Illustration by Javier Trigo
Asthma and chronic obstructive pulmonary disease (COPD) are common conditions in the UK and inhaled medications are the cornerstone of their management[1]
. Good inhaler technique is essential to maximise the benefits of these medications and improve outcomes for the patient. This article considers the impact of sub-optimal inhaler technique and how healthcare professionals can support patients in optimising their technique.
The goal of asthma treatment is for patients to be symptom free and to be able to lead a normal, active life. More information on asthma, its diagnosis, treatment and management has been covered in previous articles[2]
,[3]
. The diagnosis, treatment and management of COPD has also been covered in previous articles[4]
,[5]
. In England and Wales, 45 million prescriptions for inhalers were issued in 2011 at a cost of around £900m[1]
.
If used correctly, inhalers deliver a smaller effective amount of the drug directly to the site of action in the lungs, with a faster onset of effect and with reduced systemic availability that minimises adverse effects (when compared with systemic administration). Despite this being the preferred method of medication delivery to the lungs, evidence suggests that many patients are unable to use their inhalers effectively[6]
. Although study results vary, estimates of inhaler errors include up to 90% of patients using pressurised metered dose inhalers (pMDIs)[6]
,[7]
,[8]
and up to 54% of patients using dry powder inhalers (DPIs)[6]
,[9]
. Inadequate inhaler technique lowers drug deposition to the lungs, wastes medication and may lead to poor disease control, reduced quality of life, increased emergency hospital admissions and higher treatment costs[10]
,[11]
. In 2014, the National Review of Asthma Deaths (NRAD) reported that misunderstanding and misuse of inhalers was thought to have contributed to a significant number of the 195 asthma deaths during 2012[12]
. According to the NRAD report, only 49% of patients reviewed in primary care had their inhaler technique checked in the year before their death[12]
. Furthermore, 17% of patients admitted to hospital (n=83) did not have documented evidence that their inhaler technique had been checked during their admission[12]
.
There is increasing evidence to suggest that correct inhaler technique plays an important role in improving medicine adherence[13]
,[14]
,[15]
, clinical outcomes[14]
,[15]
, quality of life[16]
and use of healthcare resources[14]
. The National Institute for Health and Care Excellence (NICE), England’s health technology assessment body, guideline for patients with COPD[17]
and the British Thoracic Society guideline for asthma[18]
, both recommend that prior to prescribing a new inhaler, the patient should receive training and education in the use of the device. Both sets of guidelines also advise that inhaler technique should be regularly assessed at each clinic visit[17]
,[18]
. However, recent data suggests that only 7% of healthcare professionals could demonstrate all the correct steps for using a MDI[19]
.
Correct technique depends on the inhaler type, therefore, patients need to understand the right steps for their own inhaler. It is a good idea for healthcare professionals to learn how to correctly use each inhaler device and to be aware of common errors so they can confidently demonstrate this to patients.
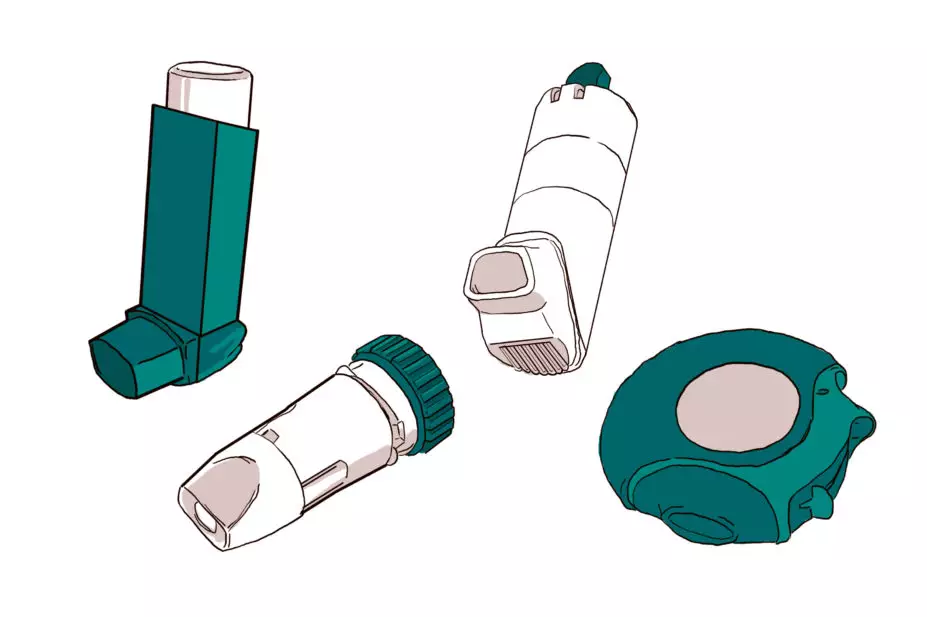
Types of inhaler device
Broadly speaking, there are two classes of inhaler devices[6]
: aerosols, which are either solutions containing medications or suspensions of solid particles in a gas, generated from devices (e.g. pMDIs or breath-actuated pMDI); and DPI delivery devices containing drugs in powdered formulation that have been milled to produce particles in the respirable range. DPI delivery devices allow the particles to be separated by the energy created by the patient’s own inspiratory flow, compared with the pMDI where the device itself generates the energy[20]
. For further information, see ‘Table 1: Advantages and disadvantages of the main inhaler types’. See Figures 1–5 for the range of devices currently available.
| Table 1: Advantages and disadvantages of main inhaler types | ||
|---|---|---|
| Reproduced with permission from[21] . | ||
| Advantages | Disadvantages | |
| Metered dose inhalers (MDIs) |
|
|
| MDI + holding chamber, reverse-flow spacer or spacer |
|
|
| Dry powder inhalers (DPI) |
|
|
What are the common problems with inhaler technique and what are their solutions?
Despite the development of several new types of inhaler device over the past 40 years, there has been no sustained improvement in how patients use them[6]
. Initiatives trying to improve patient use of inhalers have included: regular training programmes for patients and healthcare professionals; printed instructional material and videos; measures and devices to make inhalation easier (e.g. the development of a breath-actuated MDI and the attachment of a holding spacer to the MDI); and the design of various DPIs. However, a recent systematic review of inhaler technique concludes that incorrect inhaler technique is unacceptably frequent and has not improved over the past 40 years, indicating an urgent need for new approaches to education and drug delivery[6]
.
All types of inhaler devices have similar efficacy when tested under strict clinical trial conditions[22]
, however, in the real-life setting of clinical practice, a perfect inhaler does not exist; each has its advantages and limitations (see table 1). For the individual patient, inhalers should not be viewed as equivalent, and device type must become an important variable to consider when planning optimal treatment. Ensuring effective inhalation and drug delivery to the target site depends on many factors, which ultimately impact on patients’ response to treatment. In practice, the choice of inhaler device should not only take device-related aspects (e.g. aerosol velocity) into consideration, but also patient factors (e.g. inhalation flow, dexterity, cognition and preferences). With all inhaler types, error rates increase with age and the severity of airflow obstruction[23]
,[24]
.
Incorrect inhaler technique is common, regardless of the type of device prescribed. Patients may be given different inhaler types, receive minimal training (if any) and sometimes receive incorrect training on how to use the device. Therefore, it is important to understand the differences between these two types of inhalers, especially regarding how fast the patient inhales (inspiratory flow)[25]
,[26]
,[27]
. The concurrent use of multiple types of inhaler devices with different techniques can confuse patients. Ideally, patients should be prescribed one type of device or, failing that, all aerosols or dry-powder devices so that the same inhalation technique can be used.
Examples of common inhaler technique errors and recommendations for improvement are described in ‘Table 2: Common inhaler technique errors and suggested solutions’.
| Table 2: Common inhaler technique errors and suggested solutions | |
|---|---|
| Common error | Explanation and suggested solutions |
| Not shaking an aerosol inhaler device before use | Not shaking the canister properly may lead to inconsistent dosing and poorly functioning inhalers. Shake all inhalers; most dry powder inhalers (DPI) do not need shaking before use. |
| Not priming the aerosol inhaler device | Aerosol inhalers require priming (to check that the spray is functioning) before using for the first time, or if they have not been used for a while (usually five to seven days). |
| Not breathing out before inhaling | Breathing out fully (or as much as is comfortable) reduces the amount of air in the airways and increases the available space for air from the next breath. The result is a deeper than normal inhalation, maximising the opportunity to carry the drug to the site of action. |
| Incorrect positioning of inhaler device | Patients should be instructed not to hold a DPI with the mouthpiece pointing downwards during, or after loading, a dose, as the drug can escape. It should be kept horizontal or upright. The patient should keep their chin up or head slightly tilted back when using the inhaler. It should be placed correctly in the mouth and the lips should form a tight seal over the mouthpiece. |
| Incorrect coordination of pressured metered dose inhaler (pMDI) actuation with inspiration | To deliver the medication to the lungs from a pMDI, the patient must coordinate breathing in with pressing the canister. |
| Delay in inhaling drug through a holding spacer device (a device when combined with a pMDI helps to improve aerosol delivery) | The medication stays suspended in the spacer for a short time only, so if patients fail to take each dose without delay immediately after loading the spacer, a proportion of the dose is deposited on to the inner surface of the spacer and is therefore lost. |
| Incorrect inspiratory flow rate: breathing in either too fast or too slow | The total lung deposition of an inhaled drug is strongly affected by the speed of inhalation.
|
| Not holding your breath after inhalation | The ‘breath hold’ increases lung deposition through the process of sedimentation. By keeping the air still for a few seconds, a greater number of particles will sediment on to the receptor sites because of gravity. |
| Multiple actuations without waiting in between actuations | Very rapid actuations can reduce the dose delivered per actuation. |
| Using an empty inhaler | Patients frequently fail to detect when the inhaler is empty, particularly when using reliever aerosol devices. |
| Poor maintenance of inhaler or spacer device | Spacers should be reviewed every 6–12 months to check that the structure is intact (e.g. no cracks), the outer casing is clean and the valve is functioning. |
How can healthcare professionals talk to patients effectively about inhaler technique?
Training of patients by healthcare professionals has been shown to be an effective means of improving technique[28]
, but it needs to be repeated at intervals, and it is essential that those providing the training are themselves able to demonstrate the correct technique.
A recent study suggested that up to 25% of patients have not received any verbal instruction for the use of their prescribed inhaler[10]
. When given, instruction is often rushed, poor quality and not reinforced. Only an estimated 11% of patients receive follow-up assessment and education on their inhaler technique[29]
. Inhaler technique has been found to deteriorate over time (possibly after as little as two to three months)[30]
, so instruction needs to be repeated at regular intervals. In an Australian study, 75% patients using an inhaler for an average of two to three years reported that they were using their inhaler correctly but, on objective checking, only 10% demonstrated correct technique[31]
.
Figures 1–5 provide a summary of the techniques for the commonly used inhaler devices, and common errors with patient technique, that healthcare professionals can use as a guide before training patients.

Figure 1. How to use a metered dose inhaler (MDI)
Illustration by Javier Trigo
1: Cap should be removed and inhaler shaken to ensure consistent delivery of dose. Device should be primed if patient is using for the first time, or if not used for a while.
2: Patient should breathe out fully.
3: Patient should breathe in slowly and steadily and press down on the inhaler device.
4: On inhalation, the patient should hold their breath for a count of ten.
5: Patient should slowly breathe out, repeat dose (if applicable), and replace mouthpiece cover. Clean device if necessary after use.
Common errors in technique made by patients:
- Not shaking the aerosol inhaler before use
- Not priming the aerosol inhaler before first use
- Failing to detect an empty inhaler before use
- Failing to breathe out fully before inhaling
- Incorrect coordination of MDI and pMDI actuation with inspiration
- Incorrect inspiration flow rate (breathing in too fast or too slow)
- Failing to hold breath after inhalation
For solutions to these common errors, please see
table 2
.
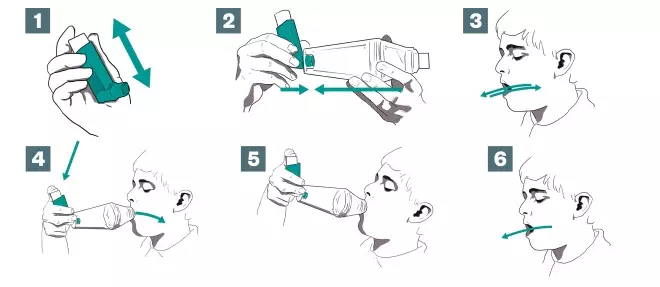
Figure 2. How to use a metered dose inhaler (MDI) with spacer
Illustration by Javier Trigo
1: Cap should be removed and the patient should check to see if the mouthpiece is clean. Inhaler should be shaken to ensure consistent delivery of dose. Device should be primed if patient is using for the first time, or if not used for a while.
2: The inhaler mouthpiece should be inserted into the end of the spacer device.
3: Patient should breathe in, and then breathe out fully.
4: The inhaler and spacer device should be held between the index finger and thumb. The spacer mouthpiece should be placed in the mouth, above the tongue. The patient should close their lips around the spacer device.
5: The patient should tilt their head back slightly toward the ceiling. The top of the inhaler device should be pressed to release a single dose of medicine. The patient should slowly breathe in all of the air and hold breath for ten seconds.
6: Patient should open mouth, remove spacer device and breathe out slowly. Patients could also use the tidal breathing technique, where they breathe slowly and steadily in and out four to five times.
Common errors in technique made by patients:
- Not shaking the aerosol inhaler before use
- Not priming the aerosol inhaler before first use
- Failing to detect an empty inhaler before use
- Failing to breathe out fully before inhaling
- Delay in inhaling drug through a holding spacer device
- Incorrect inspiration flow rate (breathing in too fast or too slow)
- Failing to hold breath after inhalation
- Poor maintenance of inhaler or spacer device
For solutions to these common errors, please see
table 2
.
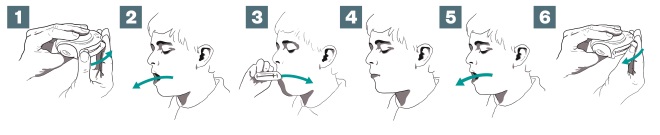
Figure 3: How to use an Accuhaler
Illustration by Javier Trigo
1: Holding the device horizontal or upright, the patient should open the inhaler by moving sliding lever in the correct direction.
2: Patient should breathe out fully but not into the Accuhaler.
3: Patient should place the inhaler device in the mouth, with the lips forming a tight seal over the mouthpiece, before breathing in quickly and deeply through the inhaler device.
4: On inhalation, the patient should hold their breath for a count of ten.
5: Patient should slowly breathe out.
6: Inhaler should be closed correctly by moving sliding lever in the correct direction. The inhaler should be cleaned as necessary.
Common errors in technique made by patients:
- Failing to breathe out fully before inhaling
- Incorrect positioning/holding of device
- Not breathing in quickly and deeply at the start of inhalation
- Failing to hold breath after inhalation
- Poor maintenance of inhaler
For solutions to these common errors, please see
table 2
.
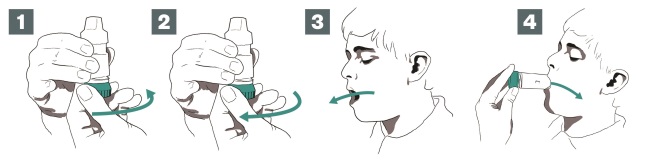
Figure 4: How to use a turbohaler
Source: Illustrations by Javier Trigo
1: The patient should unscrew the cap (turning anticlockwise) and remove. Holding the inhaler upright, the dose can be loaded by turning the coloured base to the right, as far as it will go.
2: Then twist it back to the left until it clicks. It is now loaded.
3: The patient should breathe out gently, away from the device. Holding the device without covering the air inlets, the tip of the mouthpiece should be placed between the lips and a good seal made.
4: The patient should breathe in quickly and deeply and hold their breath for 5–10 seconds. Remove the device before breathing out fully. Clean the device as necessary, replace the cap and screw it shut.
Common errors in technique made by patients:
- Incorrect positioning/holding of the device
- Incorrect inspiration flow rate (breathing in too fast or too slow)
- Poor maintenance of inhaler
For solutions to these common errors, please see
table 2
.
It is a good idea for healthcare professionals to learn how to correctly use each inhaler device (see additional resources for useful videos) and to be aware of common errors (see Table 2 and Figures 1–5), so they can confidently demonstrate this to patients. Healthcare professionals should also learn the rationale for each step of the instructions, so they can clearly explain its importance to patients during counselling (see ‘Box 1: How to engage with patients to confirm inhaler technique’ and ’Box 2: Inhaler technique checklist’).
Box 1: How to engage with patients to confirm inhaler technique
- Introduce yourself to the patient;
- Ask the patient if you can discuss their inhaler treatment with them. Do not ask “Can you use your inhaler?” It is better to say “Can you show me how you use your inhaler so that we can see if we can improve the amount of medicine getting into your lungs?” Do not rely on the patient’s assurance that they know how to use their inhaler; most are unaware that their inhaler technique could be improved;
- It is worth understanding what the patient knows about their lung condition. Educating patients in correct inhaler use may also improve adherence to their treatments;
- Discuss the inhaler with the patient, explaining what medicine it contains and how it should help their lung condition;
- Describe the steps of using the inhaler device (see Box 2 and Figures 1-5);
- Once you have described the steps, show the patient how to do it yourself;
- After you have demonstrated the optimal technique, ask the patient to show you how they would use the inhaler. Check they are doing it correctly and, if needed, explain how they can improve their technique. Non-availability of ample placebo devices can be a barrier to effective education. If a patient has their own inhalers, then an extra dose of these could be given if it is thought unlikely to cause undue harm;
- Ensure the patient knows how to keep their inhaler clean and in good working order. As every inhaler is different, ask the person to follow the manufacturer’s instructions. Also, make sure your patient knows how to recognise that their inhaler is empty or nearly empty;
- Ask the patient if they have any questions or concerns about their medicine and the steps to optimise the delivery to their lungs;
- Repeat instruction regularly. Inhaler technique must be rechecked and education must be regularly reinforced in order to maintain optimal drug delivery.
Box 2: Inhaler technique reminder checklist
- Prepare the device (e.g. remove the mouthpiece cover, open the device, hold the inhaler upright).
- Prepare the dose (e.g. shake all aerosols and load dose for DPIs).
- Breathe out gently as far as is comfortable (not into inhalers).
- Put the mouthpiece in the mouth and close the lips around it.
- Breathe in:
- Check co-ordination of breathing and actuation of MDI
- Think about the type of inhaler device – is it an aerosol device or DPI?
- Breathe in slowly and steadily for all aerosol devices (including through a spacer device).
- Breathe in quickly and deeply for all DPIs
- Remove inhaler from the mouth and hold breath for ten seconds
- Repeat dose (if applicable), replace mouthpiece cover or close device.
Additional resources:
- The Greater Manchester Inhaler Technique Improvement Innovation Project, part of Wessex Academic Health Science Network, has produced a number of videos and podcasts on inhaler technique and how to use specific devices, including:
- Asthma UK has also produced guidance on inhaler technique for patients, as well as a number of videos on inhaler technique and how to use specific devices, including:
- Using your inhalers
- Metered Dose Inhaler
- Autohaler
- Accuhaler
- Peak Flow Meter
- EasiBreathe Inhaler
- Easyhaler
- Turbohaler
- Small Volume Spacer
- Small Volume Spacer (with a child)
- Large Volume Spacer (single breath)
- Large Volume Spacer (multi-breath)
- Large Volume Spacer (with a mask)
- Large Volume Spacer (with a child)
Anna Murphy is consultant respiratory pharmacist, University Hospitals of Leicester NHS Trust and honorary visiting professor, De Montfort school of pharmacy, Leicester.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Health and Social Care Information Centre. Prescriptions dispensed in the Community. England 2003–2013. Health and Social Care Information Centre, London: 2014. Available at: http://www.hscic.gov.uk/searchcatalogue?productid=14988&q=title%3a%22Prescriptions+Dispensed+in+the+Community%22&sort=Relevance&size=10&page=1#top (accessed July 2016).
[2] Murphy A. Asthma: the condition and its diagnosis. Clinical Pharmacist 2010;2:203. Available at: http://www.pharmaceutical-journal.com/learning/learning-article/asthma-the-condition-and-its-diagnosis/11012933.article (accessed July 2016).
[3] Murphy A. Asthma: treatment and monitoring. Clinical Pharmacist 2010;2:209. Available at: http://www.pharmaceutical-journal.com/learning/learning-article/asthma-treatment-and-monitoring/11012934.article (accessed July 2016).
[4] Khachi H, Barnes N, Antoniou S. COPD: clinical features and diagnosis. Clinical Pharmacist 2010;2:382. Available at: http://www.pharmaceutical-journal.com/learning/learning-article/copd-clinical-features-and-diagnosis/11049454.article (accessed July 2016).
[5] Khachi H, Barnes N, Antoniou S. COPD: management. Clinical Pharmacist 2010;2:390. Available at: http://www.pharmaceutical-journal.com/learning/learning-article/copd-management/11049455.article (accessed July 2016).
[6] Sanchis J, Gich I & Pefersen S. Systematic review of errors in inhaler use: has patient technique improved over time? Chest 2016;128(5):3198–3204. doi: 10.1016/j.chest.2016.03.041
[7] Hardwell A, Barber V, Hargadon T et al. Technique training does not improve the ability of most patients to use pressurised metered-dose inhalers (pMDIs). Prim Care Respir J. 2011;20(1):92–96. doi: 10.4104/pcrj.2010.00088
[8] Plaza V & Sanchis J. Medical personnel and patient skill in the use of metered dose inhalers: a multicentric study. CESEA Group. Respiration 1998;65:195–198. doi: 10.1159/000029259
[9] Crompton GK, Barnes PJ, Broeders M et al. The need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement Team. Respir Med 2006;100(9):1479–1494. doi: 10.1016/j.rmed.2006.01.008
[10] Lavorini F, Magnan A, Dubus JC et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med 2008;102:593–604. doi: 10.1016/j.rmed.2007.11.003
[11] Giraud V & Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J 2002;19:246–251. doi: 10.1183/09031936.02.00218402
[12] Office for National Statistics. Deaths registered in England and Wales: 2014. Available at: http://www.ons.gov.uk/ons/rel/vsob1/death-reg-sum-tables/2014/rft-deaths-summary-tables-2014.xls (accessed July 2016).
[13] Darba J, Ramirez G, Sicras A et al. Identification of factors involved in medication compliance: incorrect inhaler technique of asthma treatment leads to poor compliance. Patient preference and Adherence 2016;10:135–145. doi: 10.2147/ppa.s95303
[14] Price D, Roche N, Christian Virchow J et al. Device type and real-world effectiveness of asthma combination therapy: an observational study. Respir Med 2011;105:1457–1466. doi: 10.1016/j.rmed.2011.04.010
[15] Giraud V, Allaert FA & Roche N. Inhaler technique and asthma: feasibility and acceptability of training by pharmacists. Respir Med 2011;105:1815–1822. doi: 10.1016/j.rmed.2011.07.004
[16] Goris S, Tasci S & Elmali F. The effects of inhaler technique and quality of life in COPD patients. J Aerosol Med Pulm Drug Deliv 2013;26(6):336–344. doi: 10.1089/jamp.2012.1017
[17] The National Institute for Health and Care Excellence guideline [CG101]. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care 2010. Available at: http://www.nice.org.uk/guidance/CG101/ (accessed July 2016).
[18] British Thoracic Society/Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. Clinical guideline 141. October 2014. Available at: https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2014/ (accessed July 2016).
[19] Baverstock M, Woodhall N & Maarman V. Do healthcare professionals have sufficient knowledge of inhaler techniques in order to educate their patients effectively in their use? Thorax 2010;65:A117. doi: 10.1136/thx.2010.150979.45
[20] Lavorini F. The challenge of delivering therapeutic aerosols to asthma patients. Allergy 2013;102418. doi: 10.1155/2013/102418
[21] Dolovich MB, Ahrens RC, Hess DR et al. Device Selection and Outcomes of Aerosol Therapy: Evidence-Based Guidelines American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest 2005;127(1):335-371. doi: 10.1378/chest.127.1.335
[22] Geller DE. Comparing clinical features of the nebulizer, metered-dose inhaler, and dry powder inhaler. Respir Care 2005;50(10):1313–1322. PMID: 16185367
[23] Melani AS, Bonavia M, Cilenti V et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011;105:930–938. doi: 10.1016/j.rmed.2011.01.005
[24] Barrons R, Wheeler J & Woods JA. Review: opportunities for inhaler device selection in elderly patients with asthma or COPD. Journal of Patient Intelligence 2015;7:53–65. doi: 10.2147/pi.s61200
[25] Al-Showair RA, Tarsin WY, Assi KH et al. Can all patients with COPD use the correct inhalation flow with all inhalers and does training help? Respir Med 2007;101(11):2395–2401. doi: 10.1016/j.rmed.2007.06.008
[26] Al-Showair RA, Pearson SB & Chrystyn H. The potential of a 2Tone Trainer to help patients use their metered-dose inhalers. Chest 2007;131(6):1776–1782. doi: 10.1378/chest.06-2765
[27] Borgstrom L, Bondesson E, Moren F et al. Lung deposition of budesonide inhaled via Turbuhaler: a comparison with terbutaline sulphate in normal subjects. Eur Respir J 1994;7(1):69–73. doi: 10.1183/090319 36.94.07010069
[28] Price D, Bosnic-Anticevich S & Briggs A. Inhaler competence in asthma: common errors, barriers to use and recommended solutions. Respiratory Medicine 2013;107:37–46. doi: 10.1016/j.rmed.2012.09.017
[29] Melani AS, Zanchetta D, Barbato N et al. Inhalation technique and variables associated with misuse of conventional metered-dose inhalers and newer dry powder inhalers in experienced adults. Ann Allergy Asthma Immunol 2004;93:439–446. doi: 10.1016/s1081-1206(10)61410-x
[30] Ovchinikova L, Smith L & Bosnic-Anticevich S. Inhaler technique maintenance: gaining an understanding from the patient’s perspective. J Asthma 2011;48:616–624. doi: 10.3109/02770903.2011.580032
[31] Basheti IA, Armour CL, Bosnic-Anticevich SZ et al. Evaluation of a novel educational strategy, including inhaler based reminder labels, to improve asthma inhaler technique. Patient Educ Couns 2008;72:26–33. doi: 10.1016/j.pec.2008.01.014