This content was published in 2009. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
In short
Patients with impaired renal function pose many pharmaceutical challenges for clinicians and usually require specialist care for their medicines to be optimised.
However, even pharmacists without specialist knowledge of renal medicine can offer important clinical input if they follow the basic steps outlined in this article.
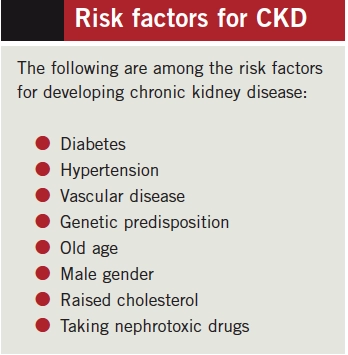
Renal failure, both acute and chronic, is caused by loss of function of nephrons. In chronic kidney disease (CKD) this process is usually gradual with permanent loss of kidney function over time. Although renal medicine is a speciality in its own right, most clinical pharmacists will regularly encounter patients with compromised renal function. It is therefore essential to have a basic understanding of CKD and its impact on patients’ ability to tolerate, and clear, medicines. This article offers some simple suggestions on how to approach the clinical assessment of prescriptions for such patients.
Monitoring renal function
Creatinine is almost exclusively eliminated by the kidneys and has proved to be a useful surrogate for estimating renal function. However, serum creatinine concentrations can be influenced by factors such as age, gender, race, weight and even diet. The “Cockcroft and Gault” and “Modification of diet in renal disease” (MDRD) equations are used to determine glomerular filtration rate (GFR) — see Box 1. Because they use different parameters they can produce different results. It is therefore essential to understand when to use each equation.
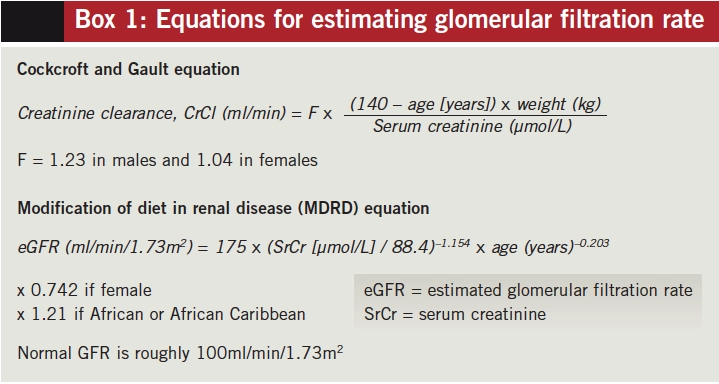
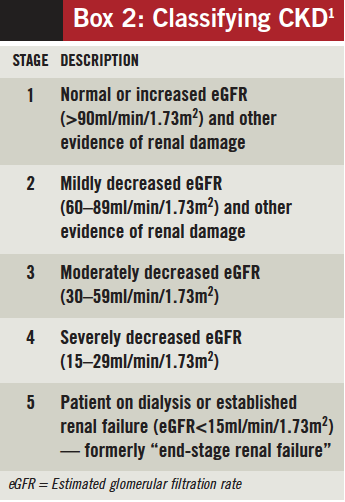
CKD classification (Box 2) is now based on an estimated GFR (eGFR) using the MDRD formula. This result is commonly reported alongside serum creatinine concentrations. Most standard references still use Cockcroft and Gault when offering advice on drug dosing. Use of the MDRD equation in this case can lead to potentially dangerous dosing errors.
Impact of CKD on medication
As renal function declines, medicines eliminated by the kidneys show reduced clearance and a prolonged plasma half-life.
Medicines metabolised to inactive compounds or excreted by non-renal routes are not affected; thus normal doses can be used.
It is also necessary to consider the therapeutic index of medicines used for renally impaired patients. Medicines that are renally excreted but have a wide therapeutic index are unlikely to be problematic in clinical practice. Medicines that are cleared renally and have a narrow therapeutic index (eg, aminoglycosides and vancomycin) have little safety margin and require careful dose adjustment.
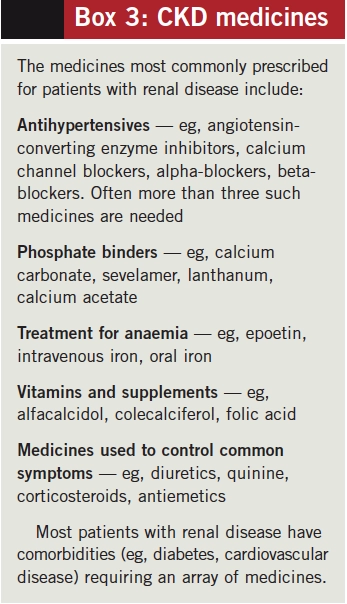
Medicines for CKD
When reviewing a prescription, the medicines prescribed can sometimes offer clues to the patient’s renal status. Commonly prescribed medicines for patients with CKD are listed in Box 3.
Renal replacement therapy
Ultimately, when the kidneys fail it is necessary to replace their critical functions with artificial methods. Types of renal replacement therapy (RRT) include haemodialysis, peritoneal dialysis, continuous renal replacement and haemodiafiltration.
Depending on their properties, medicines may be removed from the bloodstream by RRT. Drug molecules that are not bound to plasma proteins, or that have a low molecular weight, high water solubility or low volume of distribution, tend to be cleared more rapidly by RRT. Depending on how well a medicine is dialysed and the type of RRT, additional doses or even administration post-RRT can be required to avoid subtherapeutic levels. Specialist reference texts should be consulted when offering dosing advice for patients receiving RRT.
Some patients with established renal failure (CKD stage 4–5) have sufficient residual renal function to support life. They can therefore survive with little external renal support. However, it is extremely important to avoid nephrotoxic medicines for such patients.
Transplantation challenges
Transplant recipients pose different challenges for the clinical pharmacist. They can have nearly normal renal function, although this can vary significantly within and between such patients. It is therefore advisable to establish their current renal function. Furthermore, nephrotoxic drugs should be avoided or used only under specialist care.
Immunosuppressants prescribed to prevent rejection have narrow therapeutic windows and numerous drug interactions. This must be borne in mind when clinically checking prescriptions for renal transplant patients.
Information sources
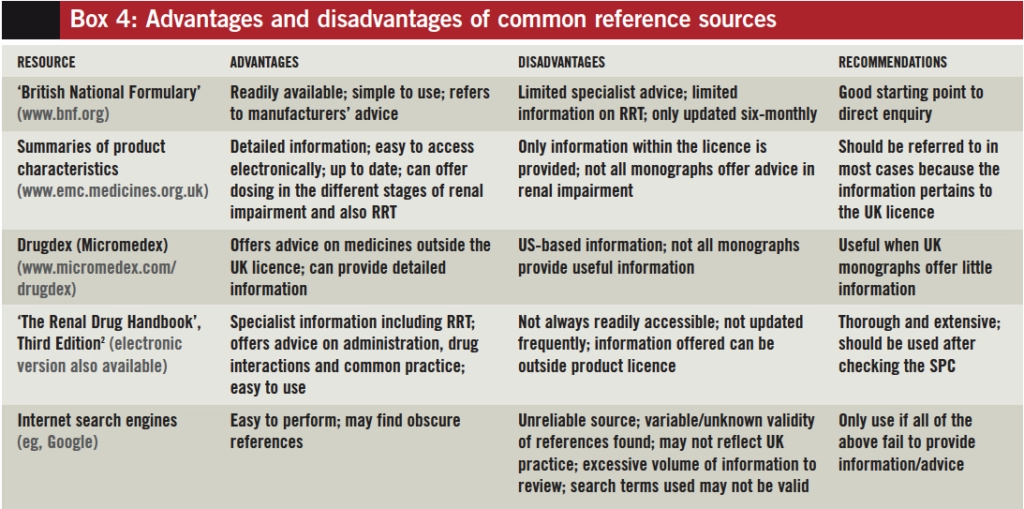
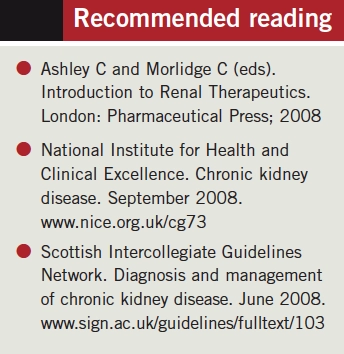
Although most clinical pharmacists head straight for ‘The Renal Drug Handbook’,2 it is wise to start by checking the most readily available resources. A 2005 review of four common reference sources highlighted a variation in definition of CKD as well as the advice offered.3 Box 4 illustrates advantages and disadvantages of common reference sources.
Clinically checking prescriptions
A prescription for a patient with CKD might seem daunting at first glance; however, the eight steps listed in the Box below can be useful when clinically checking the prescription.
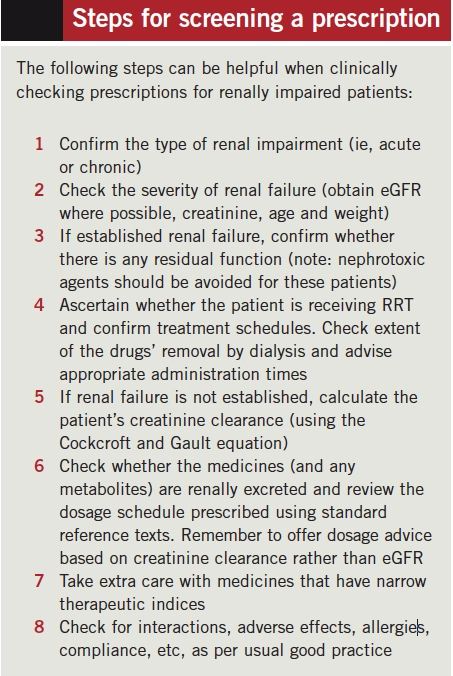
We appreciate it is not always possible to undertake a complete and thorough clinical evaluation of all the medicines taken by a patient with renal dysfunction. However, by using a structured approach pharmacists can ensure the safety of a prescription and prevent major errors in prescribing. With experience pharmacists can learn where to focus their attention.
References
- National Institute for Health and Clinical Excellence. Chronic kidney disease. September 2008. www.nice.org.uk/cg73 (accessed 18 March 2009).
- C Ashley, A Currie (eds). The Renal Drug Handbook. Third Edition. Oxford: Radcliffe Publishing; 2009.
- Vidal L, Shavit M, Fraser A, et al. Systematic comparison of four sources of drug information regarding adjustment of dose for renal function. BMJ 2005;331:263.
You might also be interested in…
How to support patients taking new oral anticoagulant medicines