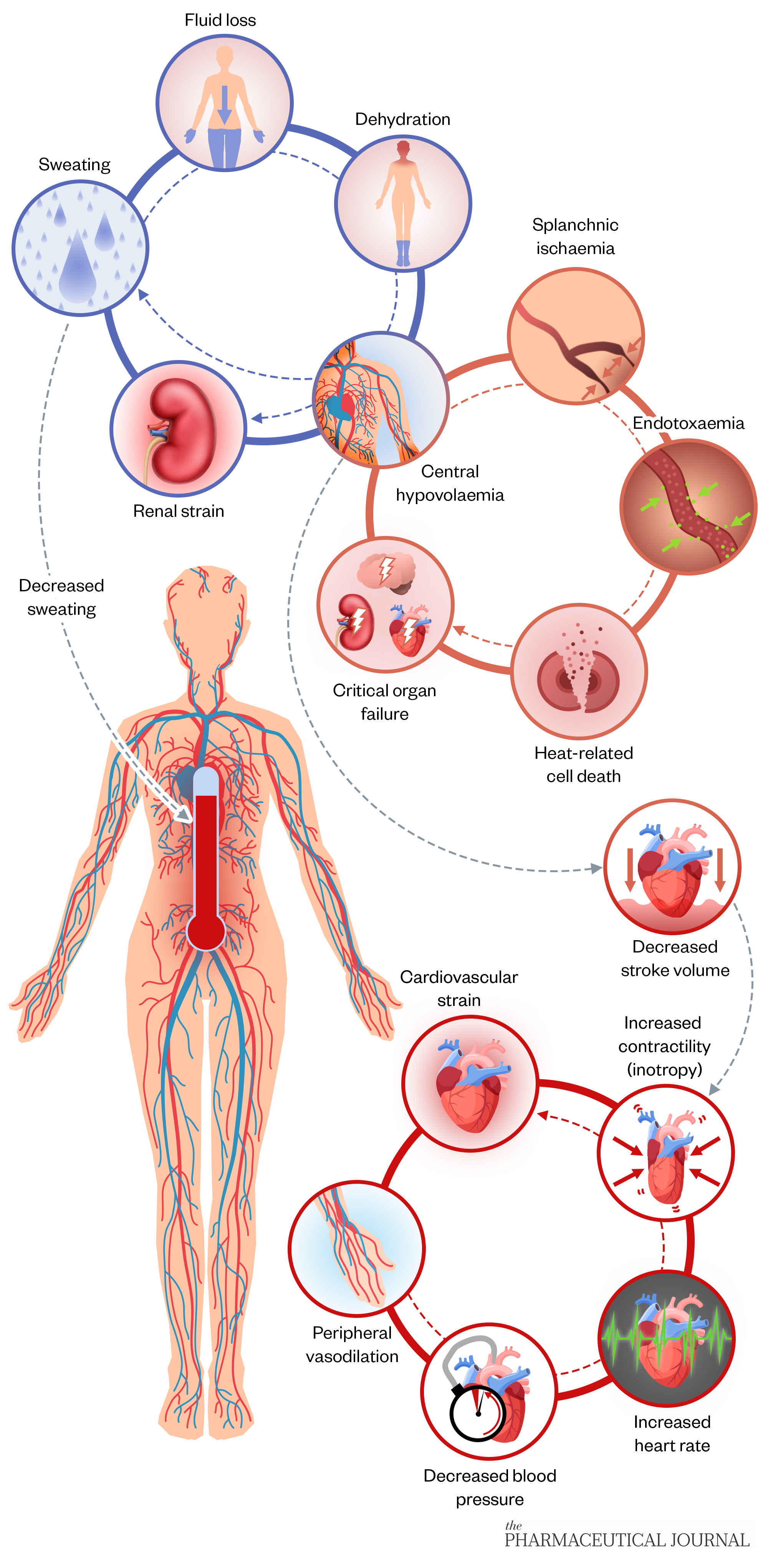
Shutterstock.com/The Pharmaceutical Journal
Risk factors for heat-related illnesses
Certain individuals are more vulnerable in extreme heat conditions and may require additional care during a heat wave, including:
- People with poor cognition owing to mental illness or disability, because they may not be able to sense or respond to dramatic changes in temperature. They may also not have capacity to take in information or advice about self-care in hot weather;
- Children and older people, who can have more difficulty regulating their body temperature. Care home residents are particularly at risk if the temperature within living quarters is not appropriately controlled or access to oral fluids is not accounted for. In addition, sweat mechanisms change with age, which decreases sweat rate, lowering evaporative capacity;
- People with pre-existing medical conditions (e.g. diabetes, renal disease and heart failure), who often take several drugs. The effects of certain drugs, such as renin–angiotensin–aldosterone system inhibitors and diuretics, can worsen heat-related illnesses (see Table 1);
- People who are overweight or obese, as they tend to retain more body heat and are therefore at greater risk of heat exhaustion or heat stroke;
- People with unconventional lifestyles, such as those who are homeless, abuse alcohol or use illicit drugs, as they may have no fixed abode and are therefore at risk of extensive heat exposure. A lack of access to oral fluids, coupled with prolonged heat exposure, can also precipitate dehydration and heat-related illness;
- Patients who work outdoors, such as gardeners and farmers, as they usually work in direct sunlight with limited access to shade or shelter. The physical work, combined with high humidity, no oral fluid access and no breaks when working, can make them more susceptible to heat-related illness[7].
Specific drugs (see Table 1) can precipitate or worsen heat-related illnesses, including:
- Drugs that affect cognition or cause sedation. Drowsiness or affected mental state may mean the patient is not aware of high temperature and the requirement to consume oral fluids. They may also not have the awareness to access cooler areas to minimise heat exposure, which can put them at risk of dehydration;
- Drugs that affect thermoregulation. Medicines that inhibit parasympathetic pathways can reduce sweating and prevent elimination of heat from the body;
- Drugs that affect the sweat response; namely, those causing hypohidrosis, which prevents the body from cooling itself and causes the physiological responses seen in heat exhaustion or heat stroke;
- Drugs that can accentuate dehydration. These may affect thirst response or trigger fluid and electrolyte loss[7,8].
Care must also be taken with certain transdermal and topical medicines during hot weather, as a medicine’s delivery rate can be increased by heat, resulting in toxicity. It is advised that people wearing transdermal patches avoid sunbathing, keep as cool as possible and be vigilant for potential symptoms of toxicity during hot weather. This is of particular importance with opioids, as heat-related, unintentional overdoses from opioid transdermal patches have been reported[9].
Common heat-related illnesses and how to tell them apart
Heat-related illnesses range from mild (heat cramps) to severe (heat stroke). They are grouped together as hyperthermia, which is when the body is unable to maintain its temperature in hot conditions without relief or adequate fluid intake[9,10]. It is essential to identify and manage the early stage of heat illness to prevent progression to heat stroke. See Table 2 for different heat-related illnesses and their treatment.
Heat cramps
Heat cramps, the mildest form of heat illness, are characterised by muscle cramps or spasms that occur in the lower limbs during intense exercise in high heat[11]. Muscular overuse and neuromuscular activity causes fluid and electrolyte depletion, and vasodilation caused by hot conditions exacerbates vascular leak, leading to increased interstitial fluid and concurrent oedema[12].
Affected individuals should cease physical activity and reduce overall body temperature; for example, by moving to a cooler environment and removing excess clothing[11,12]. Applying cool cloths can help to quickly cool the body, and slow stretches of cramped muscles will ease any pain in the limbs[11]. Affected individuals often sweat profusely in response to the high heat, so they must replenish lost fluid and electrolytes with oral fluids, such as water and sports drinks[11].
For people who work outdoors, reassure them that heat cramps are self-limiting and can be managed through adequate fluid replacement and regular access to sheltered areas[13].
Heat exhaustion
When measures to cool down the body are ineffective, heat exhaustion is the result, typified by excessive sweating and rapid fluid and electrolyte loss. Thermoregulatory dysfunction, hypovolaemia and hypotension increase the risk of dehydration, particularly in individuals with comorbidities or pre-existing risk factors[12].
Heat exhaustion is characterised by pale, moist skin and a fever (body temperature of more than 38oC). Gastrointestinal upset can also occur, which, coupled with fluid loss through sweat, increases the risk of dehydration. Headache and generalised fatigue are classic symptoms of heat exhaustion, as well as being early signs of dehydration.
Management of heat exhaustion is the same as for heat cramps. Care should be taken with children and older people, who are particularly at risk of heat exhaustion, and people who are unable to swallow should be referred to the emergency department. If appropriately managed, symptoms of mild heat exhaustion should generally resolve within two to three hours[14].
Heat stroke
When the body’s heat-regulating system is overwhelmed by excessive heat and is unable to cool itself, heat stroke occurs[10]. Heat stroke is a severe, untreated form of heat exhaustion that can last up to eight hours and, in extreme cases, can lead to cell death, organ failure and brain damage[12]. If heat stroke is suspected, the individual must be referred to the emergency department.
Unlike with heat exhaustion, people experiencing heat stroke have warm, dry skin and a high fever of more than 40oC. Tachycardia also presents, as well as gastrointestinal upset, such as nausea and vomiting. Heat stroke can also cause confusion and agitation, particularly in people at risk of dehydration[10]. Mortality can reach up to 80% in individuals experiencing heat stroke, particularly if body temperature exceeds 40oC, with or without prolonged hyperthermia; therefore, it is essential measures are taken to reduce body temperature quickly[12].
If heat stroke is suspected, follow the same cooling measures already described and apply ice bags in the armpit and groin areas[10]. If the individual can swallow, provide cool oral fluids to rehydrate and bring down body temperature. If in doubt, always refer the person to the emergency department — physical dehydration can quickly lead to acute kidney injury and cause seizures, coma and, in extreme cases, death[11,12].
A hospital patient with heat stroke is managed with IV isotonic fluids, such as normal saline or hypertonic fluids (5% dextrose in 0.9% sodium chloride). Use hypertonic fluids with caution in patients with renal or heart failure, as this may precipitate fluid overload[14]. More aggressive cooling measures, such as whole-body cold-water immersion, may be used in patients with exertional heat stroke[10,15]. Once the body temperature falls below 39oC, cooling measures must be stopped to avoid hypothermia[15]. Antipyretics should not be given in these patients; these only work when body temperature has increased owing to pyrogens and may exacerbate hepatic injury or disseminated intravascular coagulation[16]. If seizures present, anti-epileptics can be initiated as per hospital policy[10].
Sunburn
The first sign of many heat-related illnesses is changes in the skin. Though not usually fatal, it can cause discomfort and may lead to longer-term suffering in those with pre-existing dermatological conditions, such as drug-induced photosensitivity (see Table 1 for examples)[17].
Sunburn, or solar erythema, often presents as warm, red skin from excessive sun exposure[18]. If severe and left untreated, it can lead to painful blisters.
Treatment of sunburn:
- Avoid sun exposure until the skin completely heals;
- Apply cool cloths to the affected areas, or take a cool shower/bath;
- Drink plenty of water to cool down and prevent dehydration;
- Simple over-the-counter analgesia, such as paracetamol or ibuprofen[18].
Patients should not burst blisters as this can delay the healing process, as well as cause further pain. Petroleum jelly should never be applied directly to the skin, as it blocks pores, leading to retention of heat and sweat and increasing the risk of infection[19].
Prevention is often easier than treatment for sunburn. Preventative measures include:
- Using a broad-spectrum sunscreen containing UVA and UVB protection (SPF 30 or higher), reapplying every few hours or as often as the label indicates;
- Wearing protective clothing, including sunglasses with UV protection, light-coloured clothing and hats with wide brims;
- Avoiding the sun during the brightest, hottest times (usually between 11:00 and 15:00)[19].
Heat rash
Heat rash takes the form of small, red blisters that may resemble pimples[20]. These typically present on the neck, chest, groin or in elbow creases following sun exposure. Though uncomfortable, it usually self-resolves within a few days. Treatment of heat rash includes staying in cool, shaded areas and keeping the rash dry, if possible. Baby powder can help to sooth the rash as well as absorbing excess moisture on the skin. Alternative treatment options include calamine lotion, oral antihistamines, such as cetirizine, and topical hydrocortisone cream (note, this is unsuitable in pregnant women and children aged under 10 years)[20].

ISM / SCIENCE PHOTO LIBRARY
Summary
Further increases in hot days and heatwaves are expected as a result of global warming and climate change. Heatwaves are associated with excessive morbidity and mortality. Early identification and management of heat-related conditions (see Table 2) is essential, in particular with heat exhaustion to prevent progression to heat stroke.
- 1Heat and health. World Health Organization. 2018.https://www.who.int/news-room/fact-sheets/detail/climate-change-heat-and-health (accessed May 2023).
- 2Hot weather and its impacts. Met Office. 2023.https://www.metoffice.gov.uk/weather/warnings-and-advice/seasonal-advice/health-wellbeing/hot-weather-and-its-impacts (accessed May 2023).
- 3Hot weather and health: guidance and advice. UK Health Security Agency. 2023.https://www.gov.uk/government/collections/hot-weather-and-health-guidance-and-advice (accessed May 2023).
- 4Excess mortality during heat-periods: 1 June to 31 August 2022. Office for National Statistics. 2022.www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/excessmortalityduringheatperiods/englandandwales1juneto31august2022 (accessed May 2023).
- 5Ebi KL, Capon A, Berry P, et al. Hot weather and heat extremes: health risks. The Lancet. 2021;398:698–708. doi:10.1016/s0140-6736(21)01208-3
- 6Braian M B, Camila C, Antonella De V, et al. Human Physiology in Extreme Heat and Cold. Int Arch Clin Physiol. 2018;1. doi:10.23937/iacph-2017/1710001
- 7Anderson RK, Kenney WL. Effect of age on heat-activated sweat gland density and flow during exercise in dry heat. Journal of Applied Physiology. 1987;63:1089–94. doi:10.1152/jappl.1987.63.3.1089
- 8Charder N, Knoll J. Heatstroke and psychiatric Patients. Psychiatric Times. 2014.https://www.psychiatrictimes.com/view/heatstroke-and-psychiatric-patients (accessed May 2023).
- 9Using transdermal patches safely in healthcare settings. Specialist Pharmacy Service. 2022.https://www.sps.nhs.uk/articles/using-transdermal-patches-safely-in-healthcare-settings/ (accessed May 2023).
- 10Starkman E. What is heat-related illness? WebMD. 2021.https://www.webmd.com/first-aid/understanding-heat-related-illness-basics (accessed May 2023).
- 11Heat-related illnesses (heat cramps, heat exhaustion, heat stroke). Johns Hopkins Medicine. 2020.www.hopkinsmedicine.org/health/conditions-and-diseases/heatrelated-illnesses-heat-cramps-heat-exhaustion-heat-stroke (accessed May 2023).
- 12Gauer R, Meyers B. Heat-related illnesses. American Family Physician. 2019.https://www.aafp.org/pubs/afp/issues/2019/0415/p482.html (accessed May 2023).
- 13Calvello EJ, Hu K, Khoujah D. Management of the hyperthermic patient. Br J Hosp Med. 2011;72:571–5. doi:10.12968/hmed.2011.72.10.571
- 14Glazer J, Small H. Heat stroke in adults. BMJ Best Practice. 2022.https://bestpractice.bmj.com/topics/en-gb/3000174/treatment-algorithm (accessed May 2023).
- 15Lipman GS, Gaudio FG, Eifling KP, et al. Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Heat Illness: 2019 Update. Wilderness & Environmental Medicine. 2019;30:S33–46. doi:10.1016/j.wem.2018.10.004
- 16Tek D, Olshaker J. Heat illness. Emerg Med Clin North Am 1992;10:299–310.https://www.ncbi.nlm.nih.gov/pubmed/1559470
- 17Lau L, Vu M, Scardamaglia L, et al. Drug-induced photosensitivity. DermNet. 2023.https://dermnetnz.org/topics/drug-induced-photosensitivity (accessed May 2023).
- 18Sunburn. NHS. 2022.www.nhs.uk/conditions/sunburn (accessed May 2023).
- 19Heat rash (prickly heat). NHS. 2021.www.nhs.uk/conditions/heat-rash-prickly-heat (accessed May 2023).
- 20Sunburn. Medline Plus. 2021.medlineplus.gov/ency/article/003227.htm (accessed May 2023).