
BSIP SA / Alamy Stock Photo
Clinical teachers are integral to the education of health professionals. They are usually individuals who have several years of practical experience in patient-facing settings, an interest in teaching and mentoring, and a practice site that is conducive to education and training[1]
. Clinical teachers combine their professional commitments with teaching activities within a real-life context to help students apply theory in practice and transform knowledge into skills[2]
. It is particularly important for clinical teachers to model and assess professional attitudes and behaviours that are critical for success in practice[3],[4]
.
Beyond experience and a positive attitude, good clinical teachers require additional knowledge and skills related to pedagogy. Most novice clinical teachers will simply imitate the great teachers they had in the past[5]
. While this is a strong foundation upon which to build, other skills are needed to teach student pharmacists — among the most important of these is an understanding of the use of learning objectives as a tool to optimise learning.
Learning objectives are a commonly used but frequently misunderstood tool. Almost all pharmacists are familiar with learning objectives – they are used in continuing education and university-based programmes, and are a requirement for self-assessment as part of continuing professional development (CPD) activities. In some cases the intent and value of learning objectives are not fully appreciated and they can be treated as a meaningless make-work project designed to slow down or frustrate spontaneous learning.
Two seminal reports by the Educational Testing Foundation in the United States outline the potential value and impact of learning objectives. These reports, published in 2007 and 2008, note that learning objectives work to improve student outcomes when teachers and students authentically engage with them and use them as a foundation for dialogue, curriculum planning, and assessment[6],[7]
. When learning objectives are treated (by either student or teacher) as burdensome and consequently ignored or merely tolerated, they will not work, regardless of how carefully crafted they may be[6],[7]
.
Using learning objectives in pharmacy training
Consider a complex, multifactorial concept such as managing a patient with diabetes. Although each patient and his or her circumstances are unique, there are general concepts that allow pharmacists to manage each situation. Experienced clinical teachers can support learners by presenting this complexity as a series of logically connected steps, each of which is manageable in its own right, sequenced in a manner that allows complexity to increase[8]
. This roadmap for building knowledge and skills should be laid out in its entirety, so both students and teachers understand the starting point, the end point, and the steps in between[9]
. Learning objectives provide a common vocabulary and approach for describing the steps in between[8],
[9]
.
For example, before students can feel confident and competent in managing any patient with diabetes, they need to understand the anatomy and physiology of the pancreas, the clinical biochemistry that informs blood tests, such as fasting blood glucose levels or HgA1C, and then the pharmacotherapeutics for addressing these issues. If one were to leap immediately to pharmacotherapeutics without first knowing and understanding the foundational material, the quality of learning, the ability to transfer learning to different situations and the ability to manage specific patient requirements is likely to be compromised.
Designing learning objectives
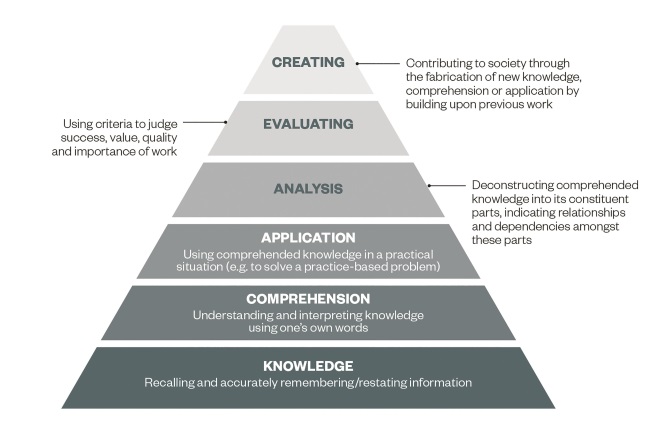
Bloom’s Taxonomy is the most common framework for developing learning objectives (see ‘Bloom’s Taxonomy: a structure for explaining learning’). The foundation of the pyramid is knowledge, followed by understanding. Each subsequent layer of the pyramid builds upon these foundations. Failure to adequately build these foundations leads to incomplete acquisition of knowledge and skills over time, which may result in performance problems, such as an inability to apply learning in new or different contexts or situations.
Bloom’s Taxonomy: a structure for explaining learning
Source: Image based on http://www.learningandteaching.info/learning/bloomtax.htm
The model illustrates that learning builds in a step-wise, progressive manner — each preceding stage is required to support more advanced forms of learning. Early levels representing knowledge acquisition and understanding provide the foundation for later levels related to application, evaluation, and creation of new knowledge.
Clinical teachers designing learning objectives use their experience to deconstruct and analyse how an individual develops from a novice to a competent and confident practitioner[10]
. Reflecting on and then articulating this process is a skill that can be developed[11]
. It is helpful to use the taxonomy as a starting point and think about each layer of the pyramid and what critical content is required at that level. See ‘Sample learning objectives for managing the care of a patient with diabetes’ for a sample series of questions and learning objectives that illustrate the process.
Box 1: Sample learning objectives for managing the care of a patient with diabetes
Goal: To be competent and confident in adjusting insulin doses based on blood glucose levels for patients with diabetes.
1. What do students need to know in order to achieve this goal?
Example: After the first four weeks of this rotation, students should be able to list common signs and symptoms of diabetes.
2. What do students need to comprehend in order to achieve this goal?
Example: At the end of this rotation, students should be able to describe the significance of laboratory test values (including fasting blood glucose and HgA1C) in establishing treatment goals for diabetes management.
3. What knowledge do students need to apply in order to achieve this goal?
Example: At the end of this rotation, students will be able to calculate appropriate modified insulin doses for patients without comorbidities, using clinical laboratory findings.
4. What do students need to analyse in order to achieve this goal?
Example: After the first week of this rotation, students should be able to appraise primary literature related to diabetes management using a systematic approach.
5. What do students need to evaluate in order to achieve this goal?
Example: At the end of this rotation, students will be able to predict and justify anticipated clinical outcomes associated with their insulin dose modification recommendations.
6. What do students need to create in order to achieve this goal?
Example: At the end of this rotation, students will be able to design patient-specific education and monitoring tools to support self-management of insulin dosing.
So-called SMART learning objectives are those which conform to a particular format[9],[10]
. Consistency in use of this format is helpful, because it enhances predictability for both students and teachers, and also facilitates design and use of learning objectives in practice[10]
(see ‘Examples of SMART learning objectives’). SMART is an acronym outlining key attributes of the most effective types of learning objectives.
‘Specific’ objectives provide clear and sufficient detail of the learning expectations. Vague terms such as ‘good’ or ‘appropriate’ may be difficult to assess and, similarly, overly-generalised learning objectives such as “manages care of patients with diabetes” are so broad as to be unhelpful. It is usually best to focus on a single activity or task within each learning objective. ‘Measurable’ objectives ensure that outcomes are observable by the teacher. The best learning objectives begin with action verbs (see ‘Verbs for writing learning objectives’ for sample verbs associated with each layer of the taxonomy). Some verbs, including ‘believes’, ‘thinks’ and ‘feels’, are not directly observable and are therefore of limited value in learning objectives.
Additionally, learning objectives should be tailored to the level of the student and the learning context and environment to ensure they are realistic and ‘achievable’. Goals should also be ‘relevant’, to ensure that both teachers and students understand their value in professional practice and therefore buy in to them — esoteric learning objectives that do not appear practical to learners will be overlooked or disregarded. ‘Timed’ objectives provide specific target dates and endpoints for attainment, as a way of building in accountability and ensuring learning – and teaching – are occurring as expected.
| Table 1: Examples of SMART learning objectives | ||
|---|---|---|
| SMART learning objective | Non-SMART learning objective | Rationale |
| Complete 25 medication reconciliations with patients aged over 65 years using ‘best possible medication history’ format by 30 September | Do medication reconciliation appropriately | Specific number, date and patient population identified to allow the student to remain on-track and on-task |
| Develop, justify and gain agreement from the medical team for pharmacy care plan recommendations for ten patients | Make good quality recommendations to enhance patient care | Without specifying what “quality” means, subjectivity and confusion will result. Quality here can be defined through justification and acknowledgement from the medical team |
| Review profiles and identify potential or actual drug therapy problems for all patients aged over 65 years receiving two or more drugs identified as potential risk using Beers Criteria during September | Ensure seniors are taking only safe drugs | Lack of specificity compromises quality of learning objective. The non-SMART objective is neither achievable, nor relevant |
| Table 2: Verbs for writing learning objectives | |
|---|---|
| Bloom’s Taxonomy level | Sample verbs |
| Knowledge | Define, list, recall, recognise, state, repeat, arrange, match, order, reproduce, replicate |
| Comprehension | Discuss, describe, explain, translate, restate, report, recognise, distinguish, estimate, indicate, select, sort |
| Application | Demonstrate, illustrate, perform, interpret, apply, employ, use, practice, prepare, modify, predict, extrapolate, manage, solve, choose |
| Analysis | Distinguish, differentiate, calculate, compare, contrast, categorise, appraise, relate, solve, examine, outline |
| Evaluation | Evaluate, assess, justify, appraise, argue, decide, criticise, defend, judge, predict, value |
| Creation | Make, propose, design, hypothesise, construct, invent, generate, synthesise, formulate, plan, compose |
Using learning objectives to guide assessment
Learning objectives can also provide a roadmap for evaluating students[12]
. Formative assessment provides students with low-judgement feedback focused on quality improvement and professional development rather than grades or ranking. Examples of formative assessment of learning objectives may include direct observation, reflective questioning, mock tests and hypothetical “what if?” discussions. Using learning objectives to guide formative assessment is both effective and fair: students should know upfront what is expected of them by simply reading the objectives, and teachers can use the targets as a way of structuring questioning, discussion and dialogue more efficiently.
Summative assessment is a more evaluative, judgmental form of evaluation, usually associated with a grade, a pass or fail decision, or ranking students in order of achievement. Examples of summative assessments include traditional tests and quizzes, objective structured clinical examinations (OSCEs) and research papers. In general, students should have frequent opportunities to receive formative assessment of their progress through learning objectives before having to perform in summative assessment. In this way, they can receive supportive feedback and coaching about areas for improvement and be better prepared for examinations.
SMART learning objectives should provide a roadmap for formative and summative assessment. For example, knowledge-level learning objectives related to ‘recalling’, ‘listing’ or ‘stating’ can be assessed using multiple choice or short-answer tests. Application-level learning objectives, such as ‘demonstrate’ or ‘perform’, are easily assessed using direct clinical observation, or OSCEs. Evaluation-level learning objectives, such as ‘defend’ or ‘appraise’, are best evaluated through debate or discussion. Any of these methods can be summative or formative, depending upon context and requirements.
Using learning objectives in practice
Tailoring a lesson or clinical rotation to make best use of learning objectives is important. Learning objectives are merely words on a page and require clinical teachers to bring them to life. Central to this process is the initial dialogue between teacher and student when the learning objectives are introduced, explaining how they will be used in the classroom or clinical setting[10]
. Helping students understand the logical progression of objectives and clarifying which assessment methods will be used is essential[10]
.
It is helpful to identify specific, recurrent times and dates for future discussions related to completing learning objectives, since this will foster accountability for learning and enhance predictability for students. During these discussions, using a variety of assessment techniques to check-in with students about their progress demonstrates the teacher’s commitment to the process and provides the student with assurance that their work is being recognised[9],[10]
. If students perceive that teachers are serious about using learning objectives, they will orient their behaviours accordingly[10],
[11]
. Identifying problems or misconceptions early in the process means they can be remedied through corrective feedback to prevent them being perpetuated in future learning. Showing genuine interest in the student’s development and illustrating how learning objectives are an important tool to foster professional development will build buy-in and engagement.
Learning objectives should reflect the strengths, needs and interests of teachers and students alike. More important than the written objectives themselves is the engagement between student and teacher that they produce: objectives will only work to support learning if they are used in an authentic manner and students and teachers commit to their use. When used in this way, they can provide a structure for teaching and learning, a platform for dialogue and discussion between teacher and student, and a roadmap for how to build knowledge, clinical skills and professional behaviours.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Woloschuk D & Raymond C. Development and evaluation of a workplace based preceptor training course for pharmacy practitioners. Can Pharm J 2012;145(5):231–236. doi: 10.3821/145.5.cpj231
[2] Kanji Z, Hamilton D & Hill D. Desirable traits of hospital pharmacy preceptors and residents. Can J Hosp Pharm 2000;53(5):352–354. doi: 10.4212/cjhp.v53i5.775
[3] Young S, Vos S, Cantrell M et al. Factors associated with students’ perception of preceptor excellence. Am J Pharm Educ 2015;78(3):53. doi: 10.5688/ajpe78353
[4] Sonthisomabat P. Pharmacy student and preceptor perceptions of preceptor teaching behaviours. Am J Pharm Educ 2008;72(5):110. PMCID: PMC2630135
[5] Kaviani N & Stillwell Y. An evaluative study of clinical preceptorship. Nurse Educ Today 2000;20:218–226. doi: 10.1054/nedt.1999.0386
[6] Millet C, Payne D, Dwyer C et al. A culture of evidence: an evidence-centred approach to accountability for student learning outcomes. Educational Testing Services: Princeton NJ; 2008. Available from: https://www.ets.org/Media/Education_Topics/pdf/COEIII_report.pdf (accessed January 2016).
[7] Educational Testing Service. A culture of evidence: critical features of assessments for postsecondary student learning. Princeton NJ; 2007. Available from: http://www.ets.org/Media/Resources_For/Higher_Education/pdf/4418_COEII.pdf (accessed January 2016).
[8] Shulman L. The wisdom of practice: essays on teaching, learning and learning to teach. Wiley: New York; 2004.
[9] Simon B & Taylor J. What is the value of course-specific learning goals? J College Sci Teach 2009; Nov/Dec:53–57. Available from: http://www.cwsei.ubc.ca/SEI_research/files/LifeSci/Simon_Taylor_ValueOfCourseSpecificLG.pdf (accessed January 2016).
[10] Eberly Centre for Teaching Excellence. The educational value of course-level learning objectives/outcomes. 2004. Available from: https://www.cmu.edu/teaching/resources/Teaching/CourseDesign/Objectives/CourseLearningObjectivesValue.pdf (accessed January 2016).
[11] Cuellar L & Ginsburg M. Preceptor’s Handbook for Pharmacists. American Society of Hospital Pharmacists: Bethesda MD; 2009.
[12] Whitman N & Schwenk T. Preceptors as teachers: a guide to clinical teaching. University of Utah School of Medicine: Salt Lake City UH; 1995.



